
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Case Report - (2021)Volume 12, Issue 1
Background: Local anesthetics act on demyelinated fibers by increasing the degree of conduction blockade already present in the demyelinated segments of multiple sclerosis.
Case report: We report an unusual prolongation of the duration of spinal anesthesia in a patient with MS, through this case and a review of the literature we discuss the causes of this incident and its relationship with demyelination, preventive measures and how to proceed in at-risk situations.
Conclusion: The excessive prolongation of spinal anesthesia beyond the conventional time frame is an uncommon but worrisome situation. Preoperative screening for neuropathy preoperative screening for neuropathy prompts to explore a conduction abnormality and informing the patient about the nervous toxicity risk of local anesthetics. ILE is probably a very interesting way to avoid their adverse effects
Spinal anesthesia; Local anesthetic; Hysteroscopy; Multiple sclerosis; Demyelination
MS: Multiple Sclerosis; LA: Local Anesthetic; ILE: Infusion Lipid Emulsion; CNS: Central Nervous System; LRA: Locoregional Anesthesia
Multiple sclerosis (MS) is the inflammatory disease of the central nervous system (CNS) which results in focal demyelination plaques of the encephalic and medullary white matter; it affects twice as many women as men, generally between 20 and 40 years old. The demyelinated neurons will acquire a high sensitivity to the neurotoxicity of local anesthetics (LA) and aggravate the conduction block [1].
We report an unusual prolongation of the duration of spinal anesthesia in a patient with MS, through this case and a review of the literature we discuss the causes of this incident and its relationship with demyelination, preventive measures and how to precede at risk situations.
Written informed consent was obtained from the patient. This was the 52 year old patient, mother of 4 children, with a history of multiple sclerosis, which has been evolving for more than 15 years; the revealing symptoms were a type of episodes of amnesia, unease feeling, muscular tiredness associated with visual disorders; the diagnosis was confirmed by MRI (Figures 1A and 1B) showing cerebral-medullary demyelination lesions. Currently in remission and not taking any treatment, the last relapse dates back 6 months.
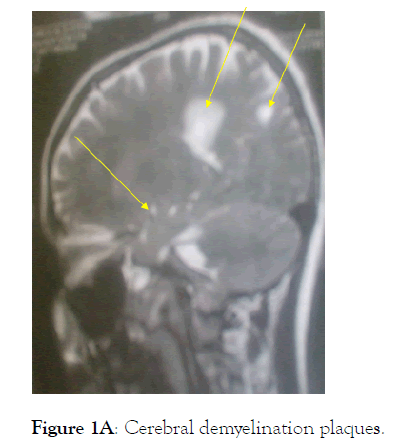
Figure 1A: Cerebral demyelination plaques
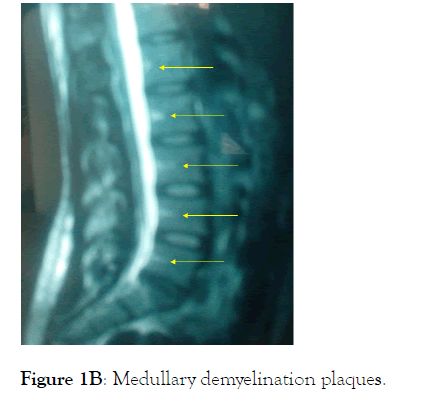
Figure 1B: Medullary demyelination plaques.
Our patient had presented for a few week’s low abundance of metrorrhagia, pelvic ultrasound revealed the presence of endometrial hyperplasia, whence his referral to the obstetrics and gynecology department for etiogical diagnosis and treatment. The preoperative examination found a patient in good general condition, a BMI at 29; the neurological examination showed a slight muscle weakness rated 4/5, without sensory deficits. The remainder of the physical examination is without abnormalities. The standard biological assessment, the chest x-ray as well as the electrocardiogram was normal, The patient was classified as ASAII by the American Society of Anesthesiologists. She was subsequently scheduled for hysteroscopy with biopsy curettage on an ambulatory.
Our patient had presented for a few week’s low abundance of metrorrhagia, pelvic ultrasound revealed the presence of endometrial hyperplasia, whence his referral to the obstetrics and gynecology department for etiogical diagnosis and treatment. The preoperative examination found a patient in good general condition, a BMI at 29; the neurological examination showed a slight muscle weakness rated 4/5, without sensory deficits. The remainder of the physical examination is without abnormalities. The standard biological assessment, the chest x-ray as well as the electrocardiogram was normal, The patient was classified as ASAII by the American Society of Anesthesiologists. She was subsequently scheduled for hysteroscopy with biopsy curettage on an ambulatory.
