Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2020)Volume 11, Issue 2
Sensitive skin syndrome; albeit reported in many countries worldwide; remained a condition of unknown etiology and pathogenesis. Some authorities speculate it as a skin condition continuum from mild to severe, its severity is difficult to assess. Our retrospective study aimed to draw a one- year new patient’s attendee clinical data comparing the patient self -reported percepts using a validated sensitive scale questionnaire between dermatologist diagnosed skin conditions in a private clinic setting including sensitive skin syndrome. The results suggested that allergic contact dermatitis, herpes zoster and sensitive skin syndrome diagnosed patients reported a similar mean Sensitive Scale-10 scores {46.07 (N= 91), 40.72 (N=35) and 41.38 (N=84); p >0.05} respectively. The mean SS 10 score was statistically significantly different from other skin conditions like atopic dermatitis and seborrhea dermatitis and control. The patterns of percepts distribution in terms of skin irritation, general discomfort, skin itchiness, tautness and pain between allergic contact dermatitis, herpes zoster and sensitive skin syndrome were similar. Though pain is more commonly reported it herpes zoster than itch. As how a patient perceives their somatic symptoms is one of the major reasons for their dermatology health seeking behavior, our study suggested that extreme acute form of sensitive skin syndrome may have a patient percepts similar to allergic contact dermatitis, herpes zoster psychosocially significantly affecting quality of life of the sufferers.
Sensitive skin syndrome; Severity; Percepts; Biopsychosocial model; Validated sensitive scale-10 questionnaire; Allergic contact dermatitis; Herpes zoster; Health seeking behavior
Percept is an impression or sensation of something perceived by an individual. It is the mental products of perceiving [1,2]. Unpleasant percepts; maybe referred as dermatological symptoms like skin sensitivity, discomfort, itchiness, tautness and pain are the main causes of patient’s health seeking behavior and visiting dermatologists. How an individual perceived their symptoms was important influenced by multiple factors like personality, external stress, positive placebo or negative nocebo effects and social support. This biopsychosocial model had been shown to be pivotal in many skin diseases influencing somatic symptoms like the sensation or suffering itch through a psychoneurobiological mechanism [3-6].
In our study, data from a previously carried out pilot investigation on the prevalence of sensitive skin syndrome (SSS) in clinic setting was retrieved (period: 1st May 2018 to 31st April 2019) [7]. The sensitive scores of a dermatologist diagnosed inflammatory and non-inflammatory skin conditions using a validated sensitive scale questionnaire (SS-10) in SSS were collected, analyzed and compared with the sensitive scores of SSS. The objective of the study was to collect background data of patient ’ s perceived symptoms and sensitive scores using a validated questionnaire and compare other dermatologist diagnosed skin condition with SSS; a condition still with an undefined pathophysiological mechanism and unclear relationship with other known skin dermatosis like allergic contact dermatitis, atopic dermatitis, urticaria, acne vulgaris and herpes zoster.
The survey complied to the ethical principles of the Helsinki declaration (1983). Voluntary consents were obtained from the interviewees and the self-reported questionnaire posed no mental risks to the participants.
The objective of this study was to compare the sensitive scores reported by the patients attending the private clinic in different types of dermatologist diagnosed eczematous skin conditions like atopic dermatitis, allergic contact dermatitis and non eczematous skin conditions like rosacea, seborrhea eczema, urticaria, acne vulgaris, psoriasis and infective skin conditions like herpes zoster and tinea infection using a sensitive scale questionnaire validated for SSS [8].
The sensitive scores (SS-10 scores) were measured with a validated patient self-reported sensitive scale questionnaire (SS-10) translated in Chinese version [7,8]. It was used previously to assess the severity of SSS and it has a good content validity captures the cores percepts or symptoms of sensitive skin especially in SSS. The Chinese version of the SS-10 had been used previously to assess the sensitive scores of who suffered from SSS and in a clinic based and community-based setting [7,9]. The collected data were used to determine the cutoff value of diagnosing SSS using the validated SS-10 questionnaire using the receiver operating characteristics curve estimation. The reports were presented and published [10]. SS-10 has been tested in more than 10 countries globally and had demonstrated good psychometric characteristics in measuring sensitive skin. SS-10 was reported to have a high correlation with Dermatology Life Quality Index (DLQI).
SS-10 scores were used as an estimate of skin sensitivity as many skin conditions like allergic contact dermatitis, urticaria, tinea infection and herpes zoster described by clinic attendees as unpleasant percepts and somatic symptoms like sensations of itch, pain and skin discomforts as sensitive skin.
