Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2019)Volume 8, Issue 2
Background: Maternal malnutrition is global health problem affecting higher proportion of women in developing countries. Maternal under nutrition in Ethiopia is amongst the highest in the world and twice sub-Saharan average level 27%. However, little evidences were documented on acute under nutrition and associated factors among pregnant women in Ethiopia in general and the study area in particular.
Objective: To assess acute under nutrition and associated factors among pregnant women in Gumay district of Jimma Zone at, Southwest Ethiopia.
Methods: Community based cross-sectional study was conducted from June 30 to July 30, 2018. Data was collected from 382 pregnant women that randomly selected. The collected data was double entered to Epi-info7 and analyzed using SPSS version 21 software. Descriptive statistics was used to describe characteristics of study participants. Multivariable logistic regressions were carried out, association between independent and dependent variables were measured using adjusted odds ratios and its 95% confidence interval and P-value below 0.05 was considered statistically significant.
Result: Prevalence of acute under nutrition among pregnant women was about 44.9%, [95% CI= 40.0-50.0]. Family monthly income [AOR=8.72 (4.80, 15.83)], Women’s decision making autonomy [AOR=0.40 (0.19, 0.82)], skipping meal [AOR=2.62 (1.41, 4.89)], substance use [AOR=2.01 (1.07, 3.77)], household food insecurity [AOR=2.01 (1.06, 3.80)], lack of prenatal dietary advices [AOR=2.73 (1.53, 4.89)], absence of Household latrine [AOR=9.23 (3.48, 24.46)], not participating health development army’s meeting at village level [AOR=3.01 (1.57, 5.72)] and hand washing habit [AOR=6.55 (3.02, 14.20)] had shown statistically significant association with maternal acute under nutrition.
Conclusion: Magnitude of acute under nutrition among pregnant women was 44.9% in a district. Monthly income, women’s decision making autonomy, skipping meals, substances use, household food insecurity, lack of prenatal dietary advices, poor hand washing habit, lack of latrine and not participate on health development army’s meeting were found to be predictors of women acute under nutrition.
Acute under nutrition; Associated factors; Pregnant Women; Gumay district
AIDS: Acquired Immune Deficiency Syndrome; AOR: Adjusted Odds Ratio; CI: Confidence Interval; DHS: Demographic and Health Survey; FANTA: Food and Nutrition Technical Assistance; FAO: Food and Agricultural Organization; FMOH: Federal Ministry of Health; GAM: Global Acute Malnutrition; HFIAS: Household Food Insecurity Access Scale; IRB: Institutional Review Board; IUGR: Intra-Uterine Growth Restriction; LBW: Low birth Weight; MAM: Moderate Acute Malnutrition; MDD: Minimum Dietary Diversity; MDDW: Minimum Dietary Diversity-Women; MUAC: Mid Upper Arm Circumference; SAM: Severe Acute Malnutrition; SES: Socio Economic Status; SSA: Sub Saharan Africa; WDDS: Women Dietary Diversity Score; WHO: World Health Organization; WRA: Women in Reproductive Age
Malnutrition is pathologic state due to either relative or absolute deficiency or excess of any essential macro or micronutrients that can be acute or chronic type. Acute under nutrition is recent severe weight loss due to food shortage or medical illness [1,2].
Maternal under nutrition is worldwide public health problem affecting wellbeing of millions of women especially in developing countries where 3.5 million women dies yearly, directly or indirectly [3,4]. Globally, under nutrition among women in reproductive age is significantly higher in Africa due to chronic energy and/or micronutrient deficiencies especially during pregnancy [5,6].
Maternal under nutrition has important implication for the health outcomes of both pregnancy and newborns [7]. It reduces productivity, recovery from illness and increase the susceptibility to infections and death [8-10]. It can also determine morbidity, mortality and disability/ ill-health of both pregnant women and children along entire continuum of care [7].
In general, maternal under nutrition has an intergenerational-effect and hence, working on its prevention is long-term investment that benefits current and future generations [11,12].
Maternal under nutrition is a worldwide public health problem affecting higher proportion of women in developing countries, where more than 3.5 million women die per year; directly or indirectly [4,13]. It remains as persistent and destructive health problem in low and middle-income countries [11]. Women in South central and Southeast Asia and Sub-Saharan African (SSA) are the most affected [5,6,14].
The analysis of the EDHS data in 2000, 2005 and 2011 also showed that women under nutrition rates in Ethiopia were 30.5%, 26.9% and 27% respectively [15,16]. Evidence from rural eastern Ethiopia showed that nearly one in every five pregnant women was malnourished [17].
Maternal nutritional status during pregnancy has important implications for health of both pregnant women and newborn babies. It is risk factor for Low Birth Weight, Intra-Uterine Growth Restriction, Small for Gestational Age, Pre-Term Birth, and other adverse outcomes during pregnancy and births [9,18,19]. Malnourished women would have malnourished child [12,19]. Improved maternal dietary quality raises fetal growth [9,12,19].
Certain previous studies showed that inadequate food intake, poor dietary quality and deficiencies of micronutrients, infections due to acute and/or chronic infectious diseases, short birth spacing or interpregnancy intervals, residence area and poor wealth were major determinants of women under nutrition [6,20].
