
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2020)Volume 11, Issue 3
Objective: Continuous administration of opioids is a common approach after cardiac surgery. However, this method may be associated with a higher incidence of delirium. The present study aimed to evaluate the influence of two administration methods- continuous administration of fentanyl in combination with acute administration of fentanyl and acetaminophen vs. a combination of acute administration of fentanyl and acetaminophen only- on the incidence of delirium after cardiac surgery.
Methods: This retrospective observational cohort study enrolled 184 adult patients from 201 prospective participants who underwent elective cardiac surgery. After intensive care unit (ICU) admission, patients were divided into two groups: One group (group S) received administration of acetaminophen (15 mg·kg-1 with a 6 hours lockout time). If administration of acetaminophen was not sufficient to control pain (numerical rating scale (NRS) score>3) throughout the lockout time, a single dose of fentanyl (25 μg bolus and 30 m lockout time) was administered. The other group (group C) began continuous administration of fentanyl (25 μg·h-1) immediately after ICU admission, and acetaminophen (l5 mg·kg-1 and 6 h lockout time) was administered using the same protocol used for group S. For all patients, the incidence and duration of delirium and NRS scores were recorded.
Results: The incidence of delirium in group S was lower than that in group C (3.0% vs. 12.0%, p=0.021). Patients belonging to group S experienced a shorter duration of delirium than those in group C (8 vs. 20 hours, p=0.042). The NRS scores after ICU admission did not differ significantly between the two groups.
Conclusion: Continuous administration of postoperative fentanyl may cause an increased risk of postoperative delirium and prolong its duration. The combination of only acute administration of fentanyl and acetaminophen may be preferable because it reduces the frequency of postoperative delirium in cardiac surgery patients.
Continuous administration; Drug administration; Fentanyl; Acetaminophen; Delirium; Intensive care delirium screening checklist; Pain control; Numerical rating scale
Postoperative pain relief is a major medical challenge. Poorly managed postoperative pain, especially following cardiac surgery, can also increase postoperative complications and impair recovery [1]. Several treatments have been proposed for postoperative pain management, including continuous administration of opioids, thoracic epidural analgesia, and paravertebral block [2]. Continuous administration of opioids is more common than thoracic epidural analgesia and paravertebral block because of the bleeding associated with heparin administration after cardiac surgery. However, several reports have indicated that the incidence of prolonged delirium is higher when an opioid is administered than when it is not [3,4]. Rudolph et al. reported that 50% of cardiac surgical patients had delirium [5]. Delirium is associated with short-term complications, such as sternal dehiscence and infection, and long-term complications, such as cognitive disorders and dementia [6,7]. Therefore, decreased administration of opioids is desirable because opioids can cause delirium if excessive doses are used. However, the postoperative increases in pain levels are independent predictors of the development of postoperative delirium. Recently, several studies have reported the effect of intravenous drip (IV) acetaminophen after cardiac surgery [8,9]. However, there have been no reports on whether continuous administration or single doses of fentanyl is more effective when combined with acetaminophen after cardiac surgery. We hypothesized that a combination of only acute administration of fentanyl and acetaminophen would provide better postoperative management of delirium and pain than that achieved with continuous administration of fentanyl following cardiac surgery. Therefore, we retrospectively evaluated the effects of these two administration methods on postoperative pain management and other clinical outcomes after cardiac surgery.
This investigation was a single-center retrospective observational study conducted between November 2016 and March 2018 at Kanazawa University Hospital. Ethical approval for the present study (approval number: 2632) was obtained from the Ethics Committee of the Institutional Review Board of the Kanazawa University School of Medicine, Kanazawa, Japan on November 3, 2017. Because the present study involved a retrospective analysis of in-patient charts and anesthetic report data from a concurrently recorded computerized database, the Ethics Committee of Kanazawa University Hospital waived the need for informed consent. We will instead release information regarding the present study to the public on an opt-out basis.
Inclusion criteria
The present study included patients undergoing cardiac surgical procedures, such as coronary artery bypass grafting (CABG), heart valve surgeries, and aortic surgery through a primary full median sternotomy. We included patients who had an American Society of Anesthesiologists physical status (ASA-PS) of fewer than 3.
