
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2022)Volume 13, Issue 8
Background and aim: Ultrasound-guided Serratus Anterior Plane Block (SAPB) is a novel analgesic technique used for breast and thoracic wall surgeries. The primary objective of the study was to evaluate the duration of postoperative analgesia with SAPB in Modified Radical Mastectomy (MRM) surgeries. The secondary objectives were to assess the total morphine consumption during the first 24 h, Visual Analogue Scale (VAS) score postoperatively.
Methods: After Institutional Ethical Committee approval and CTRI registration (CTRI/2019/01/017194), sixty patients undergoing MRM surgeries under general anesthesia were taken for the study with 30 patients in each group. At the end of the surgery, patients in group A were given ultrasound-guided SAPB with 20 mL 0.25% Ropivacaine with Dexamethasone 8 mg and no block was given in group B patients. Postoperatively patients were monitored continuously and assessed for VAS and vitals. PCA Morphine pump was administered for postoperative analgesia with 0.1 mg/h baseline infusion and 1 mg bolus doses with lockout interval time of 10 min. The duration of postoperative analgesia, consumption of morphine and adverse effects in the first 24 h were recorded.
Results: The duration of postoperative analgesia was prolonged in group A (1423 ± 185.55 vs. 148 ± 51.11 min, p-value <0.0001) with reduced morphine consumption (3.37 ± 0.85 mg vs. 10.7 ± 1.6 mg, p-value <0.0001). The average VAS scores were relatively lower in SAPB group. No complications were observed related to the SAP block.
Conclusion: Ultrasound-guided SAPB provided increased duration of analgesia and reduced morphine consumption following MRM surgeries in postoperative period with no complications.
Modified radical mastectomy; Postoperative analgesia; Serratus anterior plane block; Ultrasound guided; Visual analogue pain scale
Modified Radical Mastectomy (MRM) is a commonly performed surgery for loco regional control of breast malignancies worldwide. Effective management of postoperative pain increases patient satisfaction shortens the hospital stay and prevents the progression to chronic pain [1]. Pain following breast surgeries can be managed with intravenous analgesics or regional anesthesia techniques [2]. Intravenous opioids have side effects like sedation, nausea and vomiting, itching and respiratory depression. Non-steroidal anti-inflammatory drugs carry a risk for renal toxicity.
Regional anesthetic techniques have got the unique advantage of good pain relief with minimal sideeffects. Ultrasound-guided performance of these blocks increases the safety profile of the block. Thoracic Epidural Analgesia (TEA) is considered as the gold standard for postoperative analgesia but it is associated with undesirable hemodynamic changes. The regional anesthetic techniques that can provide pain relief in breast surgeries include Pectoral (PECS I and II) blocks, Thoracic Para Vertebral Blocks (TPVB), Serratus Anterior Plane block (SAPB), and Erector Spinae Plane Block (ESPB). SAPB is an interfascial plane block done above or below the serratus anterior muscle in the midaxillary line to block the lateral cutaneous branches of the intercostal nerves thereby providing analgesia to the hemithorax [2,3].
We hypothesized that SAPB will provide effective postoperative analgesia and reduce postoperative morphine consumption in MRM surgeries. The primary objective of the study was to evaluate the duration of postoperative analgesia and the secondary objectives were to compare the postoperative consumption of morphine in 24 h, Visual Analog Scale (VAS) scores, and side effects of morphine like respiratory depression, pruritus, nausea and vomiting, and SAPB like hematoma, pneumothorax, and infection.
This prospective, randomized controlled study was done in a tertiary care teaching institution after obtaining institutional ethical committee clearance and Clinical trials registry India (CTRI/2019/01/017194) registration from 08.02.2019 to 30.01.2020. Sixty patients undergoing MRM surgeries under General Anesthesia (GA) were included in the study with 30 patients in both groups. Patients of age group between 18 and 65, weighing from 40 to 100 kg and belonging to the American Society of Anesthesiologists’ (ASA) physical status I-III were included in the study. Patients with stage 4 malignancies, cardiac, pulmonary, hepatic and renal dysfunction, coagulopathy, allergy to local anesthetics, chronic pain on opioid therapy, local infection, and not willing to participate were excluded from the study.