However, there were limited evidences on acute under nutrition and associated factors among pregnant women across the world that could be explained by lack of consensus on type and cut-off-points values of anthropometric parameters to be applied. Even though certain previous studies conducted on prevalence of maternal acute under nutrition was used the Body Mass Index (BMI) <19.80 kgm-2 criteria as cut-off-point value to diagnose women’s acute malnutrition. Few recently published international evidences were used and recommended the MUAC <23cm to diagnose acute under nutrition among pregnant women due to MUAC is a potentially sensitive parameter to identify acute under nutrition among pregnant women [16,21,22].
Despite these facts, little evidences were documented so far on this problem in Ethiopia in general and in Gumay district in particular. Even very few previously conducted surveys were health facility setting. Therefore, the aim of this study was to assess magnitude of acute under nutrition and associated factors among pregnant women in Gumay district, Jimma zone, South West Ethiopia (Figures 1 and 2).
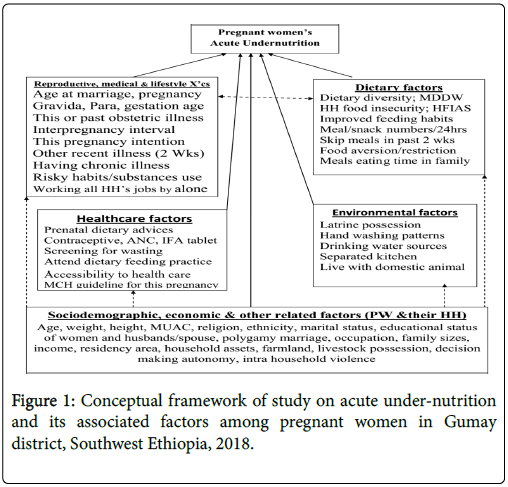
Figure 1: Conceptual framework of study on acute under-nutrition and its associated factors among pregnant women in Gumay district, Southwest Ethiopia, 2018.
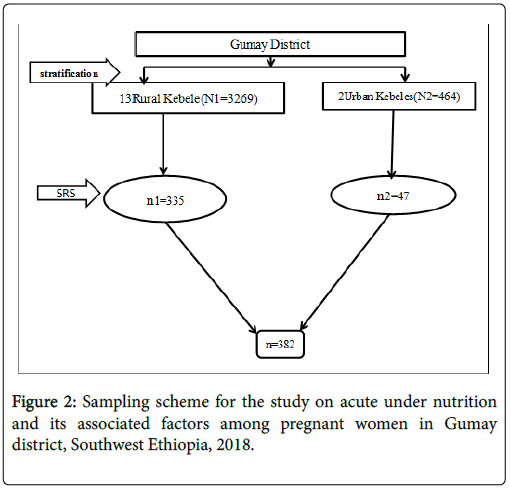
Figure 2: Sampling scheme for the study on acute under nutrition and its associated factors among pregnant women in Gumay district, Southwest Ethiopia, 2018.
Study area and period
The study was conducted in Gumay district of Jimma Zone in Oromia Regional State at Southwest Ethiopia, from June 30 to July 30, 2018.Gumay is one of the districts in Jimma Zone, located at 420 kilometers (km) from Addis Ababa, Capital of Ethiopia in southwest direction. It bordered by Goma district in South and East, by Setema district in north and by Didessa district in West respectively and currently it has 2 urban and 13 rural kebeles administration. In 2018, it has 79,933 populations (39167 males and 40766 females). Of whom, WRA, PW, children and infants were 17665, 3733, 11989 and 2574, respectively.
Potential health service coverage of the district is about 100% in 2017. Currently, 14 health posts, three health centers and four private clinics are providing basic healthcare services. The majority of residents are farmers and merchants. Cereals (maize, sorghum and wheat) are the most common agricultural products and coffee is the known cash crop in the district.
Study design
Community based Cross-Sectional study was conducted.
Source population
Source populations were all pregnant women who were residents of Gumay district during data collection period.
Study population
Study Population was all pregnant women who were residents of randomly selected kebeles of Gumay district.
Sample size determination
Sample size was estimated using single population proportion formula, considering 50% of prevalence of acute under nutrition among pregnant women because there was no similar previous study done in the district and elsewhere in similar setting in Ethiopia as 50% proportion gives maximum sample size. Other parameters considered were 5% margin of error, 95% CI, 10% non-response.
And the initial sample size calculated was greater than 10% of the source population which is 3,733 the sample size was again adjusted with finite population correction formula. The Final sample size n=n0*N/ (n0+ (N-1))=384*3733/ (384+ (3733-1))=348 with 10% nonresponse= 348+34=382 .
Sampling procedure
First, kebeles in the district were stratified into urban and rural areas (kebele is the lowest governmental administrative structure in Ethiopia). Then, sample size was proportionally allocated each stratum and then, representative pregnant women were randomly selected from.