During the period of 1st May 2018 to 31st April 2019 in a private dermatology clinic, all newly attended patients (N=1111) were asked voluntarily to fill in a validated SS-10 questionnaire. The SS-10 scores were recorded for all these clinic attendees and their clinical notes would record their respective clinical diagnosis by a dermatologist. The original aim of the study was to collect the sensitive scores of clinically diagnosed SSS in clinic. Since the data set also included newly patient attendees diagnosed by dermatologist having eczematous skin conditions like atopic dermatitis, allergic contact dermatitis and non eczematous skin conditions like rosacea, seborrhea eczema, urticaria, acne vulgaris, psoriasis and infective skin conditions like herpes zoster and tinea infection; an evaluation and comparison of the sensitive scores among these condition and SSS became feasible. The data set with the SS-10 scores with the corresponding clinically diagnosed skin condition were retrieved, recorded and analyzed retrospectively.
The number of patient dermatologist diagnosed eczematous, non-eczematous, infective skin conditions and SSS with their corresponding average SS-10 scores were tabulated (Table 1).
| Skin condition Diagnosed by Dermatologist | Number of Patients | Mean SS-10 Scores | P<0.05 as compared with mean SS-10 scores of SSS=41.38 |
|---|---|---|---|
| Allergic Contact Dermatitis | 91 | 46.07 | NS |
| Herpes Zoster | 35 | 40.72 | NS |
| Urticaria | 34 | 31.74 | <0.05 |
| Rosacea | 26 | 26.00 | <0.05 |
| Atopic Dermatitis | 74 | 26.53 | <0.05 |
| Seborrhea Dermatitis | 33 | 23.79 | <0.05 |
| Tinea pedis | 168 | 21.22 | <0.05 |
| Acne vulgaris | 145 | 19.30 | <0.05 |
| Psoriasis | 40 | 18.77 | <0.05 |
| Control (Asymptomatic skin nodules like warts) | 368 | <10 | <0.05 |
Table 1: Total Number of Patients with a dermatological diagnosis = 1098 including patients diagnosed SSS and asymptomatic nodules, NS = non significant (p>0.05).
The mean SS-10 scores of allergic contact dermatitis, herpes zoster and sensitive skin syndrome are 46.07 (N= 91), 40.72 (N=35) and 41.38 (N=84) which is statistically insignificant.
The mean SS-10 scores recorded in the study showed statistically significant difference compared with other diagnosed skin conditions: urticaria, rosacea, atopic dermatitis, seborrhea dermatitis, tinea pedis, acne vulgaris, psoriasis. The control consisted of clinically skin nodule like warts and pigmented lesions scored less than 10 in the SS -10 scale.
Skin irritation, general discomfort, itching, tautness and pain were the commonest percepts reported in the study in ACD, HZ and SSS. Itching is still the most common percepts reported in ACD, SSS followed by HZ. Tautness followed a similar pattern. HZ reported more pain than ACD and HZ respectively.
The pattern of distribution of reported percepts was represented in Figures 1 and 2.
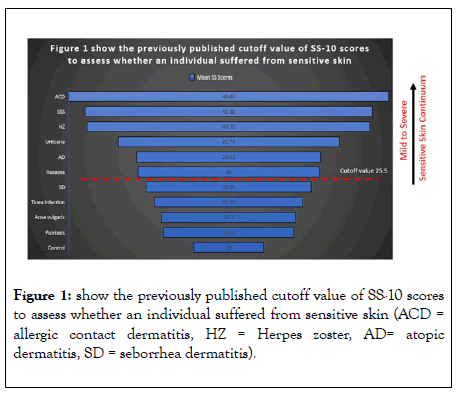
Figure 1: show the previously published cutoff value of SS-10 scores to assess whether an individual suffered from sensitive skin (ACD = allergic contact dermatitis, HZ = Herpes zoster, AD= atopic dermatitis, SD = seborrhea dermatitis).
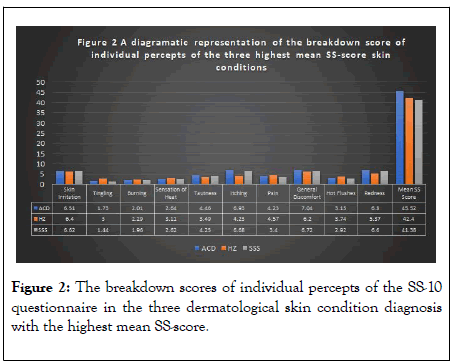
Figure 2: The breakdown scores of individual percepts of the SS-10 questionnaire in the three dermatological skin condition diagnosis with the highest mean SS-score.