All the patients were assessed preoperatively. The study protocol was explained to the patients during the preoperative checkup and informed consent was obtained. The patients were educated about the use of Visual Analog Scale (0-10) for assessment of pain with a 0 score for no pain and 10 score for maximal pain. All the consented patients were randomized into two groups by computer-generated random numbers and group allotment by closed envelope method. The allocation was done by an independent person who opened the sealed envelope according to the computer-generated numbers before the start of the study. The first anesthesiologist managed anesthesia intraoperatively, administered the block for group A patients and did not take further part in the study. Group A patients received SAPB at the end of surgery before extubation and patients in group B did not receive any block. All the patients in PACU were monitored by the second anesthesiologist who was unaware of the patient groups.
General anesthesia was standardized for all the patients. Intravenous cannula size 18 G was placed in the non-operated hand and standard monitors like pulse oximeter, non-invasive blood pressure, electrocardiogram, and end-tidal carbon dioxide monitoring were instituted on all patients. Premedication was done with midazolam 0.02 mg/kg, ondansetron 4 mg intravenously. Morphine 150 µg/kg was administered 15 minutes before induction. Propofol 2 mg/kg was used for induction. Intubation was done with vecuronium 0.1 mg/kg and anesthesia was maintained with nitrous oxide-oxygen, sevoflurane 1 MAC, and intermittent boluses of vecuronium. All the patients received 1 g paracetamol intravenous infusion during skin closure and sixth hourly for 24 hours (h) postoperatively. End-tidal carbon dioxide was maintained at around 40 mmHg. SAPB was given to patients in Group A before extubation. No block was given for patients in Group B. All the blocks were done by a single experienced anesthesiologist and operated by a single surgeon.
SAPB was done with the patient in lateral position with the hand placed over the head. A high frequency (5-13 Hz) linear ultrasound probe (GE Logiq V2, GE Medical Systems, Jiangsu, China) machine was placed sagitally in the midclavicular region and traced towards the axillary region counting the ribs from 2nd to 5th. The probe was finally positioned over the fourth or fifth rib and the lattismus dorsi and serratus anterior muscles were identified. 20 ml of ropivacaine 0.25% with dexamethasone 8 mg was injected in a plane deep to serratus muscle and above the rib by an in-plane technique using 22 G 50 mm Stimuplex needle (Figure 1).

Figure 1: Ultrasound guided Serratus anterior plane block.
Reversal of neuromuscular blockade was done with Neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg at the end of surgery and extubated. The patients were monitored in the Post Anesthesia Care Unit (PACU). Morphine was administered for postoperative analgesia in Patient-Controlled Analgesia (PCA) pump at 0.1 mg/h baseline infusion and 1 mg bolus dose with a lockout interval of 10 min. The anesthesiologist monitoring the patient was blinded to the study group involved. Oxygen was administered by nasal cannula at four liters per minute to all the patients.
The duration of postoperative analgesia was defined as the time taken from extubation to the administration of the first bolus dose in the PCA pump. The amount of morphine consumed totally in the 24 h postoperative period was recorded and compared. VAS scores were recorded every two hours and compared between the groups. Any procedure-related complications like vascular puncture, infection, and pneumothorax were also noted. Side effects related to morphine infusion like respiratory depression, itching, nausea, and vomiting were noted and treated accordingly. Respiratory depression was defined as oxygen saturation of less than 94% or a respiratory rate of less than 10. Ondansetron was used to treat nausea, vomiting, and pruritus.
We hypothesized that SAPB prolongs the duration of postoperative analgesia following MRM surgeries. The sample size was calculated using the formula.
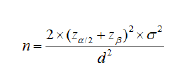
where Z α/2 is the critical value of the Normal distribution at α/2 (for a confidence level of 95%, α is 0.05 and the critical value is 1.96), Z β is the critical value of the Normal distribution at β (for a power of 80%, β is 0.2 and the critical value is 0.84), σ2 is the population variance which is calculated using the formula.
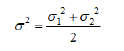
Using the data from our pilot study and taking d as eight hours (a clinically significant difference of pain-free interval between the groups), the sample size estimated was 16 in each group. For better statistical analysis, we recruited 30 patients in both groups. The cases in pilot study were not taken for inclusion in this study. The data were entered in MS-Excel Spreadsheet 2016 and analyzed using Statistical Package for the Social Sciences (SPSS) version 22.0. The quantitative variables are analyzed using Student's t-test and Chi-square test was used for analyzing qualitative variables. A p-value of less than 0.05 was considered statistically significant.