Exclusion criteria
characteristics: an ASA-PS of 4 or 5, a Glasgow Coma Scale score<15, patients with a history of or current undergoing dialysis, or severe liver damage (Child-Pugh grade B or C). We also excluded patients receiving preoperative opioids, a central nervous depressant (phenothiazine or barbiturates), a narcotic antagonist analgesic (buprenorphine or pentazocine), monoamine oxidase inhibitors, tricyclic antidepressants, or antihistamine medications. Furthermore, patients who underwent emergency surgery or surgery without a median sternotomy were excluded.
Anesthesia procedure
Anesthesia was induced with midazolam and fentanyl over a 60 s period. After rocuronium was administered for muscle relaxation, tracheal intubation was performed. Anesthesia was then maintained with fentanyl and/or remifentanil, sevoflurane, and/or propofol infusion. Five-lead ECG, pulse oximetry, invasive arterial and pulmonary artery pressure, and bispectral index measurements were monitored through IntelliVue MX8OOTM (Royal Philips, Amsterdam, Netherlands). The volume of fluids, the number of transfusions, and the doses of vasopressors administered during the operation were calculated from medical records. Immediately after the operation, all patients were moved to the ICU. They were then extubated after demonstrating functional recovery, and hemodynamic and respiratory stability, as determined by their respective attending physicians.
Strategy for postoperative pain control
In the present study, patients were divided into two groups based on the pain management they received. One group (group S) received administration of acetaminophen (15 mg·kg-1 with a 6 hours lockout time). If administration of acetaminophen was not sufficient to control pain (NRS>3) throughout the lockout time, a single dose of fentanyl (25 μg bolus and 30 m lockout time) was administered. The other group (group C) began continuous administration of fentanyl (25 μg·h-1) immediately after ICU admission, and acetaminophen (l5 mg·kg-1 and 6 hours lockout time) was administered using the same protocol used for group S (Figure 1). The primary outcome was the incidence of delirium after extubation during a patient’s ICU stay. Delirium was measured using the Intensive Care Delirium Screening Checklist (ICDSC) scores obtained 12 hours postextubation to ICU discharge. Secondary outcomes were as follows: total doses of dexmedetomidine and Propofol, time to extubation, total post-surgical dose of fentanyl, total time of continuous administration of fentanyl, total doses of acetaminophen, NRS score 8 hours after extubation, incidence of postoperative nausea and vomiting (PONV) and constipation, and the total length of ICU stay.
Nurses evaluated the ICDSC and numerical rating scale (NRS) scores in the ICU. PONV was defined as the occurrence of at least one episode of nausea or vomiting within the first 24 hours after extubation, where vomiting was defined as the expulsion of gastric content. Constipation was defined as a failure of the bowel to open for three consecutive days [10]. Nurses in the ICU monitored patient symptoms and collected these data. The total length of ICU stay was collected from the patient’s electronic chart.
Statistical analyses
Continuous data are described as medians (interquartile range [IQR]) or frequencies and proportions, depending on the variable type and distribution. Changes between groups are further presented as differences and 95% confidence intervals. Categorical variables are presented as numbers and percentages. Continuous data were compared between groups by using a parametric t-test, and non-parametric Wilcoxon Rank Sum or Kruskal-Wallis tests, as appropriate. Differences in categorical variables, including the primary outcome (incidence of delirium), were assessed with a χ2 test (or a 2-tailed Fisher exact test when cell counts were small). NRS scores (0, 8, 16 and 24 hours after extubation) across time points were compared between the two groups by using a repeated-measures analysis of variance. p values<0.05 were considered statistically significant. The Statistical Package for the Social Sciences (Version 23, IBM Inc., Armonk, NY, USA) was used for all analyses.
A total of 201 individuals were assessed for eligibility. Seventeen subjects were not enrolled: three because of aborted surgeries and fourteen because of our exclusion criteria. More specifically, these patients were excluded for the following reasons: two had an ASA-PS of 4, seven were undergoing, or had undergone, dialysis, and five had had surgery without a median sternotomy. In total, 184 patients were included, of which 101 were treated with a single administration of fentanyl or an infusion of acetaminophen (group S), and 83 received continuous administration of fentanyl (group C) (Figure 1).
