Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research - (2023)Volume 14, Issue 4
Alginate dressings play a positive role in wound care; however, controversial findings have been reported. We conducted this meta-analysis to systematically evaluate the efficacy of alginate dressings for wound care in patients. PubMed, Embase, Cochrane Library, Web of Science, Wanfang Data, and China National Knowledge Infrastructure (CNKI) were searched for relevant studies. The Q test and I2 statistic were used to examine the between-study heterogeneity. Fixed-or random-effects models were selected based on the study heterogeneity. Sensitivity analyses, funnel plots, and Begg’s tests were performed. Overall, 20 articles involving 54 trials were included in the analysis. Compared to other traditional wound dressings, our analyses revealed that alginate dressings played a positive role in shortening wound healing time (Weighted Mean Difference (WMD)=-8.04; 95% Confidence Interval (CI): -11.51 to-4.57; I2=98.3%), reducing pain (WMD=-0.96; 95% CI: -1.29 to-0.64; I2=90.1%), and reducing the frequency of dressing change (WMD=-6.75; 95% CI: -8.97 to-4.52; I2=97.1%). These findings suggest that alginate dressings could become a widely utilized and effective tool in clinical practice for improving patients' quality of life and lowering the healthcare burden of wound management. This provides an essential basis for reference in clinical wound care.
Alginate dressings; Wound care; Randomised controlled trials
‘Wound’ refers to the destruction of skin tissue integrity, often accompanied by a lack of organic matter. According to a British survey, three to four persons were found to have one or more wounds per 1000 population [1]. Approximately 1-2 million people in Europe are affected by wounds [2]. Chronic wound problems affect more than 6.5 million people in the USA [3]. Wounds bring general distress and cause a serious burden to the life of patients. The bleeding caused by wounds, malodour caused by infection, pain, and the economic burden caused by frequent dressing changes are related to a reduction in patients' quality of life [4,5]. Moreover, the social stigma associated with wounds greatly increases the psychological burden on patients [6]. Wounds not only inconvenience patients, but also bring great challenges to the healthcare system.
A moist environment may provide optimal conditions for the cells involved in the healing process and allow autolytic debridement, which is thought to be an important part of the healing pathway [7]. Alginate dressings contain sodium, or sodium with calcium and alginate salts. These salts are highly hydrophilic and can absorb large amounts of wound exudate, providing a moist environment for wound healing [8]. Owing to these characteristics, alginate dressings are widely used in clinical practice for the treatment and care of various acute and chronic wounds [7-9]. The efficacy of alginate dressings should be evaluated for wound care in patients.
Numerous studies have evaluated the role of alginate dressings in promoting wound healing; some Randomised Controlled Trials (RCTs) suggest that the use of alginate dressings have a positive effect on the healing of wounds and alleviate pain [10-24], while some contrastingly reported that alginate dressings did not have a positive effect on promoting wound healing [25-28]. Moreover, a review of previous evidence on the use of wound dressings as a treatment method for different types of wounds revealed no evidence to support the selection of specific dressings. Three systematic reviews of RCTs have reported on the treatment of ulcers (including pressure ulcers, diabetic ulcers, and lower-limb venous ulcers), which suggest that alginate dressings have no effect on promoting wound healing [7-9]. Owing to the limited sample size, single wound types, and poor literature quality involved in these studies, we are not completely convinced that alginate dressings are ineffective in promoting wound healing. Moreover, no systematic review has investigated wound dressings as a treatment method for different types of wounds to support the selection of specific dressings. Therefore, this meta-analysis aimed to investigate the role of alginate dressings in wound healing and reached conclusions contrary to the aforementioned studies, to provide a reference for clinical wound care.
Systematic review eligibility criteria
The Cochrane Handbook was followed in this study [29]. A systematic review was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [30]. The review protocol was registered on PROSPERO under the registration number CRD42023405021 (https://www.crd.york.ac.uk/PROSPERO/), no amendments were made to the information provided at registration. This study was based on the planned Participants, Intervention, Control, Outcome, and Study design (PICOS) elements outlined in (Table 1).