Sixty-six patients were recruited for the study. After excluding six patients who were not meeting inclusion criteria and unwillingness to participate, sixty patients were included. No cases were lost to follow up. The flow of patients was depicted in the CONSORT (Consolidated Standards of Reporting Trials) as in Figure 2.

Figure 2: Consolidated standards of reporting trials flow chart.
Patients in both groups were comparable in terms of demographic profile and duration of surgery (Table 1).
| Demographic profile | Group A (n=30) | Group B (n=30) | p-value |
|---|---|---|---|
| Gender (Male/ Female) | 0/30 | Jan-29 | 0.554* |
| Age (years) | 52.13 ± 10.68 | 53.9 ± 10.16 | 0.514* |
| Weight (kg) | 68.25 ± 6.32 | 67.59 ± 6.56 | 0.943* |
| ASA PS I/II/III | 0/21/9 | 0/22/8 | 0.959* |
| Duration of surgery (min) | 124.4 ± 17.63 | 125.87 ± 15.76 | 0.951* |
Note: *p- value not significant.
Table 1: Demographic data (Values in mean ± SD).
The data distribution was symmetrical and no skewing was observed. The duration of postoperative analgesia was prolonged in group A (1423 ± 185.55 min) compared to patients in group B (148 ± 51.11 min). The p-value was less than 0.0001 and hence highly significant. The total consumption of morphine was also reduced in group A (3.37 ± 0.85 mg) compared to group B (10.7 ± 1.6 mg), which was statistically extremely significant (p-value less than 0.01). The comparison of analgesic data was shown in Table 2.
| Analgesic data | Group A | Group B | p-value |
|---|---|---|---|
| Duration of postoperative analgesia (minutes) | 1423 ± 185.55 | 148 ± 51.11 | <0.0001Ϯ |
| Total morphine consumption (mg) | 3.37 ± 0.85 | 10.7 ± 1.6 | <0.0001Ϯ |
Note: Ϯ p-value significant
Table 2: Analgesia data (Values in mean ± SD).
The VAS scores were significantly lower in group A up to 20 h in the postoperative period (Figure 3).

Figure 3: Comparison of VAS scores between the two groups (mean values), (*P value- not significant; P value-significant).
The hemodynamic variables like heart rate, blood pressure and peripheral oxygen saturation were comparable in both groups with no statistical significance. There were no complications observed in both the groups related to block (block failure, vessel injury, and pneumothorax) as well as morphine administration (nausea, pruritus, respiratory depression).
SAPB, first described and it is in a newer regional anesthetic technique for chest wall surgeries as it effectively blocks the lateral branches of the intercostal nerves from T2 to T9 [2]. When performed under ultrasound guidance, the success of the block is improved and complications are avoided. The local anesthetic drug is deposited in the plane either superficial or deep to the serratus anterior muscle. The deep injection has the advantage of the good anterior distribution of the block with sensory blockade up to T2 dermatome despite a higher incidence of pneumothorax [4,5]. However, the incidence of pneumothorax is negligible in experienced hands in the presence of ultrasound. Hence, we adopted a deep injection technique to provide better blockade and the needle was advanced only after the visualization of the tip of the needle. A combined superficial and deep serratus plane block has also been performed to treat mastectomy pain [6,7]. The block can be performed either in the supine position or in a lateral position [2,7-9]. We found the lateral position to be more convenient and the block was given at the end of the surgical procedure and just before extubation as in few other studies 5 while pre-emptive block under general anesthesia was also done in some studies [7,8]. By the demonstrated modified SAPB also known as LD block for breast reconstruction surgeries where the drug was deposited between lattismus dorsi and serratus anterior in the posterior axillary line [10].
Ultrasound-guided SAPB was found to be effective in providing postoperative analgesia in breast surgeries in various studies [3,4,5,11,12]. Performed the block under direct vision deep to serratus muscle using levobupivacaine-clonidine mixture during mastectomy surgeries and found it to be effective for postoperative pain relief [13]. SAPB was also found effective in not only relieving acute pain following mastectomy but also treating chronic pain syndromes following breast surgeries [14]. SAPB was also used to provide analgesia in post-thoracotomy pain, rib fractures, implantable cardioverter-defibrillator implantation [15].