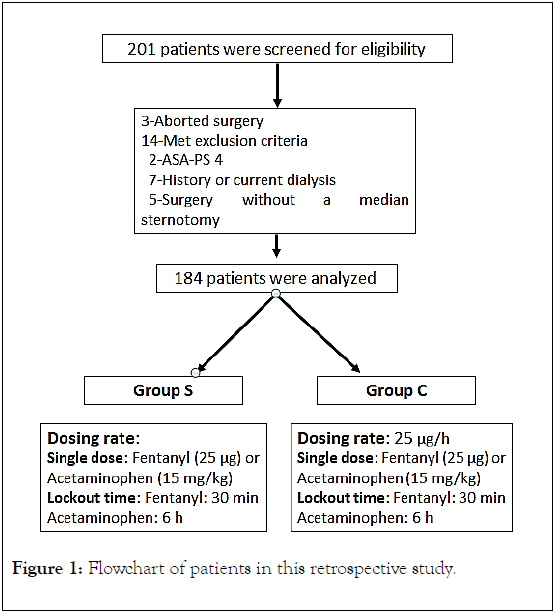
Figure 1. Flowchart of patients in this retrospective study.
The characteristics of the S and the C groups are summarized in Table 1. Age, sex, and comorbidities were not significantly different between the two groups. All patients were classified as ASA-PS 3. The distribution of the operative procedures was coronary artery bypass grafting (CABG) (35%), heart valve surgeries (53%), and aortic surgery (12%). The operative and anesthetic duration were not different between the two groups.
| Demographics | Group S (n=101) | Group C (n=83) | p value |
|---|---|---|---|
| Male | 76 (75.2) | 59 (71.1) | |
| Female | 25 (24.8) | 24 (28.9) | |
| Age, median (IQR), yr | 70 (65-75) | 69 (63-77) | |
| Height, median (IQR), cm | 163 (155-168) | 163 (157-168) | 0.668 |
| Weight, median (IQR), kg | 60 (52-71) | 64 (52-73.5) | 0.695 |
| Hypertension, No. (%) | 44 (43.6%) | 39 (46.9%) | 0.658 |
| Diabetes, No. (%) | 15 (14.9%) | 9 (10.8%) | 0.512 |
| Hyperlipidemia, No. (%) | 32 (31.7%) | 28 (33.7%) | 0.875 |
| Asthma, No. (%) | 4 (4.0%) | 5 (6.0%) | 0.734 |
| History of stroke, No. (%) | 10 (9.9%) | 11 (13.2) | 0.494 |
| Surgical characteristics | |||
| Procedure, No. (%) | |||
| AVR | 31 (30.7%) | 22 (26.5%) | 0.624 |
| MVR | 10 (9.9%) | 11 (13.3%) | 0.494 |
| MVP | 10 (9.9%) | 13 (15.7%) | 0.268 |
| CABG | 37 (44.6%) | 28 (33.7%) | 0.757 |
| Aortic surgery | 13 (12.9%) | 9 (10.8%) | 0.82 |
Abbreviations: C: Continuous use of fentanyl; S: Single administration of fentanyl; M/F: Male/female; ASA-PS: American Society of Anesthesiologists Physical Status classification; AVR: Aortic Valve Replacement; MVR: Mitral valve replacement; MVP: Mitral Valvuloplasty; CABG: Coronary Artery Bypass Grafting; IQR: Interquartile Range
Table 1: Preoperative and operative patient data.
The intraoperative doses of sedatives and analgesic agents were also not different (Table 2).
| Group S | Group C | Differences (95% CI) | p value | |
|---|---|---|---|---|
| 333 (268-383) | 316 (252-391) | 17 (-15 to 39) | 0.398 | |
| Anesthetic duration, median (IQR), y | 427 (357-479) | 414 (348-493) | 13 (-26 to 35) | 0.774 |
| Intraoperative midazolam dose, median (IQR), mg | 8 (6-10) | 8 (6-10) | 0 (-1.0 to 0.3) | 0.252 |
| Intraoperative fentanyl dose, median (IQR), μg/kg | 24.1 (16.1-25.7) | 24 (16-28.8) | 0.1 (-4.4 to 2.2) | 0.501 |
| Intraoperative remifentanil dose, median (IQR), μg/kg | 0.3 (0-1.3) | 0.4 (0-1.05) | -0.1 (-0.23 to 0.27) | 0.879 |
| Bleeding, median (IQR), mL | 2030 (1430-2600) | 1600 (985-2475) | 430 (-209 to 478) | 0.440 |
Abbreviations: C: Continuous use of fentanyl; S: Single administration of fentanyl; IQR: Interquartile range.
Table 2: Patient intraoperative profiles.