Data collection instrument
Pre-tested-structured questioners adopted from other validated published literatures having several items like socio-demographic, reproductive, medical, behavioral, dietary, healthcare and environmental characteristics were used to collect data. Mid upper arm circumferences of the pregnant women was also measured using standard three colored non-stretchable UNICEF’s MUAC tape. Standard FAO and FANTA checklists were also used to measure MDDW and HFIAS respectively.
Data collection procedure
During data collection, face-to-face-interview, observation, anthropometric measurements and standard checklists were used to collect data from pregnant women after the interviewers explained the purpose of the study and obtained the participant’s verbal consent to participate in the study. In this study, MDDW were measured by FAO-2016 standard checklist developed for this purpose which is recommended for 24 h dietary recalls. Household food insecurity was measured by FANTA-2007 standard tool that has nine questions with each comprising 3 responses; 27-score based HFIAS scale. Acute under nutrition were measured by MUAC (in cm) on their left arms at midpoint between tip of shoulder (olecranon process) and tip of elbow (acromion process) and insertion type of MUAC tape was Benonelastic and non-stretchable to take value with correct tension (not too loose/tight) with nearest 0.1 cm reading. Age, age at pregnancy and inter-birth time were approximated to local memorable events.
Data quality control
All study instruments were translated into local languages (Afan Oromo and Amharic) by native speakers and then back translated to English by two other competent persons. Six interviewers and two supervisors were recruited for the survey and were trained on overall data collection process. All the six data collectors are degree level midwifes and the supervisors were senior public health expertise with master of public health degree who were competent in Afan Oromo and Amharic languages (both are local languages in the study area). The completeness and consistency of data was assured through direct and daily supervision by the supervisors and principal investigators. They returned to interviewers if the data were incomplete and inconsistent. Interviewers re-administered the questionnaire to the respondent under supervision by the supervisor.
Study variables
Dependent variable: Acute under-nutrition among pregnant women.
Independent variable: Independent variables considered for this study were Socio-demographic characteristics of the pregnant women like age, marital status, education, religion, ethnicity, residence area, family size, income, women decision making autonomy, Intra-HH violence and polygamy. Reproductive, medical and behavioral characteristics of the study participants like age at first marriage/ pregnancy, trimester of pregnancy, pregnancy intention, gravidity, parity, abortion, inter-pregnancy interval, recent illness in the past 15 days and substances abuses were also independent variables considered in this study. Others were healthcare and environmental characteristic such as accessibility to healthcare, prenatal dietary advice, contraceptive use, ANC follow-up, drinking water source and latrine possession. Dietary characteristics of the study participants such as Minimum Dietary Diversity of Women, household food insecurity, improved dietary feeding, skipping meals/snack and eating additional meal were also independent variables included in to the study.
Data processing and analysis
The collected data were checked for incompleteness and inconsistency. Data was entered into Epi-Info version 7 software and then, exported to SPSS version-21 for analyzed. Prior to running for analysis, data was cleaned, composite indexes were computed and recoded after missing values and extreme values/outliers were identified and trimmed. Then, descriptive statistics was used to describe sample accordingly.
Bivariate logistic regression was carried out to see the association of each independent variable with acute under-nutrition and those with have p- values below 0.25 remained in to the final models (multivariate logistic regressions). Odds Ratios (OR) was generated for each variable and the independence of any association was controlled by entering all variables into the model using backward stepwise method. The magnitude of the association between the independent variables in relation to acute under-nutrition was measured using adjusted odds ratios (AOR) and 95% confidence interval (CI) and P-values below 0.05 was considered statistically significant.
Operational definition
Acute under-nutrition: In this study, acute under nutrition among pregnant women was measured by MUAC and YES when MUAC<23 cm and No when MUAC ≥ 23 cm [16,20,21].
Decision Making Autonomy: Four “Yes=1/No=0” items were asked to pregnant women on her own autonomy on health seeking, major household purchases, major household expenditures and visiting friends or participation on meetings and responses on four items were combined to define level (0-4) of decision making autonomy. For simplicity of interpretation, combined scores were reduced to 3 levels (0-2); new score of 0 implies score of ‘0’and ‘1’ while scores 2 and 3 were combined to new score of ‘1’ and new score of 2 implies to score of ‘4’ and from new score “low=0” “medium=1” and “high=2” [17].
Prenatal diet feeding habit: Two (Yes/No) items were asked women on whether they change their feeding habits/amount and frequency. Considered improved, when all items answered yes and unimproved otherwise[17].
Prenatal dietary advice: Three (Yes/No) items ever advised to eat more meals, balanced diet and fruits/vegetables asked to women. Considered yes when all items were yes and no otherwise[17].
MDDW: Dichotomous indicators of whether or not feed ≥ 5 of 10 food groups in last 24hrs at day/night [plantains, pulses,nuts/seeds, dairy, meat/poultry/fishes, eggs, dark green leafy vegetables, other vitamin-A rich fruits/vegetables, other fruits and other vegetables] and MDD was ‘low’ when MDDW<5 and ‘high’ otherwise .
Household food insecurity: Nine standard HFIAS occurrence questions developed and recommended by FANTA 2007 guideline were asked to women (in past 28 days) and HH was food secured when all items were answered ‘NO’ or HFIAS scored<1 and food insecure otherwise [23].
