Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2019)Volume 10, Issue 2
Introduction: Acne keloidalis nuchae (AKN) is a chronic folliculitis along the nape of the neck and occipital scalp that results in scarring alopecia and disfiguring keloid-like plaques often associated with infection, pain, bleeding, malodor, and progression in size. AKN appears similar to keloids, yet there are differences in pathophysiology. These two cases highlight a surgical treatment course for AKN that plastic surgeons can incorporate into their practice.
Methods: Two case studies of 25-year-old African-American males with several year histories of keloid-like masses of the posterior scalp that had been medically managed as keloids and presented to clinic for second opinions. They underwent local wide excision of AKN masses that included the posterior hairline and at least 0.5-centimeters of healthy tissue margin, followed by secondary intention healing.
Results: Patients were followed post-operatively and had aesthetically acceptable outcomes with significant improvement, one with disease-free result and the other with evidence of new disease superior to his wound requiring repeat excision and radiation.
Conclusions: By completely excising the affected tissue, along with removal of the posterior hairline, patients can be disease-free and have an aesthetically acceptable outcome.
Acne keloid; Folliculitis
Acne keloidalis nuchae (AKN) is a chronic folliculitis along the nape of the neck and occipital scalp that results in scarring alopecia and disfiguring keloid-like plaques [1-3]. This inflammatory disorder of the hair follicles disproportionally affects African-American men after puberty and is initially characterized by small pustules and papules [1-3]. In some patients, these plaques further develop and form larger keloid-like masses that are commonly associated with bleeding, malodor, infection, pain, and progression in size [1-4].
Nearly all of the literature that describes acne keloidalis nuchae (AKN) has been published within the dermatologic research community, yet there is an unknown number of patients who are seen by plastic and reconstructive surgeons and are likely misdiagnosed and incorrectly treated as keloids.
While acne keloidalis nuchae (AKN) has a similar clinical appearance to keloids, there are clear differences in the histology, recurrence rates, and treatment options for the disease. Plastic and reconstructive surgeons need to be aware of these differences in order to appropriately diagnose and successfully manage these two distinct pathologies.
Our goal is to emphasize the differences between AKN and keloids by presenting two successful examples of AKN treatment. We believe that these cases add another surgical technique to the broad armamentarium that plastic and reconstructive surgeons incorporate into their practice.
Below are two case reports highlighting the effective and aesthetically acceptable results after the wide excision of acne keloidalis nuchae masses that included the posterior hairline, followed by secondary intention healing.
A 25-year-old African-American man with a history of chest and shoulder keloids presented to the plastic surgery clinic with an 8 × 5 centimeter posterior scalp "keloid" that he had since he was an early teenager. He described that it started as an inflamed hair follicle that has been steadily increasing in size. He also noted that it limits his full range of neck motion. He was previously medically managed with steroid injections and noted the lesion has softened slightly but did not decrease in total size.
Preoperative
In clinic, the patient was preoperatively counseled on the risks, benefits, complications, treatment options, expected outcomes and postoperative course of proceeding with wide local excision and healing by secondary intention. The possibilities of reaction to medication, anesthesia, the need for additional procedures, failure to diagnose a condition, and creating a complication requiring treatment or surgery were discussed as part of the informed consent process.
On the day of surgery, the affected area was marked out with at least 0.5 centimeters of healthy uninvolved tissue as a border superiorly and laterally. The posterior hairline was included in the pre-operative markings despite the fact that actively diseased tissue did not extend that far inferiorly. The excised tissue measured 12.5 × 6 centimeter.
Intraoperative
The patient was administered general anesthesia, placed prone on the operative table and was widely prepped with Betadine without additional shaving around the operative field. A local field block was administered using 1% lidocaine with epinephrine 1: 100,000 mixed with an equivalent amount of 0.25% bupivacaine. The mixture was injected in the subcutaneous plane, circumferentially around the wound, with needle punctures within the keloid-like mass and needle aimed towards the edges. This was done to prevent further trauma to the neighboring healthy tissue.
The original pre-operative markings were used to guide the excision (12.5 × 6 centimeter) and a number 15 blade was used to incise the skin down to the underlying fat layer that was located directly on the fascia. Ensuring no violation of the fascial layer, the entire scar burden was removed down to healthy fat and fascia. Monopolar cautery was used at a blend setting of 35 watts to simultaneously lift the keloidal tissue and follicles while coagulating small vessels encountered. The affected tissue was removed en-bloc and meticulous hemostasis was completed with monopolar cautery and irrigated with normal saline. At this point more of the local anesthetic mixture was directly injected into the wound bed for additional anesthesia. For post-operative dressings, a loose moist bolster dressing was applied to the wound. Copious amounts of triple antibiotic ointment were applied to the wound bed and covered completely with Xeroform gauze (non-adherent, sterile, fine mesh gauze impregnated with 3% Bismuth Tribromophenate) then layered with moistened 4 × 4 centimeter sterile gauze, followed by another layer of Xeroform gauze, topped with dry abdominal pads and secured with a Kerlex headwrap. The patient was discharged the same day with one week of antibiotics (Duricef 500 mg BID) and pain medication as needed.