In the postoperative phase, the total dose and duration of propofol and dexmedetomidine administrations did not differ significantly between the two groups. However, the time to extubation in group S was shorter than that in group C (median 4 vs. 6 hours, respectively; difference, -2 hours; 95% CI: -6.8 to -1.8 hours, p<0.001). Patients belonging to group S showed a significantly lower incidence of delirium, the primary outcome, than the patients in group C (3.0% vs. 12.0%; difference, -9.0%; 95% CI: -26.0% to 1.1%; p=0.021). Patients belonging to group S experienced a shorter duration of delirium than patients in group C (median duration of 8 vs. 20 h, respectively; difference, -12 hours; 95% CI: -18.1. to 0.5 h; p=0.042). The occurrence of constipation did not differ between the two groups. PONV in group S was significantly lower than that in group C (5.0% vs. 14.5%; difference, -9.5%; 95% CI: -12.2% to 1.0%; p=0.039), and the length of ICU stay in group S was shorter than that in group C (median (IQR), 4 vs. 5; difference, -1 days; 95% CI, -1.4 to 0.4; p < 0.001; Table 3). The NRS scores after ICU admission did not differ significantly between the two groups at 0, 8, 16, or 24 h after extubation (Figure 2).
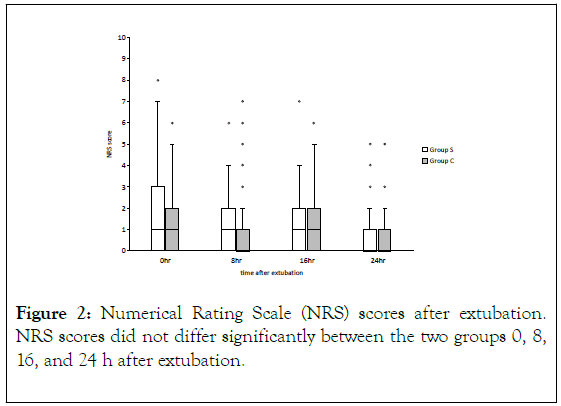
Figure 2. Numerical Rating Scale (NRS) scores after extubation. NRS scores did not differ significantly between the two groups 0, 8, 16, and 24 h after extubation.
| Group S | Group C | Differences (95% CI) | p value | |
|---|---|---|---|---|
| Delirium, No. (%) | 3 (3.0%) | 10 (12.0%) | -7.0% (-26.0% to -1.1%) | 0.021 |
| Duration of delirium, median (IQR), h | 8 (8-12) | 20 (16-24) | -12 (-18.1 to -0.5) | 0.042 |
| DEX dose, median (IQR), μg/kg/min | 0.2 (0.2-0.3) | 0.2 (0.2-0.3) | 0 (-0.03 to 0.03) | 0.943 |
| Total time of DEX median (IQR), h | 14 (10-17) | 14 (12-17.5) | 0 (-3.5 to 2.3) | 0.706 |
| Propofol dose, median (IQR), μg/kg/min | 0 (0-0.5) | 0 (0-0.8) | 0 (-0.18 to 0.16) | 0.939 |
| Total time of use of propofol median (IQR), h | 0 (0-4) | 0 (0-3) | 0 (-2.2 to 2.0) | 0.935 |
| Time to extubation, median (IQR), h | 4 (5-7) | 6 (4-16.5) | -2 (-6.8 to -1.8) | <0.001 |
| Total postsurgical continuous dose of fentanyl (μg) | - | 750 (650-950) | - | - |
| Total time of continuous use of fentanyl, median (IQR), μg/kg/min | - | 30 (26-38) | - | - |
| Total dose of acetaminophen, median (IQR), mg | 1000 (600-1400) | 600 (0-900) | 400 (421 to 835) | <0.001 |
| Total rescue dose of fentanyl, median (IQR), μg | 0 (0-25) | 0 (0-13) | 0 (-2.0 to 11.0) | 0.177 |
| PONV, No. (%) | 5 (5.0%) | 12 (14.5%) | -9.5% (-12.2% to -1.0%) | 0.039 |
| Constipation, No. (%) | 43 (42.6%) | 38 (45.8%) | -3.2% (-0.58 to 2.1) | 0.881 |
| Total length of ICU stay, median (IQR), days | 4 (3-5) | 5 (4-6) | -1 (-1.4 to -0.4) | <0.001 |
Abbreviations: C: Continuous use of fentanyl; S: Single administration of fentanyl; DEX: Dexmedetomidine; PONV: Postoperative Nausea and Vomiting; ICU: Intensive Care Unit; NRS: Numerical Rating Scale; IQR: Interquartile range.