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Participants | Patients with wounds provoked by various causes (e.g., burns, surgery, body surface ulcers, infection etc.). | Patients with deep burns (degrees III and IV), sinus patient’s treatment for bone wounds, pre-operation preparation, patients using biological tissue synthesis substitutes, and patients with autologous skin cultured transplants. |
| Intervention | Alginate dressings, including sodium alginate, calcium alginate and silver alginate dressings. | Alginate dressings is used as a non-wound dressing such as an in vivo drug release carrier, contact lens, tissue filling material, medical sensor, etc. |
| Control | Any other dressing, treatment, placebo, or blank control. | Comparison of functions before and after using Alginate dressings, Alginate dressings combined with other treatments. |
| Outcomes | Primary outcome: Time to complete wound healing, pain, and number of dressings changes; Secondary outcome: Cost, inflammatory reaction, adverse reactions, and cure rate. | Long-term follow-up results, such as quality of life. |
| Type of study | RCTs | Review, case study, mechanism study, research and development, preparation and storage of materials, animal experiment, marketing strategy, editorials, news, and registered clinical trials with unfinished/unreported results. |
Table 1: Inclusion and exclusion criteria.
Search strategy
From inception to 25 June 2023, we searched the following online databases: PubMed, Cochrane Library (CENTRAL), Embase, Web of Science, China National Knowledge Infrastructure (CNKI), and Wanfang Database (WFDATA). The search terms (‘Wounds’ or ‘Diabetic foot ulcer’ or ‘Leg ulcers’ or ‘Pressure ulcers’ or ‘Traumatic’ or ‘Postoperative wounds’) and (‘Alginate dressings’ or ‘Sodium alginate’ or ‘Calcium alginate’ or ‘Alginate silver’) were used for subject-word and free-word retrieval.
The search strategy was developed and implemented under the guidance of experts in library services from Shandong First Medical University. Unpublished studies and conference materials were manually searched and references in the included literature were tracked. No language restrictions were imposed.
Study selection
Screening was performed by two reviewers who independently examined the titles and abstracts, followed by a full-text evaluation. When the two researchers' perspectives diverged, they conferred and discussed with a third researcher before making a decision. According to the principles of PICOS (Table 1), articles were considered for inclusion if they included the following: (1) Patients with acute and chronic wounds; (2) treatment with alginate dressing; (3) any other dressing, treatment, placebo, or blank as control; (4) primary outcome of interest was the time to complete wound healing, pain, or number of dressing changes; and (5) RCT design.
Data extraction and quality evaluation
Data were extracted independently by three researchers for each included RCT using a standard data collection sheet. The following data were extracted: First author, publication year, sample size, wound type, dressing in the intervention and control groups, outcome, and main effect value. The Cochrane Risk of Bias (RoB) tool was used to assess the quality of the included studies. The risk-of-bias assessment was independently conducted by two researchers. In cases of disagreement, another author was consulted for discussion and decision-making.
Statistical analysis
All statistical analyses were performed using stata, version 12.0 (Stata Corp, College Station, TX, USA). The Weighted Mean Difference (WMD) with its corresponding 95% Confidence Interval (CI) was used as the pooled effect size for continuous data. Heterogeneity among the included studies was tested using the Q test and I2 statistic. When P>0.1 and I2<50%, a fixedeffects model was used as the pooling method; otherwise, a random-effects model was adopted. Sub-group analysis was conducted to explore the possible sources of inter-study heterogeneity based on publication year, country, wound type, dressing of the control group, and intervention time. To evaluate the consistency of the meta-analysis results, sensitivity analyses were performed to assess the impact of each individual study on the pooled effect estimates. Publication bias was assessed using funnel plots and Begg’s tests. All tests were bilateral, and P<0.05 was considered statistically significant.
Study selection and characteristics
Figure 1 shows the process flowchart for the literature search and study selection. Overall, 366 potentially relevant articles were identified in the six electronic databases, with 85 duplicate articles. Forty-four articles were selected for full-text review after title and abstract screening. Five additional articles were identified during manual screening. A further 29 articles were excluded because they did not meet the inclusion criteria. Ultimately, 20 articles met the inclusion criteria.
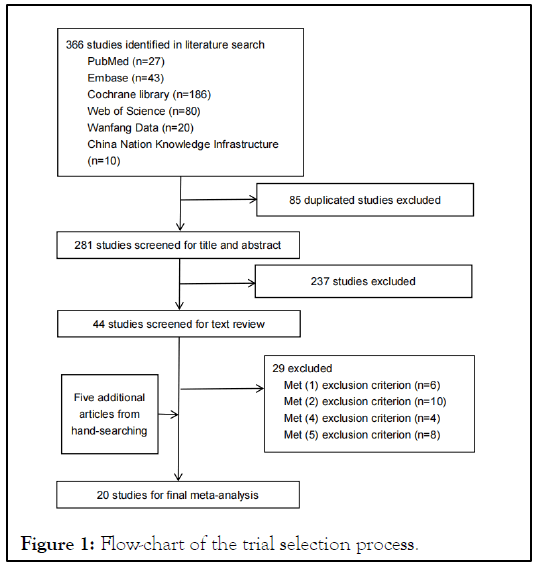
Figure 1: Flow-chart of the trial selection process.
