Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2019)Volume 10, Issue 3
Introduction To study the extent of repigmentation after autologous epidermal non-cultured cell suspension in stable vitiligo patients. Patients and Methods A prospective, longitudinal study was conducted to study the extent of repigmentation after autologous epidermal non-cultured cell suspension in 30 stable vitiligo patients Results By subjective assessment, 10% (3) patients showed poor response, 30% (9) showed good response and 60% (18) patients showed excellent response after follow-up at 6 months with good patient satisfaction. By objective assessment 10% (3) patients showed poor response, 13.3% (4) showed fair response and 23.3% (7) patients showed good response, 53.3% (16) patients showed excellent response after follow-up at 6 months. Extent of repigmentation was evaluated as-10% (3) showed poor response, 10% (3) showed fair response and 20% (6) patients showed good response, 60% (18) patients showed excellent response after follow-up at 6 months. Conclusion Autologous non-cultured epidermal cell suspension in stable vitiligo is a safe, effective, simple method, with superior quality of repigmentation.
Vitiligo; Vitiligo surgery; Grafting; Dermabrasion; Repigmentation; Non-cultured melanocytes
Vitiligo is an autoimmune disorder characterized by asymptomatic, localized and/or generalized depigmentation of the skin and/or mucous membranes in the form of typical chalky-white or milky macule(s) [1] with incidence ranges from 0.1 to>8.8% across India [1,2], most of the studies showing female preponderance [1].
Many treatment modalities are currently used for vitiligo like topical, systemic, phototherapy, lasers and surgical methods.
Recent surgical advances include autologous non-cultured epidermal cell suspensions and cultured melanocyte suspensions [3].
A study was undertaken to evaluate the extent of repigmentation after autologous epidermal non-cultured cell suspension in stable vitiligo patients.
A complete history with precipitating factors, previous medical treatment, any associated diseases, was obtained followed by a complete physical examination.
Routine blood investigations were done and tests for thyroid function done where required. Preoperative photographs of donor and recipient area were taken. Postoperative pigmentation was evaluated using scoring system and digital photography.
Patients
Study population: The study is conducted on a study population of 30 patients presenting with stable vitiligo attending OPD in Department of DVL, Santhiram Medical College and General Hospital, Nandyal.
Inclusion criteria:
1. Stable vitiligo not responding to medical treatment
Exclusion criteria:
1. Age<12 years, >50 years
2. Unstable vitiligo
3. Koebner’s phenomenon
4. Keloidal and hypertrophic scar tendency
5. Patients with platelet disorders, anemia or bleeding disorders.
6. Immunocompromised patients like HIV, Hepatitis B or C positive
7. Patients who have active skin disease/infection at treatment area.
8. Un-cooperative patients or patients unable to understand the protocol or give informed consent
Methods
1. Ethical clearance from the institutional ethics committee
2. Informed written consent
3. Pre-structured proforma
4. Preoperatively, patients will be assessed and,
5. Investigated with routine investigations and special investigations when required.
Procedure
Step 1: Under strict aseptic precautions, after shaving and surgical preparation of donor and recipient areas, a topical eutectic anaesthetic mixture of prilocaine and xylocaine is applied under occlusion for 45 minutes on both donor and recipient areas.
Step 2: A split thickness thin skin graft is harvested from anterior thigh, using a skin grafting blade inserted into Humby’s knife. After the graft is harvested, hemostasis is achieved on donor site and dressing done.
Step 3: The harvested graft is placed in a petridish containing 5 ml of 0.2% trypsin+0.8% ethylene diamine tetra acetic acid solution.
Step 4: Graft is soaked completely in the solution and spread out with epidermal surface facing upwards, and then cut into smaller pieces.
Step 5: Graft is incubated in an incubator at 37 °C for 50 minutes.
Step 6: After 50 min, trypsin solution is neutralized by 5 ml of 0.5% trypsin inhibitor.
Step 7: Dermis is teased out from the epidermis and discarded.
Step 8: Epidermis pieces are transferred to a test tube containing Dulbecco’s modified eagle’s medium (DMEM).
Step 9: The test tube with epidermal cells is centrifuged for 6 minutes at 2000 rpm to obtain a pellet-rich in cells.
Step 10: The pellet is resuspended in DMEM and transferred to a pipette, ready for application on to recipient area.
