International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2021)Volume 9, Issue 4
In this review, we organize confusing concepts of frailty, locomotive syndrome, Musculoskeletal Ambulation Disability Symptom (MADS) Complex, and sarcopenia, as avoiding fall into “word play.” The concept of Clinical Dementia Rating may be useful for understanding mixed situations. Clinical conditions differ during the process of lesion development in the brain among patients with Alzheimer disease, and that the idea of biaxial thinking for “disease” and “condition” is required. Regarding frailty, a mix of “disease” and “condition” in criteria may be a cause of confusion, and this may be an important idea in daily clinical practice. Since frailty has been identified as a reason for fall in many academic studies, of which 70% used Fried’s criteria, it is clear that frailty reflects decreased motor function. This suggests a relationship between frailty and fall.
Frailty; Locomotive syndrome; Musculoskeletal Ambulation Disability Symptom (MADS) Complex; Sarcopenia.
“Frailty” is a general term
There are many words related to frailty and the relationship among these words is complex. Therefore, we first classified these words. The International Statistical Classification of Diseases and Related Health Problems (ICD-10, 2021) defines frailty as age-related physical debility (Diagnosis Code R54). The original meaning of “frailty” is the condition of being weak and delicate, weakness in character or morals [1]. “Frail elderly people” are judged as independent by the certification of long-term care need based on the Long-Term Care Insurance Act but require support for some activities of daily living (ADL) due to decreased mental/physical functions and diseases, although they do not need nursing care or support. Academically, frailty is theoretically defined as a clinically recognizable state of increased vulnerability resulting from aging-associated decline in reserve and function across multiple physiologic systems such that the ability to cope with everyday or acute stressors is comprised [2]. In the absence of a gold standard, according to Xue , frailty has been operationally defined by Fried et al. [3]. In Japan, frailty is defined as a “conditions with increased vulnerability for various adverse health outcomes, in addition to various dysfunctions (decreased standby capacity) accompanied with aging [4].”
The Japan Geriatrics Society suggests that weakness can be expressed as frailty. Arai et al. suggested that frailty can be translated into Japanese as “fureiru” and is classified as “senility” (R54) in ICD-10, as age-related physical debility [4]. Frailty has been translated into Japanese words that show “weakness,” as well as “senility,” “debility” and “vulnerability.” However, “weakness” may suggest a “situation with irreversibly deteriorated conditions due to aging,” whereas “frailty” indicates that health may be regained by appropriate intervention. Based on this, the Japan Geriatrics Society changed the translated Japanese word from “weakness” to “frailty” in 2014 [4,5]. Therefore, frailty is defined as a condition caused by deterioration due to aging that may revert to a healthy condition with an intervention. Frailty also has physical, mental/psychological, and social aspects.
Locomotive syndrome
Advocated by the Japanese Orthopaedic Association is defined as a “condition with a high risk of nursing care needed due to locomotor disability [6]” and a “situation with decreased locomotive function due to locomotor disability [6].” The causes of “locomotor disability” in persons with locomotive syndrome are divided into “diseases of locomotor apparatus” (musculoskeletal motor system) and “locomotor dysfunction due to aging.” The former is a “decrease of balance ability, physical strength, and mobility capability due to locomotor diseases caused by aging, such as humpback, ease of fracture, spondylosis deformans, and spinal canal stenosis, in patients with osteoarthritis and osteoporosis, or symptoms of rheumatoid arthritis (pain, limited range of motion, muscle weakness, paralysis, bone fracture, spasticity).” The latter is conditions such as “muscle weakness, diminished stamina, increased reaction time, decreased motion velocity, decreased motor skills, decreased deep sensibility, and decreased balance ability”.
Musculoskeletal Ambulation Disability Symptom (MADS) Complex
A part of locomotive syndrome is defined as a “condition with decreased balance ability and mobility/walking capability caused by aging, with a high risk of fall and being housebound [6].”
The diagnostic criteria are:
• any of 11 locomotory diseases/conditions causing motor deterioration due to aging,
• a condition equivalent to rank J or A in the criteria for measuring degree of independence in daily life,
• and motor function: single-leg standing with open eyes for <15 s or a 3 m Timed Up-and-Go (TUG) test of ≥ 11 s.
Sarcopenia
Is a similar concept to frailty and is expressed as “M6284 (M62.84) Diagnosis Sarcopenia” in ICD-10 [7] and registered as a different item from frailty. In the practical definition by the European Working Group on Sarcopenia in Older People (EWGSOP) [8], sarcopenia is a “syndrome with a risk of harmful outcomes, such as physical disability, decrease of QOL, and death, and characterized by progressive and systemic decrease of skeletal muscle mass and strength.”
The EWGSOP diagnostic criteria for sarcopenia include:
• decrease of muscle mass and other events
• decrease of muscle strength or
• decrease of physical ability
In addition, there are various measurement methods proposed by the EWGSOP alone [8]. In Japan, sarcopenia is defined based on a decrease of skeletal muscle mass and strength or a decrease of physical function (gait velocity, etc.) due to aging [9], and the criteria are compliant with the EWGSOP diagnostic criteria. Specifically, a decrease of muscle mass (corrected to limb muscle mass) is measured by Bioelectrical Impedance Analysis (BIA) (male: <7.0 kg/m2, female: <5.7 kg/m2) or Dual Energy X-Ray Absorptiometry (DXA) (male: <7.0 kg/m2, female: <5.4 kg/ m2). Muscle strength is measured by grip strength (male: <26 kg, female: <18 kg), while physical ability is measured by gait velocity (<0.8 m/s) [9]. Sarcopenia is classified into primary (age-related) and secondary (related to activity, disease, or nutrition) types.
Our classification of the words and concepts related to frailty indicated that the definition of locomotive syndrome was unclear, but that diagnostic criteria for sarcopenia and MADS Complex were clear. Furthermore, severity can only be estimated for sarcopenia, for which muscle mass is objectively measured.
Fried’s diagnostic criteria for frailty are also clear, but these criteria focus mainly on the body and may not cover the entire concept of frailty. Thus the absence of a uniform definition of frailty might be a cause of confusion.
Diagnostic criteria for frailty include the accumulated deficit model [10], Phenotype model [3], Clinical Frailty Scale (CFS) [11], FiND Questionnaire [12], Gérontopôle Frailty Screening Tool [13], FRAIL scale [14], basic checklist [15], Frailty Screening Index [16], Edmonton Frail Scale [17], and Study of Osteoporotic Fractures (SOF) Index [18]. The Japanese version of the Fried’s criteria [19], simplified frailty questionnaire screening [20], simplified frailty index [21], basic checklist [15], and nursing care prevention checklist are used in Japan [22]. Cognitive frailty is defined as a condition of physical frailty with cognitive disorder (e.g. Clinical Dementia Rating [CDR] of 0.5) (excluding dementia) by the working groups of the International Academy on Nutrition and of Gerontology Aging (IANA) and the International Association and Geriatrics (IAGG) [23]. Thus, there are many diagnostic criteria used in studies of frailty.
Satake et al. suggested that frailty can be divided into an accumulated deficit model, which reflects accumulation of diseases, daily activity impairment, and physical activity impairment causing adverse events due to aging; and a phenotype model, which includes accumulation of symptoms caused by functional deficiency of various physiological systems with aging [24].
The former is the accumulated deficit model of Rockwood et al. which suggests that frailty reflects accumulation of various factors (disease, ADL impairment, physical impairment, and cognitive dysfunction). The Frailty Index is composed of 70 items that widely cover diseases, neurological signs, physical activity, ADL/ IADL, motor function, cognitive function, and mental status [10]. The latter is the phenotype model proposed by Fried et al. [3].
Frailty based on the Fried’s criteria
The phenotype model proposed by Fried et al. [3], in which frailty is defined as the presence of ≥ 3 of s hrinking (weight loss), weakness (decreased muscle strength), exhaustion (easily fatigued), slowness (decreased gait velocity), and low activity (decreased physical activity), and pre-frailty as the presence of 1 or 2 of these items. This model focuses on physical aspects of frailty. Almost 70% of academic studies of frailty are based on Fried’s criteria [24], probably because these criteria are relatively simple to evaluate. However, it has been suggested that frailty can be understood differently, even in the same subjects, when different diagnostic criteria are used [25,26]. Thus, a clear definition and uniform criteria are required to deepen understanding of frailty.
Clinical conditions associated with frailty, locomotive syndrome, Musculoskeletal Ambulation Disability Symptom (MADS) Complex, and sarcopenia are shown in Figure 1 and Table 1.
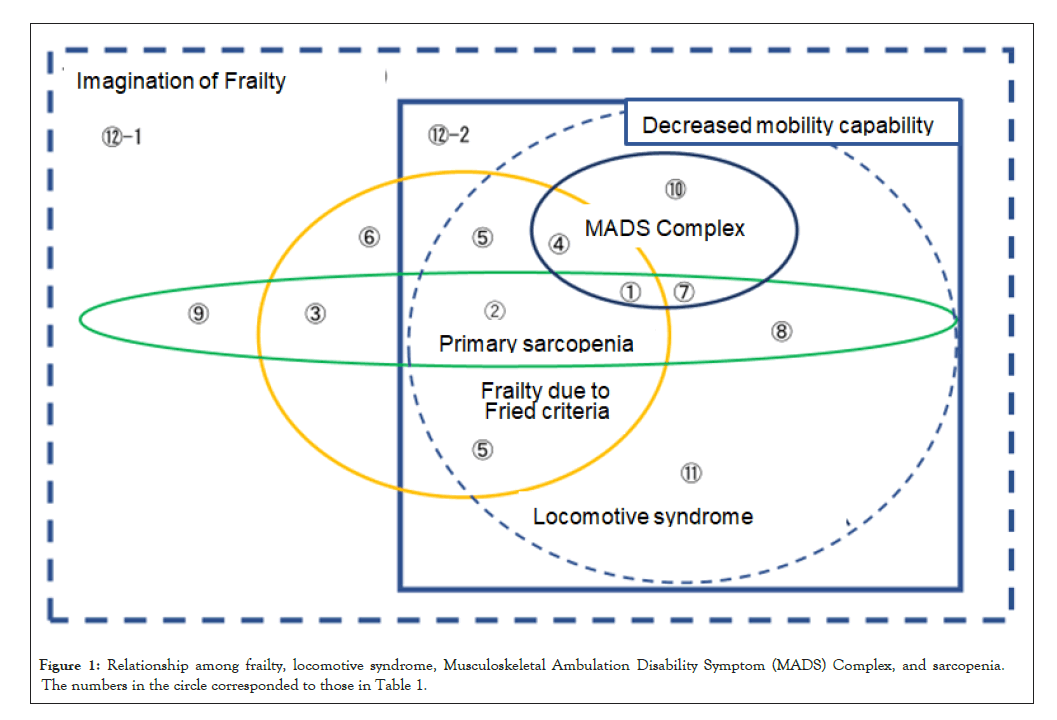
Figure 1: Relationship among frailty, locomotive syndrome, Musculoskeletal Ambulation Disability Symptom (MADS) Complex, and sarcopenia. The numbers in the circle corresponded to those in Table 1.
| Frailty due to Fried criteria | Primary sarcopenia | Locomotive syndrome | Musculoskeletal Ambulation Disability Symptom Complex | Clinical conditions | |
|---|---|---|---|---|---|
| ① | Yes | Yes | Yes | Yes | Seemingly independent walking, but decreased skeletal muscle mass, balance and mobility capability |
| ② | Yes | Yes | Yes | No | decreased mobility capability due to decreased skeletal muscle mass and also due to locomotory diseases |
| ③ | Yes | Yes | No | No | Preserved mobility capability despite locomotory diseases. but decreased skeletal muscle mass causing generalized fatigue and body weight loss |
| ④ | Yes | No | Yes | Yes | Seemingly independent walking and preserved skeletal muscle mass, but decreased balance and decreased mobility capability due to locomotory diseases |
| ⑤ | Yes | No | Yes | No | Preserved skeletal muscle mass, but decreased mobility capability due to locomotory diseases |
| ⑥ | Yes | No | No | No | Preserved skeletal muscle mass and mobility capability despite locomotory diseases, but generalized fatigue and body weight loss |
| ⑦ | No | Yes | Yes | Yes | Seemingly independent walking, but decreased balance and decreased skeletal muscle mass, and also decreased mobility capability |
| ⑧ | No | Yes | Yes | No | Decreased skeletal muscle mass and decreased mobility capability due to locomotory diseases |
| ⑨ | No | Yes | No | No | Preserved mobility capability but decreased skeletal muscle mass |
| ⑩ | No | No | Yes | Yes | Seemingly independent walking, but decreased balance and decreased mobility capability due to locomotory diseases |
| ⑪ | No | No | Yes | No | Decreased mobility capability due to locomotory diseases. Preserved skeletal muscle mass, and seemingly independent walking and no decreased balance, or seemingly dependent walking |
| ⑫-1 | No | No | No | No | Preserved mobility capability and skeletal muscle mass, but sometimes cognitive impairment and social isolation |
| ⑬-2 | No | No | No | No | Decreased mobility capability despite no locomotive syndrome, but due to dementia |
Table 1: Clinical conditions associated with frailty, locomotive syndrome, Musculoskeletal Ambulation Disability Symptom (MADS) Complex, and sarcopenia. The numbers in the leftmost column corresponded to those in Figure 1.
The concept of CDR [27,28] may be useful for understanding mixed situations. Clinical conditions differ during the of process lesion development in the brain among patients with Alzheimer disease, and that the idea of biaxial thinking for “disease” and “condition” is required.
Regarding frailty, a mix of “disease” and “condition” in criteria may be a cause of confusion, and this may be an important idea in daily clinical practice. Since frailty has been identified as a reason for fall in many academic studies, of which 70% used Fried’s criteria it is clear that frailty reflects decreased motor function. This suggests a relationship between frailty and fall.
No financial disclosure.
No conflict of interest.
Citation: Kumai K, Meguro K (2021) A Confusing General Term “Frailty” Should be Organized in Relation with Fried’s Criteria for Frailty, Locomotive Syndrome, Musculoskeletal Ambulation Disability Symptom Complex, and Sarcopenia, as Avoiding Fall into “Word Play”. Int J Phys Med Rehabil. 9:601.
Received: 11-Mar-2021 Accepted: 25-Mar-2021 Published: 01-Apr-2021 , DOI: 10.35248/2329-9096.21.9.601
Copyright: © 2021 Kumai K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.