Hand washing habit: Women who washed their hands during all activities (after latrine, before food preparation, before eating and after clean child feces) are frequently and not otherwise.
Pregnant women: Women with visible pregnancy to interviewer’s naked eye or their self-report identified visible pregnancy and pregnancy checklist positive for invisible pregnancy[17].
Trimester: When gestational age up to ≤ 13 weeks is 1st trimester pregnancy, from 14-28 weeks is 2nd trimester pregnancy and >28 weeks to 40 weeks is 3rd trimester pregnancy[17].
Drinking water sources: ‘Protected’ if tap/hand pump and not otherwise[17].
Contraceptive use: When women in reproductive age used (≥ 1) any of modern contraceptives (COC, POP, IUCD, Norplant, Implants or Jadelle) but not natural and permanent for spacing births[17].
Socio demographic, economic and cultural characteristics
A total of 374 pregnant women were participated in the study with a response rate of 97.9%. The majority: 321 (85.8%) of participants were rural residents. More than half: 226 (60.4%) of participants were aged 25-34 years followed by youths (15-24 years) age of 76 (20.3%). Their median age was 28 years (IQR=7). About one third: 127 (34.0%) of participants cannot read and write and two third, 249 (66.6%) of them had large family size with the median family size of 5 (IQR=2) (Table 1).
| Characteristics | Categories | Frequency | Percentage (%) |
|---|---|---|---|
| Residence area | Rural | 321 | 85.8 |
| Urban | 53 | 14.2 | |
| Age category in years | 15-24 | 80 | 21.4 |
| 25-34 | 222 | 59.4 | |
| 35-44 | 72 | 19.3 | |
| Religion | Muslim | 291 | 77.6 |
| Orthodox | 64 | 17.1 | |
| Protestant | 19 | 5.1 | |
| Ethnicity | Oromo | 269 | 71.9 |
| Amhara | 48 | 12.8 | |
| Kafa | 31 | 8.3 | |
| Other | 26 | 7 | |
| Current marital status | Married | 352 | 94.1 |
| Others | 22 | 5.9 | |
| Educational status | Not read/write | 127 | 34 |
| Primary school | 182 | 48 | |
| Secondary and above | 65 | 17.4 | |
| Family size | ≥ 5 | 249 | 66.6 |
| <5 | 125 | 33.4 | |
| Household average monthly income | ≤ 1000 ETB | 147 | 39 |
| >1000 ETB | 227 | 61 | |
| Decision making autonomy | Low | 58 | 15.5 |
| Medium | 99 | 26.5 | |
| High | 217 | 58 | |
| Polygamy marriage | Yes | 38 | 10.2 |
| No | 336 | 89.9 | |
| Intra household violence practice | Yes | 55 | 14.7 |
| No | 319 | 85.3 |
Table 1: Socio-demographic, economic and cultural characteristics of pregnant women in Gumay district, Jimma Zone, Southwest Ethiopia (n=374), 2018.
Reproductive, medical and behavioral characteristics
About 179 (47.9%) of participants were get their first pregnancy at teenage (<20 yrs). The majority, 242 (64.7%) of participants had short (<24 months) inter-pregnancy interval and 231 (61.8%) of them used at least one of substance in this pregnancy. Only 62 (16.6%) of them were primipara (Table 2).
| Characteristics | Categories | Frequency | Percentage (%) |
|---|---|---|---|
| Age at first pregnancy (in years) | <20 | 179 | 47.9 |
| ≥ 20 | 195 | 52.1 | |
| Median | 20 (IQR=3) | ||
| Parity | 0 | 62 | 16.6 |
| 01-Mar | 251 | 83.7 | |
| >3 | 61 | 16.3 | |
| Median | 2 (IQR=2) | ||
| Gravidity | ≤ 2 | 140 | 37.4 |
| 03-Apr | 167 | 44.7 | |
| ≥ 5 | 67 | 17.9 | |
| Median | 3 (IQR=2) | ||
| Ant type of Abortion | Yes | 65 | 17.4 |
| No | 309 | 82.6 | |
| Gestational age in weeks | ≤ 28 Weeks | 243 | 65 |
| >28 Weeks | 131 | 35 | |
| Median | 28 (IQR=10) | ||
| This pregnancy intention | Unplanned | 152 | 40.6 |
| Planned | 222 | 59.4 | |
| Any illness during current pregnancy | Yes | 212 | 56.7 |
| No | 162 | 43.3 | |
| Substance use (≥1 of these substances) | Yes | 231 | 61.8 |
| No | 143 | 38.2 |
Table 2: Reproductive, medical and behavioral characteristics of pregnant women in Gumay district, Jimma Zone, Southwest Ethiopia (n=374), 2018.