The time to request for the first analgesic dose was prolonged in the block group which was demonstrated in various other studies [3,8,16,17]. The duration of analgesia in our study was comparable to 20 ± 3 hours for SAPB as in the study 5 where 0.4 ml/kg of 0.25% Bupivacaine with 5 mcg/ml adrenaline was injected deep to the Serratus anterior muscle. The postoperative duration of analgesia was observed to be 323.5 ± 49.7 min in Rahimdazeh [3]. The study was significantly longer than the control group. But this was shorter compared to our study because they injected plain bupivacaine in the superficial plane. The duration of analgesia for SAPB was 245.6 ± 58 min in MRM surgeries. where plain bupivacaine 0.5% was injected superficial to serratus anterior muscle [7]. Dexamethasone was used as an adjuvant in our study and was also proven to increase the duration of analgesia in SAPB in various other studies [6,9,18]. The demonstrated dexamethasone was added to levobupivacaine provided 23-45 h of pain relief in patients with multiple rib fractures [18].
The amount of morphine consumption was significantly reduced in the SAP block group when compared to the control group. Significant reduction in fentanyl consumption was observed in mastectomy patients who received SAPB (104.2 ± 21.4 µg) than the control group (480.6 ± 25.6 µg) [3]. In two separate studies, SAPB was also found to have reduced the postoperative requirements of morphine (10.14 mg in SAPB group as against 5.48 mg in the control group) 9 and fentanyl (100 µg in SAPB group vs. 200 µg in the control group) 8 following thoracotomies [9].
VAS scores in the postoperative period were significantly lower in the SAPB group of Figure 3 which was analogous to many other studies [3,5,10]. Amin et al. demonstrated the VAS scores are lower both during rest and movement in mastectomy patients who received SAPB [5]. In a study on thoracotomy surgeries, SAPB was found to provide good hemodynamic stability than TEA with less VAS pain scores and reduced morphine consumption in the postoperative period [19]. Though TEA was considered as the gold standard for postoperative analgesia in thoracotomies, SAPB was found to be equally effective with better hemodynamic stability.
Some studies demonstrate the superiority of TPVB over SAPB while others favor SAPB as an effective technique for postoperative analgesia compared to TPVB [5,7,8,20].However, ultrasound-guided TPVB is technically skill-demanding with a steep learning curve and associated with complications. SAPB was technically easier to perform like Transversus Abdominis Plane block in abdominal surgeries with minimal complications [21]. We observed a prolonged duration of analgesia in the SAPB group compared to the PECS group in mastectomy patients though there was no significant difference in fentanyl consumption [10]. Hards demonstrated the superiority of SAPB over local wound infiltration in mastectomy surgeries [12]. There were no complications encountered in our study. Real-time ultrasound guidance helps in avoiding complications like vessel puncture, pneumothorax. Deposition of drug deep to the muscle usually spares long thoracic nerve and hence no case of winging of the scapula was reported in our study. The safety of the block was also demonstrated in various other studies [5,7,10,20].
There are a few limitations to our study. Double-blinding could not be done as the control group did not receive any block. An experienced anesthesiologist has performed all the blocks which may be another limitation, as we have not encountered failures or complications. Also, we did not measure serum concentrations of ropivacaine to predict absorption rate for local anesthetic toxicity. However, ropivacaine is a relatively safe drug and we have not exceeded toxic doses. To conclude, Serratus Anterior Plane Block is a highly effective regional anesthetic technique in providing prolonged postoperative analgesia and reducing the analgesic consumption with a high safety profile in experienced hands under ultrasound guidance.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Venkatraman R, Yogalakshmi K, Karthik K, Saravanan R (2022) A Prospective Randomized Controlled Study on Evaluation of Effectiveness of Serratus Anterior Plane Block for Postoperative Analgesia in Modified Radical Mastectomy Surgeries. J Anesth Clin Res. 13:1077.
Received: 25-Jul-2022, Manuscript No. JACR-22-19041 ; Editor assigned: 28-Jul-2022, Pre QC No. JACR-22-19041 (PQ); Reviewed: 12-Aug-2022, QC No. JACR-22-19041 ; Revised: 19-Aug-2022, Manuscript No. JACR-22-19041 (R); Published: 25-Aug-2022 , DOI: 10.35248/2155-6148.22.13.1077
Copyright: © 2022 Venkatraman R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.