Step 11: The recipient area is abraded with a micromotor dermabrader fitted with diamond fraise wheel till uniform pinpoint bleeding appears.
Step 12: The cell suspension is spread evenly on the dermabraded area through a pasteur pipette and covered with collagen dressing, then by sterile gauze soaked in DMEM solution, followed by occlusive TEGADERM transparent film dressing and finally by adhesive crepe bandage.
Step 13: Patients are instructed to take complete rest and avoid all vigorous physical activities. Oral antibiotics and NSAIDs are prescribed for 1 week.
Step 14: Dressings are removed after one week.
Step 15: Patients are followed up at 1 week, 1 month, 3 months, 6 months.
Post-operative assessment was done by subjective assessment, scoring systems and digital photography.
Digital photographs were taken before procedure, then after 1 week on removal of dressing, after 1 month, after 3 months and finally after 6 months of procedure.
Subjective assessment was done by asking patients to evaluate repigmentation as follows: 0-25%=Poor; Good=26-75%; Excellent=76-100% [4].
Objective assessment was done by the following scoring system (Table 1) [5].
| Criteria for evaluation | Score | Factor | Total | |||
| 0 | 1 | 2 | 3 | |||
| A. Extent of pigmentation | <50% | 51%-70% | 71-90% | >90 | X5 | |
| B. Color match * | Poor | Good | Excellent | X3 | ||
| C. Complications (Recipient area)** | Minimal cobblestone/variegated appearance | Moderate to marked cobblestone/variegated appearance, milia | Thick graft margins, wrinkles over graft, tyre-patch appearance | Keloid hypertrophic scar | X-3 | |
| D. Complications (donor area)** | Minimal hypo/hyper pigmentation, minimal scarring | Moderate hypo/hyper pigmentation, moderate scarring | Gross hypo/hyper pigmentation, unsightly scarring | Keloid depigmentation | X-2 | |
| Results: 17-21-Excellent; 12-16-Good; 7-11-Fair; 6 or less-poor | ȣ (A+B+C+D) | |||||
*Excellent color match-minimal hypo or hyper pigmentation of grafted area not requiring camouflage.
Good color match-moderate hypo or hyperpigmentation amenable to light camouflage.
Poor color match-gross hypo or hyperpigmentation difficult to cover up with ordinary makeup.
** In presence of complications belonging to more than one score, only the highest score should be multiplied by the factor.
Table 1: Scoring system for evaluation of results of autologous transplantation methods in vitiligo.
Extent of pigmentation was assessed and classified into [6].
Excellent if>90% repigmentation
Good if 70-89% repigmentation
Fair if 30-69% repigmentation
Poor if<30% repigmentation
The data has been collected and analysed in an excel sheet. Proportions are calculated for the data.
On removal of dressing on the recipient area, crusted scabs were seen partially attached to dermabraded area, along with erythematous achromic areas. Repigmentation usually started by 2-3 weeks and was complete within 6 months in most of the patients. Earliest onset of pigmentation was observed within 10 days with pin-point pigmentation. In some patients with perifollicular type of repigmentation, initially islands of pigmentation was seen which later coalesced to form uniform repigmentation. Whereas in other patients, diffuse pigmentation was seen in central part of vitiliginous area, then gradually spread to pigment surrounding margins.
Repigmentation was rapid and maximum in initial 3-4 months, and then slowed in the following months (Figures 1-6).
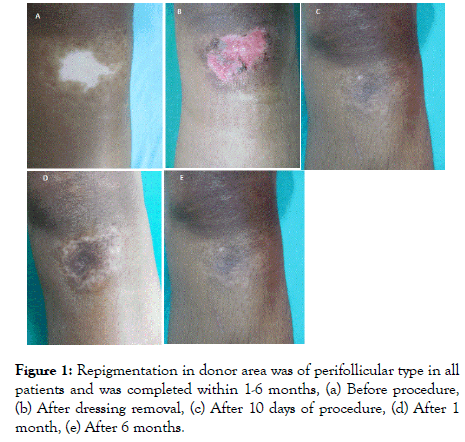
Figure 1: Repigmentation in donor area was of perifollicular type in all
patients and was completed within 1-6 months, (a) Before procedure,
(b) After dressing removal, (c) After 10 days of procedure, (d) After 1
month, (e) After 6 months.