Dietary characteristics
Prevalence of acute under-nutrition among pregnant women was 168 (44.9%) [95% CI=40.0-50.0] in the district. The majority, 311 (83.2%) of participants had low dietary diversity. Their median MDDW score was 3.4 (IQR=1.4). More than half, 208 (55.6%) of them were living in food insecure household. Three forth, 283 (75.7%) of them had unimproved prenatal dietary feeding (Table 3).
| Characteristics | Categories | Frequency | Percentage (%) |
|---|---|---|---|
| Acute under nutrition | Yes | 168 | 44.9 |
| No | 206 | 55.1 | |
| Minimum Dietary Diversity Women (MDDW) | <5 | 311 | 83.2 |
| ≥ 5 | 63 | 16.8 | |
| Median | 3 (IQR=2) | ||
| Household food security status (HFIAS score) | Food Insecure | 208 | 55.6 |
| Food Secure | 166 | 44.4 | |
| Median | 2 (IQR=8) | ||
| Prenatal diet feeding habits | Unimproved | 283 | 75.7 |
| Improved | 91 | 24.3 | |
| Meals’ feeding time at home | At end/last | 145 | 38.8 |
| First/middle | 229 | 61.2 | |
| Ever skipping meals during this pregnancy | Yes | 215 | 57.5 |
| No | 159 | 42.5 | |
| Food aversion/restrictions | Yes | 147 | 39.3 |
| No | 227 | 60.7 | |
| Eat from outside/friend home | Yes | 160 | 42.8 |
| No | 214 | 57.2 |
Table 3: Dietary characteristics of pregnant women in Gumay district, Jimma Zone, Southwest Ethiopia (n=374), 2018.
Health care and environmental characteristics
Three hundred twenty six (87.2%) participants attended at least one ANC follow-up during their current pregnancy. Prenatal dietary advice was never given for more than half, 213 (57.0%) pregnant women during current pregnancy. The majority, 317 (84.8%) of participants were never screened for wasting during current pregnancy. More than three fourth, 316 (84.6%) of pregnant women do not have integrated national family health guideline/book at their home for their current pregnancy (Table 4).
| Characteristics | Frequency | Percentage (%) | |
|---|---|---|---|
| ANC attendance | Yes | 326 | 87.2 |
| No | 48 | 12.9 | |
| Modern contraceptive | Never use | 140 | 37.4 |
| Ever use | 234 | 62.6 | |
| ITN bed net possession | No | 152 | 40.6 |
| Yes | 222 | 59.4 | |
| Prenatal dietary advices | No | 213 | 57 |
| Yes | 161 | 43 | |
| Screening for wasting | No | 317 | 84.8 |
| Yes | 57 | 15.2 | |
| Participating on HDA meeting | No | 260 | 69.5 |
| Yes | 114 | 30.5 | |
| Attending IYCF demonstration | No | 306 | 81.8 |
| Yes | 68 | 18.2 | |
| Possession of national family health guideline for current pregnancy | Not have | 316 | 84.5 |
| Have | 58 | 15.5 | |
| Latrine possession | No | 316 | 84.5 |
| Yes | 58 | 15.5 | |
| Hand washing habits/patterns | Not frequently | 330 | 88.2 |
| Frequently | 44 | 11.8 | |
| Drinking water source type | Unprotected | 302 | 80.7 |
| Protected | 72 | 19.3 | |
Table 4: Healthcare and environmental characteristics of pregnant women in Gumay district, Jimma Zone, Southwest Ethiopia (n=374), 2018.
Factors associated with acute under-nutrition
Candidate variables for final model (for multivariate analysis): On bivariable analysis residence, age, educational status, marital status , average monthly income, decision making autonomy, age at first pregnancy, parity, pregnancy intention, any illnesses, substance use, prenatal feeding habit, skipping meals, feeding additional meals, avoid at least one food item, HH food security, screening for under-nutrition, ITN bed-net possession, family health guide possession, participating on health developmental army meeting at kebele level, attending IYCF demonstration/practice, ANC follow up , Prenatal dietary advices, modern contraceptive utilization, hand washing practice, Latrine possession and drinking water source type were associated with acute under-nutrition and included in to multivariate model (Table 5).