Postoperative
Forty-eight hours following surgery, the dressings were removed in the office and inspected for signs of infection. The patient was instructed to change the dressings twice daily and to replace them with a simple wet-to-dry regimen of saline damp 4 × 4 centimeter gauze pads and dry abdominal pads secured with either Kerlex headwrap or surgical tape. We recommend to patients to use non-fragrance soap and to remove dressings in the shower after they are saturated, as they are easier to remove with less discomfort. The patient returned for follow up appointments at 2, 4, 5, 7, 10, 14, and 18 weeks postoperatively (Figure 1) and subsequently every 2 months afterwards. When the wound is fully closed (approximately 8-9 weeks), the patient was instructed to dress wound with triple antibiotic ointment and leave open to air. At 14 week, 6 months, and 8 months the wound looked slightly raised and the decision was made to inject 3 cc of Kenalog 50 mg/ml along the entire length of the scar. He is now 15 months post-operative, and at his most recent appointment he reported being very happy with the aesthetic and functional result, yet inquired about further intervention to address an area of new disease superior to his wound. This would require another round of wide local excision, although less extensive than the original surgery. Pathology at the time of original excision revealed dense acute and chronic inflammatory processes with follicular disruption consistent with AKN.
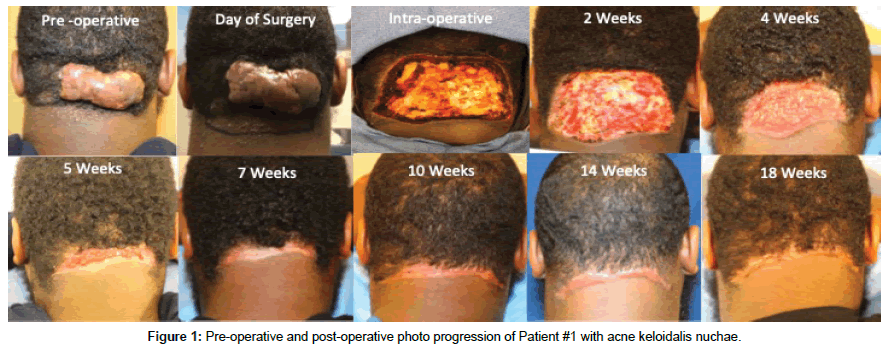
Figure 1. Pre-operative and post-operative photo progression of Patient #1 with acne keloidalis nuchae.
A 25-year-old African-American man with no history of keloids presented to the plastic surgery clinic with an 11 × 7 centimeter posterior neck mass that he has had for two years. He reports that he is embarrassed of the size and the fact that it is nearly impossible to obtain a haircut without bleeding. He has been medically managed with steroid injections with minimal softening, but no decrease in overall size.
The surgical management was identical to the previous patient except the lesion excised measured 12 × 9.5 centimeter. He returned for follow-up at 2, 4, 5, 7, 10, 12, and 14 weeks post-operatively and subsequently every 2 months afterwards without issues or need for steroid injection (Figure 2). He now is 13 months post-operative, happy with the aesthetic result, and reports he is working and cutting his hair without issue. Pathology also revealed suppurative ruptured folliculitis, consistent with acne keloidalis nuchae.
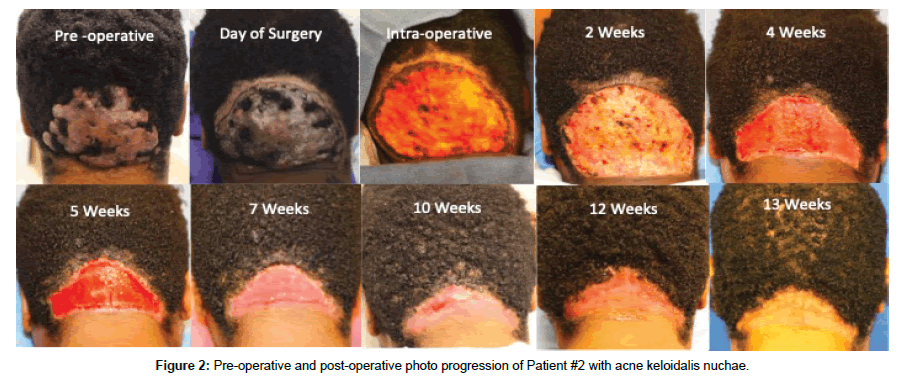
Figure 2. Pre-operative and post-operative photo progression of Patient #2 with acne keloidalis nuchae.