On the morning of the operation, the patient received 2 mg of midazolam and 1 gm of cefazolin preoperatively; at 8:30 a.m. in the operating room after standard monitoring and in the sitting position The spinal puncture was performed without difficulty in the L4-L5 space, with a needle from Whitacre 27G. She had received in the subarachnoid space 10 mg of isobaric bupivacaine 0.5% (2 cc), combined with 2.5 Ɣ of sufentanyl (0.5 cc), the injection speed was 1 ml/5 seconds. The patient was immediately placed in the supine position, the maximum sensory level required for low endoscopic gynecological surgery is T10 was reached in 5 min, correlated with a Bromage score equal to 3 (complete motor block). The installation in gynecological position is then carried out, followed by the introduction of hysteroscopy after water-distension with isotonic saline, which allowed us to confirm the endometrial hypertrophy and to perform extensive biopsy curettage.
The intervention lasted 30 minutes and upon completion the patient was transferred to a post-interventional care unit. At this moment of hospitalization, we observed a persistence of the sensory-motor block at the same level and score after a period of 4 hours. Ahead of this abnormal prolongation of the effect of spinal anesthesia and to deal with this diagnostic and therapeutic problem, we had decided to eliminate a neurosurgical emergency, a spinal cord MRI was performed eliminating any local anomaly and especially the compressive perimedullary hematoma.
Subsequently, after 7 hours of evolution, the examination of the patient regains a stationary sensory-motor level, without hemodynamic or respiratory repercussions. Faced with this worrying situation, a lipid emulsion infusion (ILE) was administered to attempt an antagonization of local anesthetics with a bolus of 3 ml/kg ILE (Intralipid® 20%) as a slow intravenous injection within 10 minutes.
Thirty minutes later, the patient had started to feel an onset of relief in the intensity of the sensory-motor block, however the total regression of the motor block was obtained after 2 h, and of the sensory block after 5 h.
In total, we observed persistence of the motor block for nine hours, sensory recovery after twelve hours, with no sign of hemodynamic or respiratory intolerance or bladder retention (bladder catheter in place). After the block was lifted, the patient had not presented any other incidents and the next day was discharged with a consultation appointment. Her 3 month follow-up did not reveal any relapse of her disease,.
The abnormal prolongation of a peripheral or central nerve block can be defined as an exceeding of the usual sensory and/or motor recovery time, which raises fears of complications and requires a diagnostic and therapeutic approach [2].
Neurological complications related to spinal anesthesia are reported to five causes: hematoma or compressive abscess, direct toxicity of anesthetics, mechanical nerve damage related to posture, direct trauma by the puncture needle.
Compression of the spinal cord by a hematoma, or abscess, has been eliminated by lumbo-sacral MRI, which is the reference for diagnosing this complication. The occurrence of perimedullary hematomas is very rare, Moen reports 7 cases after 1 260 000 spinal anesthesia [3]. Anticoagulants or antiplatelet agents are almost always involved in these situations, while epidural abscesses occur a few days (4-10 days) after the spinal anesthesia procedure.
Positional nerve injury or direct needle trauma seems unlikely, spinal anesthesia was performed without incident, and in particular no paresthesia was noted. Several authors have insisted on the mechanical factors that can promote a neurological complication, Warner et al. [4] analyzed 198 461 patients operated on in a gynecological position (lithotomy), reporting 55 cases of sensory-motor disorders of the lower limbs. The risk factors added to the lithotomy position were: a prolonged operating time greater than 4 hours (main risk factor for postoperative neuropathy) and the BMI less than 20. In our case the operating time was very short (30 min) and the patient's BMI of 29.
Other causes are related to the patient's condition such as diabetes, peripheral neuropathy, spinal cord neuropathy, and age over 65 years, are factors that abnormally prolong the duration of the peripheral or central block [5].
Koné et al. reported the case of an unusual 23 hour extension of the sensory-motor duration of an analgesic femoral block, in a 42 year old patient with no particular history followed for chronic cruralgia without motor deficit, no abnormalities locale was noted. The allodynia presented by the patient suggested chronic suffering related to a pre-existing neuropathy [6].
The myelin is a protective sheath that envelops the nerves and is essential for the transmission of electrical signals Multiple sclerosis is a chronic autoimmune disease of the central nervous system characterized by inflammation and demyelination, causes a difficulty in conduction of the nerve impulses within the axons (information travels less quickly, if at all), on the other hand, the contact of a concentrated solution of local anesthetic (LA) on these nerve roots is responsible for the neurotoxic effect, as has already been proven on ponytail roots known for their low myelination and high sensitivity to AL [1].