| Associated factors | Acute Under-nutrition | Crude OR | Adjusted OR | ||
|---|---|---|---|---|---|
| Yes (%) | No (%) | COR (95% CI) | AOR (95% CI) | ||
| Residence area | Rural | 139 | 182 | 0.63 (0.35,1.13) | 0.52 (0.24, 1.12) |
| Urban | 29 | 24 | 1 | 1 | |
| Age category (in years) | 15-24 | 46 | 34 | 1.60 (0.84, 3.04) | 2.04 (0.79, 5.25) |
| 25-34 | 89 | 133 | 0.79 (0.46, 1.35) | 1.09 (0.49, 2.44) | |
| 35-44 | 33 | 39 | 1 | 1 | |
| Marital status | Others | 16 | 6 | 3.51 (1.34, 9.18) | 1.75 (0.41, 7.48) |
| Married | 152 | 200 | 1 | 1 | |
| Educational status | Illiterate | 76 | 51 | 2.51 (1.62, 3.89) | 1.50 (0.77, 2.91) |
| Literate | 92 | 155 | 1 | 1 | |
| Average monthly income in ETB | ≤ 1000 | 110 | 37 | 8.66 (5.38, 13.96) | 8.72 (4.80, 15.83)* |
| >1000 | 58 | 169 | 1 | 1 | |
| Decision making autonomy | Low | 32 | 26 | 1.41 (0.79, 2.53) | 2.7 (1.81, 11.09)* |
| Medium | 35 | 64 | 0.63 (0.38, 1.03) | 0.40 (0.19, 1.82) | |
| High | 101 | 116 | 1 | 1 | |
| Age at first pregnancy | <20 yrs | 87 | 92 | 1.33 (0.88, 2.00) | 1.07 (0.58, 2.00) |
| ≥ 20 yrs | 81 | 135 | 1 | 1 | |
| Parity | <1 | 24 | 38 | 1 | 1 |
| 01-Mar | 110 | 171 | 1.24 (0.70, 2.18) | 0.91 (0.41, 2.05) | |
| >3 | 34 | 27 | 1.99 (0.97, 4.09) | 0.91 (0.32, 2.63) | |
| Pregnancy intention | Unplanned | 81 | 71 | 1.77 (1.17, 2.69) | 0.68 (0.37, 1.23) |
| Planned | 87 | 135 | 1 | 1 | |
| Any illnesses facing | Yes | 105 | 107 | 1.54 (1.02, 2.34) | 1.32 (0.69, 2.52) |
| No | 63 | 99 | 1 | 1 | |
| Substances user | Yes | 121 | 110 | 2.25 (1.46, 3.47) | 2.01 (1.07, 3.77)* |
| No | 47 | 96 | 1 | 1 | |
| Prenatal dietary feeding habit | Unimproved | 144 | 139 | 2.89 (1.72,4.82) | 1.33 (0.56, 3.15) |
| Improved | 24 | 67 | 1 | 1 | |
| Skipping meals | Yes | 81 | 78 | 1.53 (1.01, 2.31) | 2.62 (1.41, 4.89)* |
| No | 87 | 128 | 1 | 1 | |
| Feeding meals additional meal | Yes | 80 | 80 | 1.43 (0.948, 2.16) | 0.67 (0.36, 1.19) |
| No | 88 | 126 | 1 | 1 | |
| Avoid at least 1 food | Yes | 80 | 67 | 1.89 (1.24,2.87) | 0.97 (0.49, 1.92) |
| No | 88 | 139 | 1 | 1 | |
| HH food security status | Insecure | 103 | 105 | 1.52 (1.01,2.31) | 2.01 (1.06, 3.80)* |
| Secure | 65 | 101 | 1 | 1 | |
| Screening for under nutrition | No | 155 | 162 | 3.24 (1.68,6.25) | 1.03 (0.42, 2.55) |
| Yes | 13 | 44 | 1 | 1 | |
| ITN bed net possession | No | 87 | 65 | 2.33 (1.53, 3.55) | 1.25 (0.66, 2.34) |
| Yes | 81 | 141 | 1 | 1 | |
| Family health guide possession | No | 152 | 164 | 2.43 (1.31, 4.51) | 0.56 (0.23, 1.34) |
| Yes | 16 | 42 | 1 | 1 | |
| Attend HDA meeting | No | 136 | 124 | 2.81 (1.75, 4.52) | 3.01 (1.57, 5.72)* |
| Yes | 32 | 82 | 1 | 1 | |
| Attend IYCF demonstration | No | 149 | 157 | 2.45 (1.38, 4.35) | 1.94 (0.71, 5.32) |
| Yes | 19 | 49 | 1 | 1 | |
| ANC attendance | No | 28 | 20 | 2.01 (1.32, 3.08) | 0.73 (0.27, 1.94) |
| Yes | 140 | 186 | 1 | 1 | |
| Prenatal dietary feeding advices | No | 125 | 88 | 3.90 (2.50, 6.07) | 2.73 (1.53, 4.89)* |
| Yes | 43 | 118 | 1 | 1 | |
| Modern contraceptive utilization | No | 78 | 62 | 1.68 (0.98, 2.86) | 1.51 (0.80, 2.83) |
| Yes | 90 | 144 | 1 | 1 | |
| Hand washing pattern/habit | Not frequent | 137 | 141 | 2.04 (1.25, 3.32) | 6.55 (3.02,14.20)* |
| Frequent | 31 | 65 | 1 | 1 | |
| Latrine possession | No | 46 | 9 | 8.24 (3.90,17.43) | 9.23 (3.48, 24.46)* |
| Yes | 121 | 195 | 1 | 1 | |
| Drinking water source | Unprotected | 148 | 154 | 2.50 (1.42, 4.39) | 1.44 (0.64, 3.24) |
| Protected | 20 | 52 | 1 | 1 | |
Note: *statistically significant at P value <0.05
Table 5: Association between Acute under Nutrition and independent variables (Crude & adjusted OR and its 95% CI) among Pregnant Women in Gumay District, Jimma Zone, South West Ethiopia, 2018.
Independent predictors of women acute under-nutrition: In this study average family income of households of the respondents showed statistically significant association with acute under-nutrition i.e., respondents her household monthly income ≤ 1000 ETB were 8.72 times more likely to have acute under-nutrition compared those who have >1000ETB monthly income to farmers (AOR=8.72, 95% CI: 4.80, 15.83) (Table 5).