The exact origin of acne keloidalis nuchae (AKN) is currently unknown, yet studies have suggested that inflammation, trauma, chronic hair follicle irritation/ingrowth, infection or hormones play a role in its etiology [1-8]. The leading theories suggest that skin injury or trauma to the area may cause an immune reaction that leads to primary cicatricial alopecia and abnormal keratin formation [6-9]. Histologically, AKN is characterized by the initial infiltration of neutrophils and lymphocytes during the chronic perifollicular inflammatory phase and later stages illustrate the subsequent destruction of hair follicles [6,10]. Medical management for AKN consists of a number of options that include topical treatment (corrosives, corticosteroids, antibiotics, immune modulators) intralesional steroid injections, cryotherapy, systemic therapy (tetracycline derivative antibiotics, retinoids), and laser therapy (1064 nm Nd:YAG, 810 diode, carbon dioxide) [2,4,10,11]. There are a limited number of case reports that look specifically at wide excision and healing by secondary intention in patients with AKN, yet those studies report a 0% recurrence rate [5,12,13]. There is a growing understanding that to prevent recurrence, all of the even potentially diseased tissue must be removed with the active lesion. That along with the desire to have a relatively naturally appearing new posterior hairline is why the original posterior hairline is included in the resection [14].
In comparison, the exact mechanism of keloid formation has not been elucidated, yet is linked to a previous trauma or surgical site and is thought to be due to abnormal regulation of collagen equilibrium [15]. It is characterized histologically by disorganized extracellular architecture and randomly oriented collagen fibrils that have overgrown beyond the border of the original scar [15]. Another important difference to note is the recurrence rate cited in the literature for surgical management of keloids is highly varied and as high as 100% [15].
There are differences in the medical management of keloids and AKN that are outside the scope of this case report, but as illustrated through the provided cases, the surgical management for AKN is drastically different than if the lesions were traditional keloids. For example, if either mass in the above cases were a traditional keloid, the senior author would have offered a different treatment regimen out of near assurance of a recurrence otherwise. He would have chosen tissue expander placement in nearby healthy tissue followed by a several month expansion process. This would have been preceded by excision of the lesion without incorporating the posterior hairline, removal of the tissue expander, and primary closure with non-dissolvable sutures using the newly expanded skin. Intraoperative steroid injections within the incision would have then been performed and likely a recommendation to receive low dose post-operative radiation treatment to the wound. This option is significantly different than the surgical approach to the two above patients with AKN.
It is important to note that one of our patients is pursuing further surgical management due to new disease superior to his previous excision. It is important to consider that when counseling patients with this diagnosis that there is an open discussion that further surgical intervention may be warranted if the entire area of disease is not removed successfully on the first excision. The senior author balances aggressive removal of affected tissue with awareness of the physical effects of removing hair-bearing tissue, by excising the tissue that he visually inspects as being affected with an additional 0.5 cm margin. With that said, it may be worth considering excision of more than the 0.5 cm in the superior margin, as it may be difficult to differentiate disease in hair bearing areas.
The novelty of this case report is that prior citations, solely in the dermatologic literature, were primary older men with less aggressive and smaller keloidal-like masses. The two examples presented here are young African-American men with large, extensive pathology. The senior author has treated many more keloid patients than those with a diagnosis of AKN, yet has learned through his experience with the cases above that plastic and reconstructive surgeons can approach the management of the AKN patient with different surgical options.
The authors would like to thank Dr. Richard Bennett for his willingness to share his experience over his illustrious career.
The authors have nothing to disclosure
Citation: Ligh CA, Butler PD (2019) Acne Keloidalis Nuchae is Not the Same as a Keloid: A Case Report of Successful Excision with Healing by Secondary Intention. J Clin Exp Dermatol Res 10: 487. doi:10.4172/2155-9554.1000487
Received: 03-Feb-2019 Accepted: 05-Mar-2019 Published: 12-Mar-2019
Copyright: © 2019 Ligh CA et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Sources of funding : GB´s PhD-project on ethical challenges and decision-making in nursing homes has been financially supported by the Norwegian Extra Foundation for Health and Rehabilitation through EXTRA funds (grant no. 2008/2/0208).