Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2023)Volume 14, Issue 5
Fillers for volume replacement improve the appearance of depressions, grooves, and wrinkles. However, the frontal region presents a challenge due to intravascular injections and embolisms that can cause skin necrosis and blindness. Given the need for and benefits of filling, a safer technique to overcome these risks is necessary. The present study describes the protocol of a technique for filling the forehead involving the dissection of the soft tissue above the periosteum. This technique creates a space for filling placement, prevents the compromise of the vessels, and avoids the irregular appearance of the filling material. This protocol with dissection demonstrated that filling materials can be injected more safely and may be able to restore convexity and volume, improving aesthetic appearance and promoting support in the frontal region.
Skin; Face; Calcium hydroxyapatite; Hyaluronic acid
Volume loss in the face associated with age plays an important role in structural changes resulting from aging, so current treatments focus mainly on the restoration of lost volumes [1]. In addition, the aging of the forehead also manifests with loss of volume and convexity, with the appearance of depressions, sagging, and static wrinkles [2,3]. A convex, wrinkle-free forehead is considered aesthetically pleasing, and therefore volume replacement is a welcome strategy. However, injecting the frontal region has several limitations. The fat under the skin limits the space for implantation of the filling material and makes it difficult to camouflage any irregularity. However, the biggest concern even is the chance of intravascular injections and retrograde embolisms that can cause rare but devastating adverse effects such as blindness and stroke [2,4-7].
This article aims to provide specific guidelines for filling the forehead, describing a protocol that mainly includes tissue dissection as a safer alternative for volumazing, rejuvenation, and prevention of frontal aging.
Anatomical and physiopathological considerations
The primary source of blood supply to the orbit is the Ophthalmic Artery (OA), the first branch of the internal carotid artery. The central artery of the retina is a branch responsible for the retinal blood supply along with the posterior ciliary arteries, and the obstruction of these arteries has devastating consequences for vision [8,9].
The Supratrochlear Artery (STA) and Supraorbital Artery (SOA) are branches of the OA and provide the glabella and forehead with an abundant blood supply [10].
The fillings in the glabella are more likely to cause this rare complication, given the shorter distance to the central retinal artery or ciliary branches. Still, other middle and upper face regions are also at risk. Fillers in the forehead region can result in the SOA or STA accidental puncture. If the injection pressure exceeds systolic blood pressure, it can propel the plunger to travel closely, against blood flow, along the OA and its branches [5,7,11].
The SOA emerges from the supraorbital foramen (or notch) deeply and extends laterally to pierce the frontal muscle and become the superficial branch. Drilling occurs 20.7 ± 5.1 mm from the orbital margin [10]. Another study found a larger variation, from 20 to 40 mm above the orbital edge [12]. The supraorbital foramen can be identified on average at 10.8 ± 4.9 mm laterally, from the medial corner of the eye, along the orbital edge [10].
STA represents a terminal branch of OA and emerges medially at the orbital edge 1.2 mm above the inner corner of the eye. It pierces the corrugator muscle of the eyebrow, rises to the forehead between 1.7 and 2.2 cm from the midline, and becomes subcutaneous between 15 and 25 mm above the supraorbital edge [13-15]. The mean STA diameter is reported among the studies in a range of 0.6 to 1.4 mm [11,13,14,16]. A deep branch can rarely be present and it is located laterally to the superficial branch [10,11,15-17].
In the lateral region of the forehead, the STA and SOA can cause anastomosis with the frontal branch of the superficial temporal artery, a final branch of the external carotid artery [17].Therefore, the possibility of blindness is present in the filling of the temporal areas as well.
Description of the technique
The area selected for the filling should comprise the central part of the forehead where it usually presents greater depression and volume loss (Figure 1). The lower limit must respect two centimeters above the orbital bone border, because, from this limit, the SAO and STA are in the superficial plane (Figure 2).