Table 3: Primary and secondary outcomes.
The incidence of delirium in group S was lower than that in group C after extubation, despite equivalent sedation levels. Additionally, time to extubation, delirium duration, and length of ICU stay in group S were also shorter than those in group C. In group C, the median total postsurgical continuous dose of fentanyl was 750 μg, and the median total time of continuous use of fentanyl was 30 h. The total rescue dose of fentanyl was not significantly different between the two groups in the postoperative period. On the other hand, the total dose of acetaminophen was higher in group S. NRS scores also showed no difference between the two groups. The PONV incidence in group S was lower than that in group C.
It is well known that postoperative pain adversely affects physical functioning, recovery, and quality of life, which in turn often interact with one another, leading to a wide variety of postoperative complications, such as dysfunction of the nervous, respiratory, circulatory, gastrointestinal, and hematic systems, as well as infection [11-13]. Careful postoperative pain management is, therefore, essential. Although continuous administration of opioids theoretically maintains more consistent blood opioid levels, and thus yield more stable analgesic effects than administration of single doses, postoperative pain in both groups was well controlled, as indicated by median NRS scores of less than 3. Our results demonstrate that a combination of a single dose of fentanyl and acetaminophen can provide postoperative pain control equivalent to the continuous administration of fentanyl after cardiac surgery. Furthermore, the incidence of delirium after cardiac surgery was significantly reduced in this paradigm. Subramaniam et al. have reported similar results [9]. However, direct comparisons with our results are difficult because they used morphine, hydromorphone, and oxycodone, as well as fentanyl and acetaminophen in their study. Our study used only fentanyl and acetaminophen as analgesic agents. Therefore, our results indicate that a single dose (as rescue) of fentanyl is effective and acetaminophen can substitute for continuous administration of fentanyl, which reduces the risk of delirium without compromising post-surgical pain management.
We were able to assess delirium at 8 h intervals instead of daily intervals by using ICDSC in this study. This revealed that the median duration of delirium in group S was 8 h post-extubation, while the corresponding value for group C was 16 h postextubation. Subramaniam et al. also indicated that the median duration of delirium was one day [9]. However, our study suggests that the duration of delirium may be shortened by the administration of single doses of fentanyl and acetaminophen for postoperative pain management.
Although the present study contributes significantly to the literature, it also has several critical limitations that warrant discussion. First, we utilized only the ICDSC as a metric to assess postoperative delirium. However, other instruments, such as the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU), could also have been used [14]. The ICDSC and the CAM-ICU are the most well-known and widely used instruments to diagnose delirium [15]. While the CAM-ICU is sensitivity (93%) and specificity (89%) for the diagnosis of delirium [16], the ICDSC in ICU patients has been shown to be more sensitive (99%) but less specific (64%) than the CAM-ICU [15]. However, this difference may not be entirely accurate because there are no documented differences between the ICDSC and CAM-ICU in their assessments of postoperative pain [17].
Second, patients in our study were administered acetaminophen and fentanyl. Therefore, correlations between postoperative delirium and acetaminophen, as well as other agents, should be taken into account both in our results and in future work. Finally, this strategy for postoperative pain control was developed in our ICU. Furthermore, the present study utilized a retrospective, observational design; these are both critical limitations. Therefore, future multi-center, randomized clinical trials are needed to complement the pilot data obtained from our single-center, nonrandomized study to identify methods for minimizing the incidence of delirium without compromising post-surgical pain management.
Continuous administration of postoperative fentanyl may cause an increased risk of postoperative delirium and prolong its duration. Acute administration of fentanyl in combination with acetaminophen may be preferable because they reduce the incidence of postoperative delirium in postoperative cardiac surgery patients.
Citation: Tennichi T, Taniguchi T (2020) A Single-Center Retrospective Observational Cohort Study on Postoperative Pain Management: Better with Continuous Or Single Doses of Fentanyl With Acetaminophen? J Anesth Clin Res. 11:940. DOI: 10.35248/2155-6148.20.11.940.
Received: 25-Feb-2020 Accepted: 10-Mar-2020 Published: 17-Mar-2020 , DOI: 10.35248/2155-6148.20.11.940
Copyright: © 2020 Tennichi T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.