Decision making autonomy of pregnant women at household level was also showed significantly association with acute under-nutrition. Pregnant women who had low decision making autonomy at household level were 2.70 times more likely to have acute undernutrition compared to those who had high decision making autonomy (AOR=2.70, 95% CI: 1.81, 11.09) (Table 5).
Skipped meals by respondents showed statistically significant association with acute under-nutrition. Respondents skipped meals were 2.62 times more likely to have acute under-nutrition compared to those who did not skip meals (AOR=2.62, 95% CI: 1.41, 4.89) (Table 5).
Pregnant women used substances were 2.01 times more likely to have acute under-nutrition compared to those who didn’t used the substances (AOR=2.01, 95% CI: 1.07, 3.77) (Table 5).
Household food security status was also another variable that showed statistically significant association with pregnant women acute under-nutrition. Pregnant women from household with food insecurity state were 2.01 times more likely to have acute undernutrition compared to their counterparts (AOR=2.01, 95% CI: 1.06, 3.80) (Table 5).
Participating on women’s development army (HAD) at kebele (village) level showed statistically significant association with pregnant women acute under-nutrition. Pregnant women didn’t participated in women’s development army at kebele level were 3.01 times more likely to have acute under-nutrition compared to those who actively participated in the meeting (AOR=3.01, 95% CI: 1.57, 5.72) (Table 5)
Pregnant women who didn’t receive prenatal dietary advices from health professional were 2.73 times more likely to have acute undernutrition compared to those who received the advices (AOR=2.73, 95% CI: 1.53, 4.89) (Table 5).
Pregnant women who had not practiced frequent hand washing habits were 6.55 times more likely to have acute under-nutrition compared to their counterparts (AOR=6.55, 95% CI: 3.02, 14.20) (Table 5).
Pregnant women who were not from households having latrine were 9.23 times more likely to have acute under-nutrition compared to those who were from households having latrine (AOR=9.23, 95% CI: 3.48, 24.46) (Table 5).
In this study, prevalence of acute under-nutrition among pregnant women in the study district was 44.9% (95% CI: 40.0%-50.0%). The observed finding in our study was found to be almost consistent with findings of cross sectional studies conducted in Tahtay Adiyabo district of Tigray region, Northwest Ethiopia which showed the prevalence of under-nutrition was 47.9 % (95 % CI 42.11-53.7 %) [23]. However, the finding in our study is higher than a cross-sectional studies conducted in Eastern Ethiopia[17] , a cross-sectional study conducted in Gambella [24]and institution based cross-sectional study conducted in University of Gondar Hospital, Northwest Ethiopia [25] which showed magnitude of under nutrition among pregnant was 19.06 % , 28.6% and 16.2% respectively. Possible explanation of inconsistency of our study with a latter mentioned three studies may be that our study was fully community based that can show what really exists in the public but the mentioned once were institution based. Difference in study area might also be another reason for inconsistency.
In this study, low average monthly income, women’s autonomy, skipping meals, substances use, household food insecurity, lack of prenatal dietary advices, poor hand washing habit, lack of latrine and not participate on health development army’s meeting were independent predictors of acute under-nutrition.
In this study, pregnant women her household monthly income ≤ 1000 ETB were 8.72 times more likely to have acute under-nutrition compared those who have >1000ETB monthly income to farmers (AOR=8.72, 95% CI:4.80, 15.83). This finding is in agreement with studies conducted in eastern Ethiopia[17], and rural Bangladesh [26].
In our study, pregnant women who had low decision making autonomy at household level were 2.70 times more likely to have acute under-nutrition compared to those who had high decision making autonomy (AOR=2.70, 95% CI:1.81, 11.09). This finding is consistent with studies conducted in eastern Ethiopia[17] and University of Gondar Hospital, Northwest Ethiopia [25]. In addition, this finding was also consistent with findings of cross sectional household studies done in rural India which showed statistically significant association of maternal autonomy with stunting [27]. The above indicated finding is also in agreement with other studies conducted in India that shows statistically significant association between maternal under nutrition and their autonomy at household level [28].
In ours study, pregnant women who skipped meals were 2.62 times more likely to have acute under-nutrition compared to those who did not skip meals (AOR=2.62, 95% CI:1.41, 4.89) which is consistent with a community based study conducted in rural parts of eastern Ethiopia[17].
In our study, pregnant women who didn’t receive prenatal dietary advices from health professional were 2.73 times more likely to have acute under-nutrition compared to those who received the advices (AOR=2.73, 95% CI: 1.53, 4.89). Our finding on effect of prenatal dietary advice on acute under-nutrition among pregnant women also goes with other previous studies done in eastern Ethiopia and Bangladesh [17, 29]. This could imply prenatal dietary advice is one of the key interventions that all health institutions should do integrating it with other services given to pregnant women at antenatal care clinic.
In this study, Household food security status was also another variable that showed statistically significant association with pregnant women acute under-nutrition. Pregnant women from household with food insecurity state were 2.01 times more likely to have acute undernutrition compared to their counterparts (AOR=2.01, 95% CI:1.06, 3.80). This finding is consistent with findings of studies conducted in Tigray region [23], Gambella [24] and Nepal [30].