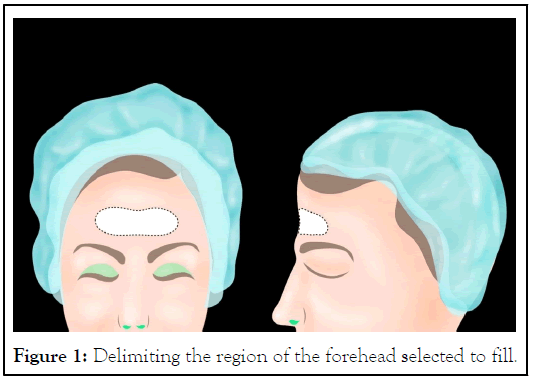
Figure 1: Delimiting the region of the forehead selected to fill.`
Figure 2: Anatomical representation of supratrochlear and supraorbital arteries.
Approximately 0.2 ml of 2% lidocaine with epinephrine is used for each anaesthetic button made on the sides of the delimited area, at approximately 45 mm from the midline so that the cannula reaches the entire area (Figure 3). The orifice can be done with a 21G needle, and a semiflexible and disposable cannula (21G × 50 mm) is used to deposit 1 ml of lidocaine with epinephrine at the periosteum level throughout. After anaesthetizing the area, the cannula is reintroduced deeply to dissect all the tissue above the periosteum, thus creating a space above the frontal bone to receive the filling material. Displacing all the tissue above the bone and making this place the filling material minimizes the possibility of puncture of arteries in this plane.
Figure 3: Representation of the filling area and its orifices.
Hyaluronic Acid (HA) has a direct filling effect at the site where it is applied, whereas Calcium Hydroxyapatite (CaHA) induces an inflammatory response leading to collagen synthesis [18-21].Therefore, the volume obtained by CaHA injection is primarily due to transporter gel volume, which is reabsorbed in the first 30 to 90 days. Later, the volume occurs through collagen formation. The high G' of the Rennova Diamond® and the posterior collagen formed allows substantial support to the overlapping tissues, with greater tissue integration, outstanding durability, and less displacement [1,22,23].The problem with creating volume only at the expense of CaHA on the forehead is that due to the small thickness of tissue and muscle activity, the possibility of nodule formation is greater. Recently, clinical studies with histological evaluation have shown that the association of CaHA with HA stimulates collagen production in the injected region, even in the presence of HA [20,24].
As a filler material, we selected a HA with relatively high viscoelasticity, Rennova Ultra Deep® (Panaxia LTD, Israel), with the purpose of volumization, but that was associated with CaHA (Panaxia LTD, Israel) for collagen stimulation. The synthesis of collagen formed within the HA matrix suggests greater tissue support and integration. For this reason, the association of CaHA with HA promotes volume with a lower chance of nodule formation. Additionally, this association has partial reversibility and collagen stimulation. The mixture consists of 1.25 mL of HA mixed with 1.25 mL of CaHA added 1 ml of saline solution to facilitate the accommodation of the material. Dilution reduces the viscosity of materials but preserves their elasticity and malleability [25,26].
The three materials are transferred and mixed using a Leur Lock connector system connecting to 2 sterile 3.0 mL polypropylene syringes.
Yag-Howard used the combination of HA-CaHA in more than 250 cases without adverse events (i.e., nodules, granulomas, or vascular occlusion).
The sample used in the present article includes more than 500 cases also treated with the association of CaHA and HA.
For a plunger to move retrogradely within an artery, the systolic pressure of the vessel must be overcome by injection force. Then, in addition to the safety steps already mentioned, the slow retrograde injection technique is recommended. The filler material, already mixed and homogenized, is transferred to a sterile polypropylene syringe of 1 ml to assist in this gentle injection pressure. The 21G × 50 mm gauge cannula is fixed to inject the material immediately after it is transferred.