Our retrospective clinical data analysis descriptively reported that in terms of patient ’ s percepts or clinically presented symptoms like skin irritation, general discomfort, skin itchiness, tautness and pain, ACD, HZ and SSS showed a similar mean SS-10 scores. This may have clinical and pathophysiological implications. Firstly, as SSS is still an undefined clinical entity, the percepts reported by patients seeking health care attention is comparable and maybe as severe as ACD and HZ which affect patient’s quality of life. Is sensitive skin a disease, a syndrome, a disorder is still debatable, our reported data showed that severe SSS was a dermatological disorder warranted clinical care and management of the suffering itch and percepts as in ACD and HZ [11]. Secondly, as the pattern of percept distribution between ACD, HZ and SSS were similar, further research and investigations focusing on similar mechanisms mediating these conditions were merited.
Based on a biopsychosocial model perspective, internal factors like personality and external stress or adverse catastrophic factors mediated by cognitive factors on how we think; e. g. negative thinking enhance a feeling of helplessness, worry and anxiety. While behavior factors like uncontrolled scratching enhance the negative percept of discomfort, irritation and itch. Finally, social factors like lack of perceived social support may work through psychoneurobiological mechanism in resulting in health seeking behavior of patients in SSS [3-6]. However, pain has been reported more in HZ compared with SSS and ACD, a neuropathic questionnaire maybe useful in assessing and comparing patients in these conditions [12,13].
Currently, International Forum for the Study of Itch (IFSI) defined SSS as a syndrome by the occurrence of unpleasant sensations (stinging, burning, pain, pruritus, and tingling sensations) in response to stimuli that normally should not provoke such sensations [14]. These unpleasant sensations cannot be explained by lesions attributable to any skin disease. Till now, no known pathogenesis and proven treatment or management care existed [15]. This definition is valid only as far as no additional data on the severity, patient ’ s percepts, behaviors and psychosocial determinants were available. If a validated cutoff value was taken as SS-10 scores=25.5 which show that many skin conditions like atopic dermatitis, urticaria, rosacea may be associated with SSS and were part of the lesser severe spectrum of sensitive skin. On the other hand, if we look at SSS as a skin condition continuum from mild to severe, our clinic-based study observed that severe SSS may have a significant disease percepts comparable to ACD and HZ with well-defined clinical diseased entity which required medical management. From this perspective, it is arguable, whether acute severe SSS with a mean SS-10 scores above 40 may be regarded as a dermatological disorder [11]. Most of the observed and diagnosed case of ACD are related to application of over the counter, patient self-purchased cosmetics containing fragrances, toiletries, cleansers and topical cosmeceutical agents applied over the face, this raise the possibility whether SSS maybe a cosmetic disorder or aggravating risk factor of ACD.
Our report has the following limitations including that it was a retrospective study retrieving information from a data set which has been already reported and published. ACD may have different types like irritant or allergic while HZ patient may present to the clinic at different stages of the diseases. However, the total number of patients studied was 1111 from a one-year period and the results were drawn from both a validated sensitive score assessment SS-10 questionnaire and a dermatologist clinical diagnosis, these may increase the validity of the results. Ways to improve or disprove the results of the study is to repeat the study with a specific aim to compare the presented percepts of these three conditions, ACD, HZ and SSS, recruiting more patients and carrying out the study in other clinical settings with both a validated sensitive skin and neuropathic questionnaire.
A retrospective study was carried out to compare the percept of patients attending a private clinic in Hong Kong within a oneyear period. The percept and symptoms reported by the clinic attendees as measured by a validated SS-10 questionnaire showed that ACD, HZ and SSS differ significantly from other skin conditions. The commonest reported skin percepts are skin irritation, general discomfort, itching, tautness and pain. ACD, HZ and SSS reported a similar pattern in the SS-10 apart pain was more commonly reported in HZ compared with ACD and HZ. A biopsychosocial model through a psychoneurbiological mechanism involving neuroendocrine mediators like cortisol, endogenous opioids and oxytocin together with a validated neuropathic questionnaire may worth further research and investigations.
Citation: Chan KTM (2020) A Retrospective Study Comparing Patient Self -Reported Percepts using a Validated Sensitive Scale Questionnaire between Dermatologist Diagnosed Skin Conditions in a Private Clinic Setting including Sensitive Skin Syndrome. J Clin Exp Dermatol Res. 11:518. DOI: 10.35248/ 2155-9554.20.11.518
Received: 25-Mar-2020 Accepted: 08-Apr-2020 Published: 15-Apr-2020 , DOI: 10.35248/2155-9554.20.11.518
Copyright: © 2020 Chan KTM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.