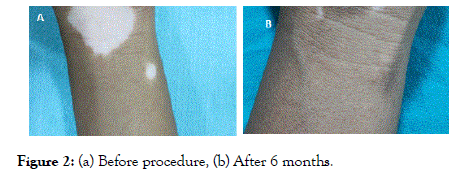
Figure 2: (a) Before procedure, (b) After 6 months.
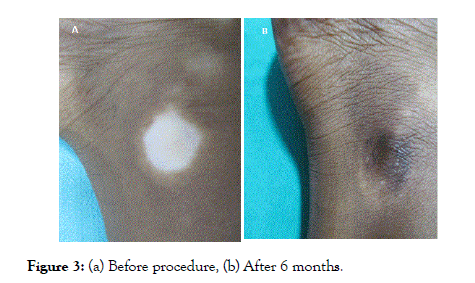
Figure 3: (a) Before procedure, (b) After 6 months.
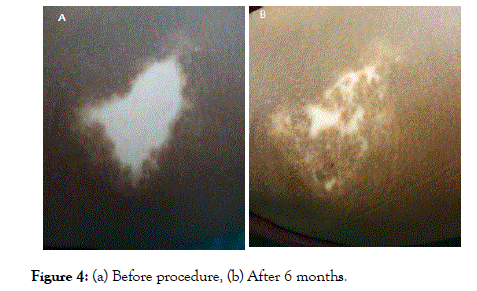
Figure 4: (a) Before procedure, (b) After 6 months.
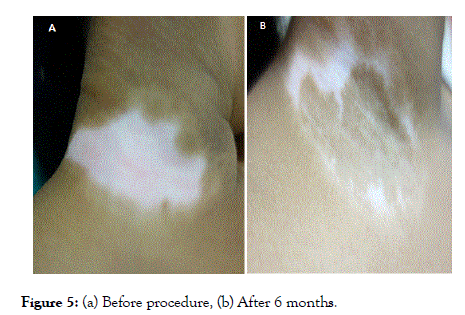
Figure 5: (a) Before procedure, (b) After 6 months.
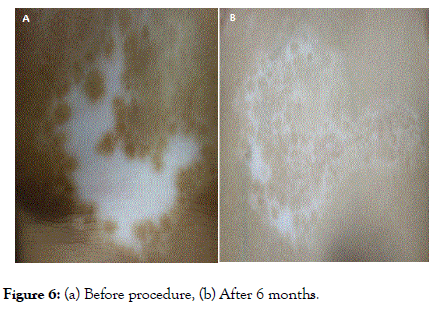
Figure 6: (a) Before procedure, (b) After 6 months.
This procedure is also known by other names like non-culture melanocyte transfer, basal cell suspension technique, nonculture cellular transplant [5-7].
The principle is seeding of melanocytes i.e. introduction of melanocytes from normal skin into a region of depigmented skin [8]. The basic principle is to separate the basal cells and the melanocytes by trypsinization, and prepare a suspension which is applied on the dermabraded lesional skin [9]. During the initial 7 days of healing, melanocytes and keratinocytes present in the grafted material, multiply and repigment the depigmented area. Further pigmentation can be accelerated by topical psoralen therapy [9], NBUVB and PUVA. However, some authorities use phototherapy only if there is delay in onset of repigmentation [6,10]. Pigmentation in the treated areas gradually increases in size due to melanocyte proliferation and migration under the influence of cytokines secreted by surrounding keratinocytes. Hence, melanocytes taken from a small donor can pigment a much larger recipient area [9].
A total of 30 patients were included in this prospective longitudinal study and followed up at 1 month, 3 months and 6 months. All patients completed the study.
Age
Study group was in the age group of 12-50 years. The youngest patient was 12 years old and oldest was 50 years old.
Sobhy et al. [11], study showed the age of 20 patients varied between 13 and 33 years, highest proportion of studied patients was 60% in age group<15 years, and lowest was 40% in age group 15-33 years.
Sex
Slight preponderance of females was seen with females 66.7% (20), and males 33.3% (10).
Verma et al. [12], in their study, non-cultured melanocyte technique group included 47.4% (9) females and 52.6% (10) males while Sobhy et al. [11] study showed 13 female and 7 male patients.