Deep injections in this frontal region are essential, and touching the frontal bone with the cannula, with a scratching sound, signals that the application is in the correct plane. The filler is moulded to accommodate the space during injection, and irregularities or ripples are adjusted.
Before employing the technique, botulinum toxin is recommended so muscle activity does not displace the filling material.
To the detriment of high doses of botulinum toxin, the filling of the forehead helps to obtain a smoother forehead that is more sustained, with less eyebrow ptosis and less possibility of formation of static wrinkles because tissue thickness is increased (Figure 4).
Figure 4: (a) Before hydrolifting (b) After three months.
In the post procedure recommendations, the patient is instructed to not to compress the area using bands or caps for approximately three weeks. Eyelid oedema may occur between 3 and 5 days after the procedure. Administration of 4 mg of dexamethasone 1 hour before the procedure is performed to minimize the risk of inflammation and edema.
The filling of the forehead, despite the good aesthetic response, is not frequently indicated in clinical practice because the concern with blindness discourages professionals from performing it.
In the most significant systematic review of secondary blindness after facial filling injections with 190 patients, injection velocity and pressure influenced the development of blindness. These two reasons directly influence the possibility of intravascular embolization, with a displacement of the material in the arterial counterflow [27].The injection force must overcome systolic blood pressure to push the filler droplets closely along the OA. For this reason, it reaffirms the clinical recommendation that excessive syringe pressure and rapid speed should be avoided during filling [5,6]. So, the retrograde and slow injection technique is recommended.
Thus, the preference for larger calibre cannulas reduces the possibility of embolisms, and smaller syringes reduce the injection speed [4,6].
The viscosity of the material is also crucial because it determines the injection speed and pressure used by the injector. Therefore, the dilution of the material increases the safety of the technique.
The diameter of the STA varies between 0.6 mm and 1.4 mm, and the 21G cannula is 0.8 mm. The smaller the cannula's lumen concerning the vessel's lumen, the greater the possibility of embolization. So, a 21G or larger cannula is the ideal option.
Considering the superficial location of the vessels on the forehead, with the possibility of embolization and blindness, any technique in this region must be in a deep plane.
Although the anatomical possibility of a larger calibre vessel in a deep plane in this selected area is scarce, the dissection predicted, with the creation of a supraperiosteal cavity before the application of the filling material, makes the technique safer.
Two studies proposed the injection of tumescent solution with deep serum and anaesthetic before the filler application was proposed in two studies. The intention was to promote a tissue hydrodissection and create a space bag to distribute CaHA and avoid possible vascular impairments [3,27].However, serum injection leads to a more significant postoperative transient oedema, especially in the eye region, which generates patient concern and dissatisfaction. The dissection, with mechanical creation of the cavity and minimal serum, can provide the space needed to deposit the material.
It is possible to establish a step covering several aspects capable of increasing the safety of the filling of the forehead and encouraging professionals to perform it. Dissection of tissues above the periosteum is one of these indispensable steps before depositing the filler, minimizing the possibility of embolisms and obtaining satisfactory aesthetic results in the volumization and rejuvenation of the forehead.
The one ml syringe allows low strength for extrusion of the material, deposited slowly and in retroinjection avoids intravascular embolization. Additionally, the 21G-caliber cannula minimizes the possibility of embolization as well, and along with the dilution of the material, it also allows a small force for extrusion.
Citation: Scardua T, Scardua N, Carpinteiro I (2023) A Dissection Technique for Filling the Forehead. J Clin Exp Dermatol Res. 14:648.
Received: 14-Aug-2023, Manuscript No. JCEDR-23-26064; Editor assigned: 16-Aug-2023, Pre QC No. JCEDR-23-26064(PQ); Reviewed: 31-Aug-2023, QC No. JCEDR-23-26064; Revised: 08-Sep-2023, Manuscript No. JCEDR-23-26064(R); Published: 15-Sep-2023 , DOI: 10.35841/2155-9554.23.14.648
Copyright: © 2023 Scardua T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.