
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Case Report - (2025)Volume 16, Issue 1
Tetralogy of fallot is one of the most common forms of cyanotic congenital heart disease and in the absence of surgical correction it has an elevated early mortality, with most patients dying in childhood. The authors reported this case because of the unusual course of an uncorrected tetralogy of fallot. There are only a few reports of patients with an uncorrected tetralogy of Fallot who reach an advanced age and to the best of our knowledge this is the first case report of a possible endocarditis in a patient with an uncorrected tetralogy of fallot who is older than 70 years.
Cyanotic congenital heart disese; Surgical; Fallot
Pregnancy adversely affects physiology in patients with Congenital Heart Disease (CHDs), the impact is greater in cyanotic coronary heart disease. Patients with uncorrected Fallot Tetralogy (TOF) rarely survive until pregnancy. Usually, the extent of cyanosis is correlated with the severity of TOF; a subgroup of patients with TOF are acyanotic, popularly called 'pink TOF'. Patients with pink TOF generally have less severe Pulmonary Stenosis (PS). However, if PS is severe in such patients, the possibility of Major Aorta Pulmonary Collateral Arteries (MAPCAs) should be ruled out. Here, we report the anesthesia treatment of a 27-year-old pregnant woman with pink TOF with severe PS, who presented for an emergency Lower Segment Caesarean Section (LSCS) in the 36th week of gestation [1].
A 27-year-old woman from G3P1A2 diagnosed with TOF complained of increased exertional dyspnea and acral cyanosis. Breathlessness started to worsen progressively beyond the 32nd week of gestation; cyanosis became noticeable even on the lips and tongue. Two-dimensional echocardiography at 32 weeks showed TOF with severe PS, a pulmonary gradient of 65, mmHg and biventricular enlargement (Left Ventricular diastolic diameter (LV), 5.4 cm; LV systolic diameter 3.8 cm; ejection fraction, 55%; and bidirectional shunt).
At the 35th week, she was admitted for breathlessness (grade 4); repeat 2D echo showed mild to moderate LV dysfunction (LV diastolic diameter, 6.0 cm; LV systolic diameter, 4.6 cm; ejection fraction, 45%) (Figure 1).
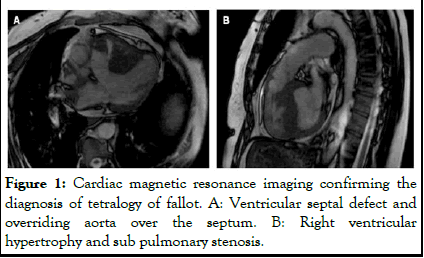
Figure 1: Cardiac magnetic resonance imaging confirming the diagnosis of tetralogy of fallot. A: Ventricular septal defect and overriding aorta over the septum. B: Right ventricular hypertrophy and sub pulmonary stenosis.
On the 35th week and the 4th day an emergency LSCS was planned for a non-reassuring fetal heart rate and oligohydramnios. Arterial blood gas before surgery showed the following results: pH, 7.47; PO2, 57 mmHg; PCO2, 24 mmHg; K+, 2.7 meq/l; haemoglobin, 15 g/dL; and lactate, 3.2 mmol/L. The baseline saturation in the room air was 85%, which improved to 98% with supplemental oxygen through a venturi mask with a flow of 10 L/ min. The respiratory rate was 28 breaths/min and the noninvasive blood pressure was 138/96 mmHg. Chest auscultation revealed bilateral fine basal crepitations [2]. After explaining the risks and benefits of General Anesthesia (GA) and Central Neuraxial Block (CNB), informed consent was obtained. Five-lead electrocardiograms were attached, 18-G intravenous (IV) cannula was secured and left radial artery cannulation was performed. Before Subarachnoid Block (SAB), arterial blood pressure, pulse rate (HR) and respiratory rate were 130/80 mmHg, 98 beats/min (regular) and 30 breaths/min. Low-dose SAB was preferred over Epidural Anesthesia (EA) due to ongoing fetal distress and meconium-stained amniotic fluid. Ceftriaxone (2 g IV) and gentamicin (120 mg IV) were administered as infective endocarditis prophylaxis. Four milligrams of IV ondansetron were administered for antiemesis and potassium correction was also initiated.
The patient was placed in the right lateral position before spinal injection and wedged in the supine position afterward. Subarachnoid injection was administered in the L3-L4 interspaces using a 25-G quincke needle, 1.5 ml of 0.5% bupivacaine heavy with 25 mcg of fentanyl was administered and a sensory block level of T6 was achieved [3].
After SAB, blood pressure dropped to 100/60 mmHg and recovered after two IV boluses of phenylephrine (50 mcg each) and 200 ml of saline bolus. During surgery, a total of 500 ml of saline was infused. The newborn weighed 1.2 kg and the apgar score was 8. After removal of the placenta, methylergonovine (0.2 mg) was administered intramuscularly, followed by an infusion containing 10 U of oxytocin in 500 ml of normal saline (20 drops/min). Transverse abdominis plane block was used for postoperative pain relief, along with 1 g of paracetamol IV every 6 h. The patient was moved to the postoperative Intensive Care Unit (ICU) and the newborn was transferred to the Neonatal Intensive Care Unit (NICU). Before moving the patient to the ICU, 40 mg of furosemide was administered intravenously; additional oxygen (10 L/min, venturi mask) was administered throughout. The next day, the patient was transferred to the high-dependence obstetric unit and the ward a day later. The newborn remained in the NICU for 2 weeks due to low birth weight; later, both the mother and the newborn were discharged from the hospital [4].
The main physiological problem for a pregnant woman with uncorrected TOF is cardiac decompensation; pregnancy-induced volume overload and fluid changes during labor tend to precipitate left ventricular LV failure. Pregnancy-associated hypercoagulability and immunosuppression predispose the pregnant to the risk of thromboembolism and infections. Even in a pregnant woman with a corrected TOF, cardiovascular changes of pregnancy can reveal residual or recurrent TOF [5].
Only a few adults, with uncorrected TOF, have survived until the third decade have been reported. Although most patients with uncorrected TOF patients are blue; cyanotic, a few are pink acyanotic as well. MAPCAs should always be anticipated in a 'pink TOF'. It is critical to differentiate between blue and pink TOFs because they significantly change management goals.
MAPCAs develop early in embryonic life but usually regress as normal Pulmonary Arteries (PAPAs) develop. In the presence of severe pulmonary stenosis PS (or pulmonary atresia), MAPCAs may continue to grow and become the main source of blood flow to the pulmonary arteries. Since MAPCA arises from the systemic circulation, they expose PA to systemic pressures, resulting in the progressive development of Pulmonary Artery Hypertension (PAH). In the presence of Patent Ductus Arteriosus (PDA) with Pulmonary Stenosis (PS), although saturation is above 80%, the lung parenchyma is not affected much. In contrast, with MAPCA, some patients may have torrential blood flow to the AP that disturbs the lung parenchyma and the patient often has hemooptysis. Patients with a decrease in blood flow to the PA through MAPCA will have progressive increasing cyanosis and patients with torrential blood flow will have high volume overload and progressive left heart failure. These patients may have received prior treatment with diuretic or Angiotensin Converting Enzyme inhibitors (ACE) treatment.
Almost all available literature deals with anesthesia concerns in the 'blue TOF' “blue TOF”; it is critical to differentiate between a pink and a blue TOF from the pathophysiological point of view. In blue TOF, poor lung circulation leads to hypoxemia, polycythaemia and cyanosis. In MAPCA-pink TOF, in the early stage of MAPCA-pink TOF, hypoxemia is less severe and so is polycythaemia; however, in the later stage, LVF and PAH are the main concerns. Preservation of inotropy and Systemic Vascular Resistance (SVR) and prevention of further worsening of PAH are common goals for both types of TOF. Unlike cyanotic TOF, where IV fluid loadings are done performed before induction of anesthesia (to prevent infundibular spasm and improve blood theology), fluids should be restricted in 'pink’ TOF [6].
Although GA is preferred in 'blue TOF,' few reports of CNB are also described there. In our case, CNB helped eliminate the need for mechanical ventilation (weaning from mechanical ventilation could have been difficult due to the anticipated high PAH). Epidural Anesthesia (EA) was the modality of choice was EA, but we preferred SAB due to the time constraint due to coexisting fetal distress.
When managing a "pink TOF", invasive hemodynamic monitoring should be adopted pre-emptively and an emergency cart for intubation should be kept handy. Endocarditis prophylaxis must be given administered. A lower dose of local anesthesia than usual should be used in SAB; any block level inadequacy can be managed with intravenous IV ketamine supplementation. Any drop in oxygen saturation may not necessarily be due to an increase in the right-to-left shunt (a worsening of LV function should always be ruled out). Phenylephrine should be preferred to mephenteramine to restore SVR; any rhythm abnormality or electrolyte imbalance must be promptly corrected [7].
Methylergonovine should be preferred to oxytocin for uterine contraction, because oxytocin may cause a fall in SVR. Methylergonovine may worsen LVF and should be addressed. Postoperative pain should be adequately managed (poorly managed pain can worsen PAH), preferably with regional anesthesia techniques. Uncorrected TOF is associated with an increased maternal and fetal adverse outcome, including mortality. However, close coordination between the obstetrician, an anesthesiologist, between a cardiologist and a neonatologist is vital to a good outcome [8].
The case report refers to an adult "pink TOF" patient; these patients are encountered very rarely. Pregnancy-associated pathophysiological changes tend to complicate pathophysiology adversely and unpredictably. Although some case reports on 'blue TOF' treatment with pregnancy are available, none of them deals with anesthetic implications in 'pink TOF.' Since the pathophysiology of pink TOF is quite diverse from that of blue TOF, this case report might be a valuable addition to the literature.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Kumar S (2025) A Deceptive Case of Uncorrected Pink Tetralogy of Fallot with Severe Pulmonary Stenosis for Emergency Caesarean Section: A Report. J Anesth Clin Res. 16:1173.
Received: 11-Feb-2024, Manuscript No. JACR-24-29556; Editor assigned: 15-Feb-2024, Pre QC No. JACR-24-29556 (PQ); Reviewed: 29-Feb-2024, QC No. JACR-24-29556; Revised: 01-Jan-2025, Manuscript No. JACR-24-29556 (R); Published: 08-Jan-2025 , DOI: 10.35248/2155-6148.25.16.1173
Copyright: © 2025 Kumar S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.