The characteristics and methodological quality evaluation results of the included studies are presented. Among them, 16 articles were from developing countries [10-14,16,18-24,27,31,32] and 4 from developed countries [17,25,26,28]. There were 11 papers published in 2020 or later [10,12-14,16,18,19,21,24,25,31] and 9 were published before 2020 [11,17,20,22,23,26-28,32]. Six studies reported patients with post-operative wounds [12-14,17,25,28] three reported infected wounds [10,24,27] four reported diabetic ulcers [19,21,26] three reported pressure ulcers [16,22,31] two reported burns [11,32] and two reported bites [18,23]. Since there were many types of wounds, we classified them into three groups: Post-operative, chronic (including infected wounds, diabetic foot ulcers, and pressure ulcers), and acute (including burns and bites). The types of treatment administered to the control group were not restricted. The control treatme
nt was divided into two categories: Traditional drug therapy (Drugs commonly used in clinical wounds, such as biogels and antibacterial gels) [10,11,22] and traditional dressing therapy (Dressings commonly used in clinical wounds, such as saline gauze and iodophor gauze) [12-14,16-21,23-28,31,32]. In the analysis of healing time and pain, the study by Li, et al. [12], divided surgical wound into class I, II and III according to wound types, and marked them as group 1, 2, 3. Type I incision operation: Clean surgical incision, also known as sterile incision, the surgical site does not have bacterial infection, the most common is thyroid surgery and breast, inguinal hernia and other operations, through local skin disinfection on the body surface, one can basically meet the aseptic requirements; type II incision operation: Contaminated incision, incision may produce contamination, commonly seen in abdominal surgery, such as gastrointestinal surgery, biliary surgery, pancreatic surgery, etc; type III incision operation: The incision of contaminated surgery, generally abscess or infection disease, most of the incision and drainage, so that the purulent secretion in time to empty, faster control of infection, such as suppurative appendicitis, abscess incision, intestinal perforation, acute obstructive suppurative cholangitis surgery wound, respectively. When analysing pain, according to the intervention duration (1-3 days, 4-7 days, and ≥ 8 days), the studies by Chen, et al. [10],Cheng, et al. [11], Zhu [16], Mamalodis, et al. [25] and Zhang, et al. [31] were grouped and labelled as ‘a’, ‘b’, and ‘c’, respectively. Therefore, 21 articles with 54 experiments were included in this study. Quality evaluation of the included studies was performed at Level B. In all studies, the patients’ basic characteristics were comparable between the intervention and control groups (P>0.05).
Primary outcome
Healing time: Fourteen study groups of 12 RCTs with a total of 860 patients showed that the wound healing time in the alginate dressing group was significantly shorter than that in the control group (P<0.01; WMD=-8.04; 95% CI:-11.51 to-4.57; I2=98.3%) (Figure 2). Sub-group analyses for healing time were performed by year of publication, country, wound type, and dressing type; the results of the sub-group analyses. According to the year of publication, 3 studies published before 2020 showed that alginate dressing had no obvious effect on shortening wound healing time (P=0.121; WMD=-0.028; 95% CI:-20.029 to 19.973; I2=61.3%) [11,20,26], whereas 11 studies published after 2020 showed otherwise (P<0.01; WMD=-8.688; 95% CI:-12.249 to-5.127; I2=98.5%) [10,12-14,16,18,19,21,25]. By sub-group analysis of country types, 2 studies from developed countries showed that alginate dressings had no effect on promoting wound healing (P=0.998; WMD=-0.028; CI:-20.029 to 19.973; I2=61.3%) [25,26], while 11 studies from developing countries found that alginate dressings had a positive effect (P<0.01; WMD=-8.688; 95% CI:-12.249 to-5.127; I2=98.5%) [10-14,16,18-21]. Sub-group analysis of wound types showed that alginate dressings played an active role in shortening the healing time of acute (P=0.022; WMD=-9.607; 95% CI:-17.843 to-1.370; I2=92.9%) [11,18] chronic (P<0.001; WMD=-11.433; 95% CI:-15.823 to-7.042; I2=97.6%) [10,16,19,21], and post-operative (P=0.002; WMD=-3.918; 95% CI:-6.395 to-1.442; I2=85.6%) wounds [12-14]. In term of types of dressings in the control group, the results showed that alginate dressings had more advantages in promoting wound healing than traditional drugs did [11], (P=0.018, WMD=-5.140; 95% CI:-9.385 to-0.895) and dressings (P<0.001; WMD=-8.264; 95% CI:-11.871 to-4.656; I2=98.4%) [10,12-14,16,18-21,25,26]. These results indicated that the year of publication, country, wound type, and dressing type were the main sources of heterogeneity.