Sakurai and Al administered Lidocaine intravenously to 28 patients with multiple sclerosis and 19 normal subjects, for a plasma concentration of 2.7 μg/ml. No normal subjects showed symptoms, but 23 of the 28 MS patients showed transient and reversible neurological deficits, including visual deficits (15/23); the hypothesized mechanism is that partial blockage of sodium channels produced by the low concentration of local anesthetic is not sufficient to block conduction in normal CNS tissue, but may exacerbate the pre-existing partial blockage in demyelinated plaque, thus revealing transient deficits [1].
Kytta et al. noted that out of 56 patients with multiple sclerosis, five patients who underwent central nerve block under epidural anesthesia with bupivacaine concentrations greater than 0.25%, their sympathetic block was extensive with marked hypotension and response reduced to vascular loading and vasopressors, concluding that the absorption of local anesthetics in the spinal cord is greater after spinal or epidural injections in the presence of demyelination [7].
Moreover, it has been observed in some studies, that when local anesthetics are applied to nerve trunks or in the spinal cord in the presence of demyelination, this causes an extension of the anesthetic duration, thus Finucane and Col found in a 33 year old woman without a pathological history programmed for inguinal hernia treatment under general anesthesia who had benefited from an analgesic lumbar paravertebral block at the end of the operation, that the sensory-p required a duration of 12.5 h, the authors believe that this duration was much longer than expected, even after spinal, epidural or subdural diffusion of a local anesthetic. Further etiological investigations revealed a disease of multiple sclerosis [8].
In the case of our patient undergoing spinal anesthesia with a usual duration of 90 min, was excessively prolonged up to 12 hours and given her history of MS, this incident is probably related to the increased sensitivity of demyelinated neurons to AL neurotoxicity.
Therefore, the responsibility of spinal anesthesia seems plausible given the minor nature of the surgical act and the chronology of events. Despite the divergent on the anesthetic management of MS, spinal anesthesia is still frequently used in these patients. On the contrary, some authors consider that MS should not be considered as a contraindication to epidural or spinal anesthesia [9,10]. In view of the benefits offered to this population of patients, particularly during obstetrical labour or for patients whose respiratory function cannot be assessed in the preoperative phase due to serious neurological injuries or in the context of bladder spasticity in urological surgery. On the other hand, the choice of anesthetic technique should rather be based on: discussion with the patient about the potential anesthesia technique, patient preference, estimation of the benefit/risk ratio of each technique for each patient and respect of absolute contraindications.
Regarding the prevention of this incident, it involves the preoperative diagnosis of neuropathy via the detection of nerve conduction abnormalities at the electromyogram; the judicious choice of LA, giving priority to the least neurotoxic, knowing that the toxicity ratios of bupivacaine, ropivacaine and lidocaine are approximately 4:3:1 [11] and it is recommended to plan the surgery during the remission period for elective surgery.
With regard to the management of this incident, although it is not possible to say with certainty that the use of lipids was responsible for the reversal of the sensory-motor block, but it should be said that the use of infusion lipid emulsion in the treatment of LA induced cardiovascular toxicity has been well documented [12,13]; however, the role of lipid in the treatment of isolated LA induced central nervous system toxicity, although reported [14]. It is through case reports that we can assess the accuracy of our conduct and not through controlled trials (an ethical concern), It should be noted that only those learned societies of anesthesia that are empowered to authorize or not authorize its inclusion as an approved practice.
Ultimately, it can be said that excessive prolongation in duration of spinal anesthesia beyond the usual time is an uncommon but worrying situation; preoperative screening for neuropathy prompts us exploration of a conduction abnormality, informing the patient about the neurotoxic risk of LA when LRA is chosen by the physician and the patient; nevertheless, prevention is through the use of less neurotoxic local anesthetics, ILE are probably a very interesting way to treat their ill effects.
Not applicable
The patient involved provided written consent for reporting of this case.
Not applicable
The authors declare no conflicts of interest
The authors have no sources of funding to declare for this manuscript
HM developed the idea and the design of the study. BD revised literature, collected the data, FN analyzed the data, HM wrote and critically revised the manuscript. All authors read and approved the final version of the manuscript.
The author would like to thank all the medical and paramedical staff of the Gyneacology and Obstetrics Department of the Bab El Oued University Hospital Center who participated in the recruitment and care of the parturient. Ms Mechouch Djoher for her participation in the English translation of this article.
Citation: Mohamed H, Dalila D, Berbiche R, Bouderbala F, Nadia F (2021) Abnormal Prolonged Duration of Spinal Anesthesia in Patient with Multiple Sclerosis. J Anesth Clin Res. 12: 984.
Received: 31-Dec-2020 Accepted: 14-Jan-2021 Published: 21-Jan-2021 , DOI: 10.35248/2155-6148.21.12.984
Copyright: © 2021 Mohamed H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.