Our study also reveals that, pregnant women who had not practiced frequent hand washing habits were 6.55 times more likely to have acute under-nutrition compared to their counterparts (AOR=6.55, 95% CI: 3.02, 14.20). This finding on hand washing habit should be emphasized for preventive intervention measure.
In our study, pregnant women who were not from households having latrine were 9.23 times more likely to have acute undernutrition compared to those who were from households having latrine (AOR=9.23, 95% CI:3.48, 24.46) . The possible explanation for this finding is that the latrine utilization could have numerous health benefits associated with sanitation and hygiene. This finding was in line with the findings of studies EDHS based study conducted in Ethiopia [31], and Northwest Ethiopia [25] and Bangladesh [29].
Our study also showed that, pregnant women used substances were 2.01 times more likely to have acute under-nutrition compared to those who didn’t used the substances (AOR=2.01, 95% CI: 1.07, 3.77). This finding is consistent with finding of studies conducted in eastern Ethiopia [32], data from systematic review and dose-response metaanalysis [33] and another study done on Cigarette smoking, alcohol use and adverse pregnancy outcomes [34].
In our study, participating on women’s development army (HAD) at kebele (village) level showed statistically significant association with pregnant women acute under-nutrition. Pregnant women didn’t participated in women’s development army at kebele level were 3.01 times more likely to have acute under-nutrition compared to those who actively participated in the meeting (AOR=3.01, 95% CI:1.57, 5.72). The implication of this finding may be that participating pregnant women in health development arm at their living are may have a significant role in reducing acute under nutrition of pregnant women.
Strength of the study
This study considered several independent variables and used many composite indexes during analysis that might improve validity of the measurements. The study was community based study in which primary data was directly collected from pregnant women visiting their house. The study also tried to use standardized tools and procedures in measuring dietary and other characteristics of participants which could be mentioned as strength of the study.
Study limitations
Despite our efforts to cover wide range of risk factors, there were variables unmeasured such as laboratory assessment of some nutritional relevant diseases including intestinal parasites. Most data on exposure variables were obtained by maternal self-report which could be potential for recall biases. Social desirability biases might also occur as some of the questions were culturally sensitive to study participants even though we took a maximum possible cares.
In this study, magnitude of acute under nutrition among pregnant women was 44.9% and it is interpreted as high magnitude. Average family income of households of the respondents, decision making autonomy of pregnant women at household level, Skipping meals by respondents, Using Substance, household food insecurity, participating on women’s development army (HAD) at kebele (village) level, prenatal dietary advices from health professional, not practicing frequent hand washing habits, being from households not having latrine were found to be independent predictors of pregnant women acute under nutrition.
Based on the findings of the study the following recommendations are forwarded to all responsible organizations.
Stakeholders like Ethiopian federal Ministry of health, Oromia regional health bureau, Jimma zone health department, Gumay District, health institutions and health professionals working in the district, and non-governmental partners working on maternal and child health should focus on sustainable and intensive information dissemination and behavioral change communication to pregnant women and their partners about under nutrition and its health consequences specially during pregnancy.
Efforts should also made to enhance women’s decision making autonomy at household level, avoid skipping meals, avoid using substance, solve the problem of food insecurity, involve women in women’s development army (HAD) activities, give prenatal dietary advices from health professional at all primary health care and community level, improve hand washing habits, encouraging possessing and properly utilizing latrine among all households.
Ethical clearance was obtained from Arsi University College of Health Sciences research ethical and review committee. The permission to conduct the study was obtained from Gumay District and all selected kebeles. Verbal consent was obtained from each study participant. All interviewers are oriented on how to obey the rules of strict confidentiality practices for all clients both during and after data collection.
Availability of data and materials
Data supporting the findings is available upon request. Please contact the Principal Investigator of the study, Gebi Husein (gebihussein@gmail.com).
The authors declare that they have no competing interests
We authors extend our very genuine appreciation to Arsi University College of Health and Science Oromia regional health bureau for sponsoring the study. Our very thankful also goes to Gumay district health office, Gumay district health workers and Health extension workers in the selected kebeles for their unreserved support they made during data collection. We also appreciate all study participants for genuinely sharing data cooperatively. Last but not list, we are grateful to all data collectors and supervisors for handling their duties in a very responsible ways.
The whole research fund was covered by Arsi University and Oromia regional health Bureau. However the university had no role in the design of the study, collection, analysis, interpretation of data and in writing the manuscript.
As involved in proposal writing, designing, recruitment and training of supervisors & data collectors, analysis and write-up of the paper. GH contributed in the designing of the project proposal and methodology, led the study, design of questionnaires, supervised and involved in the analysis stage of the project, final approval of the paper and preparation of the manuscript. Both authors read and approved the final manuscript.
Citation: Shiferaw A, Husein G (2019) Acute Under Nutrition and Associated Factors among Pregnant Women in Gumay District, Jimma Zone, South West Ethiopia. J Women's Health Care 8:458. doi:10.35248/2167-0420.19.8.459.
Received: 21-Nov-2018 Accepted: 13-Apr-2019 Published: 20-Apr-2019
Copyright: © 2019 Shiferaw A, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.