Figure 2: Random effects of meta-analysis of healing time of
alginate dressings for wound. Note: Type I incision operation;
type II incision operation; type III incision operation, CI:
Confidence Interval; WMD: Weighted Mean Difference.
Here  I-squared=98.3%.
I-squared=98.3%.
Pain
Twenty study groups of 10 RCTs with a total of 1298 patients showed that the degree of pain in the alginate dressing group was significantly better than that in the control group (P<0.001; WMD=-0.96; 95% CI:-1.29 to-0.64; I2=90.1%) (Figure 3). Subgroup analyses according to year of publication, country, wound type, dressing type, and intervention days were performed for pain. The differences across sub-groups were statistically significant for the year of publication, country, wound type, dressing type, and intervention duration. In addition, alginate dressings were more effective in reducing wound pain in subgroups by year of publication and dressing type than in the controls. However, in the other sub-groups, no statistically significant results were found for alginate dressings, such as in the developed country, acute trauma, and 1-3 days intervention sub-groups.
Figure 3: Random effects of meta-analysis of pain of alginate
dressings for wound. Note: Type I incision operation; type II
incision operation; type III incision operation; a: 1-3 day; b:
4-7 day; c: ≥ 8 day. Here  I-squared=
90.1%.
I-squared=
90.1%.
Dressing change frequency
Eight RCTs with a total of 643 patients showed that dressing changes in the alginate dressing group were significantly fewer than those in the control group (P<0.001; WMD=-6.75; 95% CI:-8.97 to-4.52; I2=97.1%). Figure 4 shows the results of the detailed sub-group analysis for dressing change frequency. The differences across sub-groups were statistically significant for the year of publication, country, wound type, and dressing type. However, sub-group analyses showed that alginate dressing changes were fewer compared to controls in all subgroups, except for the different degrees of dressing changes.
Figure 4: Random effects of meta-analysis of dressing change
frequency of alginate dressings for wound. Note:  97.1%.
97.1%.
Secondary outcomes
Secondary outcome indicators included costs, inflammatory reactions, and adverse reactions. Owing to the diverse evaluation methods, a qualitative systematic review was conducted to summarise the secondary outcomes (Table 2). Two studies have shown that the use of alginate dressings effectively reduced dressing changes and hospitalisation costs [17,22]. Five studies from China suggested that alginate dressings could effectively reduce wound infections [10-12,23,24]. Four studies showed that alginate dressings reduced the incidence of wound infection and another showed that alginate dressings reduced the infection rate of type II and III incisions [12]. Lu suggested that alginate dressings could effectively reduce the rate of infection recurrence [10,11,23,24]. Two studies indicated that alginate dressings could effectively reduce scar hyperplasia and one study by Chen, et al [10] indicated that alginate dressings could reduce the incidence of adverse events [11,14].
| Reference | year | Outcome | Effect value | Main conclusion |
|---|---|---|---|---|
| Cost | ||||
| [27] | 2017 | Total cost during hospital stay | The average cost of the experimental group was 2647.82 US dollars, while the average cost of the control group was 3308.83 US dollars | No statistically significant difference between the alginate dressing and the control group |
| [22] | 2013 | Cost of treatment | The average cost of the experimental group was 377.17 US dollars, while the average cost of the control group was 467.74 US dollars | Cost of the experimental group was significantly lower than that of the control group |
| [17] | 2016 | Total cost per dressing per day | The experimental group spent $12.94 per day, while the control group spent an average of $11.54 per day. | Cost of the control group was significantly lower than that of the experimental group |
| Inflammatory reaction | ||||
| [11] | 2019 | Inflammatory reaction on the wound surface (with redness and swelling) | The occurrence rate of wound inflammation reaction in the experimental group was 6.67%, lower than 46.67% in the control group. | Incidence of wound inflammatory reaction in the experimental group was significantly lower than that in the control group |
| [12] | 2021 | Incision infection rate (refer to the "Diagnostic Standards for Hospital Infection in China") | The infection rates of both groups were 0 in type I incision, and the infection rates of type II and type III incision experimental groups were 14.3% and 34.2%, respectively. The infection rates in the control group were 85.7% and 68.4%, respectively. | There was no significant difference for type I incision between the two groups; the infection rate of the control group with type II and type III incision was significantly higher than that of the observation group |
| [10] | 2022 | Infection control time | The infection control time in the experimental group was 5.12 ± 1.56 days, and that in the control group was 7.34 ± 2.3 2 days. | Infection time of the experimental group was lower than that of the experimental group |
| [23] | 2019 | Wound secretion | 24% of patients in the experimental group had a decrease in secretion, while 15% of patients in the control group had a decrease in secretion. | Infection time of the experimental group was lower than that of the experimental group |
| [24] | 2020 | Incision infection control time and reinfection rate | The wound infection control time in the experimental group was 3.8 ± 0.6 days, while the wound control time in the control group was 5.6 ± 1.9 days. The recurrent infection rate in the experimental group was 0, while the recurrent infection rate in the control group was less than 2%. | Infection time of the experimental group was lower than that of the experimental group; and the recurrent infection rate in the experimental group was significantly lower than that in the control group |
| Adverse reactions | ||||
| [10] | 2022 | Occurrence of adverse reactions | The incidence of adverse reactions was 4.66% in the observation group and 27.9% in the experimental group. | The incidence of adverse reactions in the experimental group was significantly lower than that in the control group |
| [28] | 2015 | Overall 30‐day wound complication incidence | The incidence of adverse reactions within 30 days in both the experimental and control groups was 30%. | The silver-eluting alginate dressing showed no effect on wound complication incidence |
| [11] | 2019 | Scar hyperplasia | The experimental group (VSS score 3.73 ± 1.91) was lighter than the control group (VSS score 5.67 ± 2.09). | Scar hyperplasia in the experimental group was better than that in the control group |
| [14] | 2022 | Scar hyperplasia | The experimental group had a VSS score of 6.31 ± 1.24 before intervention and 3.05 ± 1.19 after intervention; The control group had a VSS score of 6.27 ± 1.26 before intervention, and 4.56 ± 1.02 after intervention. | Scar formation in the experimental group was significantly better than that in the control group |
Table 2: Main conclusions of the studies assessing the secondary outcomes.
Sensitivity analysis and publication bias detection
In the sensitivity analysis, no individual study substantially influenced the pooled WMDs for wound healing time, pain score, or dressing change frequency. The funnel plots used to assess publication bias. Their shapes are roughly symmetrical. No publication bias was detected using the Begg’s test for healing time (P=0.827), pain (P=0.626), or dressing change frequency (P=0.902).
To the best of our knowledge, this is the first systematic review and meta-analysis to evaluate the effect of alginate dressings in promoting multiple types of wound healing using RCTs involving alginate dressings for wound care. Our study included 21 articles with 54 RCTs and 1790 cases. The results of this study suggest that the use of alginate dressings may shorten wound healing time, relieve wound pain, and reduce the number of dressing changes.
In the analysis of the therapeutic effect, our study suggests that alginate dressing can effectively shorten wound healing time and promote wound healing. These results are consistent with those of nine clinical trials [10-14,16,18-21,25,26]. However, some studies have suggested that alginate dressings are not more effective in the treatment of wounds compared to the control. This lack of effectiveness may be because the sample sizes of these studies were small and the intervention times were short. According to the results of the sub-group analysis, the year and country of publication may have been the source of heterogeneity in this study. This may be related to increasing progress in medical and health conditions in recent years. In addition, one study by Thomas, et al. [33] suggested that wound healing is related to race, and people of African and Asian ancestry typically have longer wound healing times and are prone to scar formation, which are related to individual genes and the incomplete penetrance of non-Mendelian autosomal dominant inheritance [33].
Our results indicate that alginate dressings can effectively reduce wound pain, which is consistent with the results of 12 previous studies [10-17]. However, some studies indicated that alginate dressings do not significantly reduce wound pain [10,11,15,16,25]. One study showed that a humid wound environment is more conducive to autolysis and debridement, pain reduction, scar reduction, and the activation of collagen synthesis [34]. Alginate, a natural linear polysaccharide, has good bio-compatibility and liquid absorption ability, and can provide a wet environment for wound healing [31]. Our subgroup analysis showed that the country in which the study was conducted, the type of wound, and the number of intervention days may be sources of heterogeneity. Pain is a subjective sensation described as a complex paradigm that includes three dimensions: Sensory discrimination, emotional movement, and cognitive assessment. Pain cannot be directly measured and can only be determined by the person experiencing it [35]. Therefore, racial and individual differences may result in variations in pain tolerance. One study by Langemo, et al. [36] indicated that tissue damage may lead to hyperalgesia and active abnormal pain near, the damaged site. Therefore, patients may experience greater pain than expected during wound cleaning and dressing changes. At the same time, inflammation is a major cause of chronic wound pain. Tissue ischaemia stimulates the release of endogenous chemicals, thereby increasing pain allergy [33,37]. In addition, the release of inflammatory mediators can also increase pain [35,36]. The feeling of pain in patients with chronic wounds may be stronger than that in patients with acute wounds. Therefore, the degree of pain relief in patients with chronic wounds may be stronger than that in patients with acute wounds after using alginate dressings. In addition, the sub-group results of intervention days showed that the analgesic effect of alginate was more pronounced after 3 days of use, which implies that the failure of the dressing to exert its effect might be due to the short intervention times of less than three days.
Eight of the included articles considered that the use of alginate dressings was effective in reducing the number of dressing changes [10,13,14,16,18-20,32]. This may be because alginate dressings can absorb exudates well; thus reducing the frequency of dressing changes.
Regarding secondary outcomes, studies by Meekul, et al. [27] and Cannavo, et al. [17] showed that the use of alginate dressing cannot reduce hospitalisation expenses, whereas Chuangsuwanich, et al. [22] showed otherwise. The reasons for this may be related to the different medical fee standards and welfare systems in different countries. In terms of inflammation, although each study used different observational measures, all results indicated that alginate dressings can effectively control inflammatory reactions, which may be related to the strong adsorption of the alginate surface fibre structure [10-12,23,24]. It can adsorb and kill most pathogenic bacteria while forming a protective barrier to reduce the risk of infection [31]. Finally, we describe the role of alginate dressings in reducing adverse wound events. A study by Chen, et al. [10] suggested that the use of alginate dressings can reduce the occurrence of adverse reactions, while one study by Ozaki, et al. [28] had the opposite conclusion. Two studies suggested that the use of alginate dressings can prevent excessive scar hyperplasia [11,14].
Potential limitations of this meta-analysis should also be considered. Only Chinese and English databases were searched; therefore, the literature was not comprehensive. Although all the included studies were all RCTs, the study design was not appropriately rigorous for some articles, and the blinding method and hiding of the distribution scheme were rarely mentioned; thus, the literature quality was medium.
In the future, well-designed multi-centre RCTs with larger sample sizes are needed to provide reliable evidence to support the use of alginate dressings in the treatment of wounds. This meta-analysis provides evidence that alginate dressing is a safe and effective wound-healing treatment. Compared to conventional dressings, alginate dressings are more conducive to promote wound healing, thereby shortening healing time, reducing the number of dressing changes, and alleviating pain in patients. Owing to the inclusion of several medium-quality studies, additional rigorous RCTs are required to confirm the conclusions of this meta-analysis.
The authors declare they have no conflicts of interest.
WL and ZQ participated in the design of this study. ZQ, YW and WW conducted the literature search. ZQ and WW retrieved and selected the articles. QN, ZQ, and WW conducted data extraction and quality assessment. ZQ, GD and WL performed the statistical analysis of the data. ZQ, YW and GD wrote the manuscript draft. GD, ZQ, YW and WL revised the manuscript. GD and WL supervised the study. All authors contributed to the article and approved the submitted version.
This study was supported by Study Project for Reformation of Undergraduate Teaching in Shandong Province (Z2022107), Study Abroad Program for Shandong Provincial Government Education System (2022-44) and Overseas Study Fund Program for Shandong First Medical University (Shandong Academy of Medical Sciences).
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
We thank Dr. Chen for her helpful advice in the submission stage.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Qu Z, Wang Y, Niu Q, Wen W, Ding G, Liu W (2023) Alginate Dressings in Wound Care: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J Clin Exp Dermatol Res. 14:640.
Received: 01-Jun-2023, Manuscript No. JCEDR-23-25306; Editor assigned: 05-Jun-2023, Pre QC No. JCEDR-23-25306 (PQ); Reviewed: 19-Jun-2023, QC No. JCEDR-23-25306; Revised: 28-Jun-2023, Manuscript No. JCEDR-23-25306 (R); Published: 05-Jul-2023 , DOI: 10.35841/2155-9554.23.14.640
Copyright: © 2023 Qu Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.