Duration of stability
In the present study, percentage of patients with stable disease for 1 year was 3.3% (1) patient, with stability for 2 years was 23.3% (7) patients, with stability for 3 years was 16.7% (5) years, with stability for 4 years was 26.7% (8) patients, with stability for 5 years was 13.3% (4) patients, stability for 6 years was 10% (3) patients, stability for 7 years was 3.3% (1) patient, stability for 10 years was 3.3% (1) patient.
Sobhy et al. [13] found that the most important variable is the stability of the disease (2 years or more) rather than the duration of the disease. But, in the present study, patients with stability less than 2 years were also included according to IADVL task force guidelines regarding the stability.
Associated diseases
In this study, association with only thyroid disease has been noted, 83.3% (25) patients had normal thyroid function tests, whereas 16.7% (5) patients had abnormal thyroid function tests. All 5 patients with abnormal thyroid function tests were females.
Subjective assessment
After follow-up at 6 months, 10% (3) showed poor response, 30% (9) showed good response and 60% (18) patients showed excellent response.
Objective assessment
After follow-up at 6 months, 10% (3) showed poor response, 13.3% (4) showed fair response and 23.3% (7) patients showed good response, 53.3% (16) patients showed excellent response.
Gauthier [14] in study has reported incomplete repigmentation in 20% of patients, probably due to type of vitiligo.
Extent of pigmentation
After follow-up at 6 months 10% (3) showed poor response, 10% (3) showed fair response and 20% (6) patients showed good response, 60% (18) patients showed excellent response.
Paul [6] has reported excellent repigmentation in 65% (32) patients, 18% (9) patients had good repigmentation, 8% (4) patients each had fair and poor repigmentation. 79% (39) patients had excellent colour and texture matching.
Pandya et al. [15], have reported excellent response in 52.2% (12) patients.
Sobhy et al. [11], reported excellent repigmentation 35% test sites, good repigmentation in 55% sites, fair repigmentation in 10% sites and did not report poor repigmentation at any site.
Rajesh et al. [12] reported good repigmentation in 62% (31) patients, 20% (10) patches as fair repigmentation, 18% (9) patches with poor repigmentaion.
Age at presentation versus extent of pigmentation at 6 months
At the end of 6 months, excellent repigmentation was seen in 100% (5) patients in age group 11-20 years.
In this study, it was observed that repigmentation was better and occurred earlier in younger patients than in older patients.
Sobhy et al. [11], also reported earlier repigmentation and better prognosis in age group<15 years than in older patients, probably due to younger cell that grows and multiplies rapidly.
Czajkowski [9], also has found that the time of proliferation of melanocytes in in vitro culture conditions depends on the age of the patient and, younger the patient, faster is the melanocytes proliferation.
In the present study, by subjective assessment, 10% (3) patients showed poor response, 30% (9) showed good response and 60% (18) patients showed excellent response after follow-up at 6 months with good patient satisfaction. By objective assessment 10% (3) patients showed poor response, 13.3% (4) showed fair response and 23.3% (7) patients showed good response, 53.3% (16) patients showed excellent response after follow-up at 6 months. Extent of repigmentation was evaluated as-10% (3) showed poor response, 10% (3) showed fair response and 20% (6) patients showed good response, 60% (18) patients showed excellent response after follow-up at 6 months. Repigmentation was uniform, matched well with surrounding skin and usually completed within 6 months. Cosmetic acceptability is also superior as there is no cobble-stoning or scarring seen in other methods, giving good patient satisfaction. The study confirms that repigmentation by autologous non-cultured epidermal cell suspension in stable vitiligo is a safe, effective, and simple method, with superior quality of repigmentation, very few adverse effects and high level of patient satisfaction with possibility to repigment vitiliginous skin manifold larger than the donor skin
Citation: Thejaswi C, Madhavilatha M (2019) High Frequency Ultrasound in Aesthetic Dermatology Novel Research for the use of 18 MHz Shearwave Elastography for Pre and Post Therapy Assessment: A Pilot Study. J Clin Exp Dermatol Res. 10:497. doi: 10.35248/2155-9554.10.497
Received: 02-Apr-2019 Accepted: 16-Apr-2019 Published: 23-Apr-2019 , DOI: 10.35248/2155-9554.10.497
Copyright: © 2019 Thejaswi C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited