
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2018) Volume 9, Issue 9
Keywords: Postoperative analgesia; Local anesthesia infiltration; TAP-block; Lower abdominal surgery; Ethiopia
C/S: Caesarian Section; CI: Confidence Interval; LAI: Local Anesthesia Wound Site Infiltration; NPS: Numeral Pain Score; SA: Spinal Anesthesia; SPSS: Statistical Package for Social Science; TAP: Transversus Abdominis plane; TVP: Trans Vesicle Prostatectomy; VAS: Visual Analogue Score; VNRS: Verbal Numeric Rating Scale
Pain is an unpleasant sensory or emotional experience associated with actual or potential tissue damage [1]. Post-operative acute pain management is a major health issue, hence acute post-operative pain management is critical to patient satisfaction and a timely discharge, for improved outcomes and to reduce health care costs [2]. Currently, the main stay of treatment for acute post-operative pain is the use of systemic opioids [3]. Unfortunately, opioids are not without complications. Drowsiness, nausea, vomiting, ileus, urinary retention and pruritus, are all side effects of opioids [4].
Knowledge of pain pathways and mechanisms has supported the development of a variety of drugs that alleviate pain through different pharmacological action [5]. Transversus Abdominis Plane (TAP) block technique has been shown to be safe and effective postoperative adjunct analgesia methods in variety of general [6,7] gynecological [8-10], urological [11], plastic [12,13] as well as pediatric surgery [14,15] and it’s suggested as part of the multimodal anesthetic approach to enhance recovery after lower abdominal surgery. Transversus Abdominis Plane (TAP) block provided by technique of using a ‘two pop’ sound at ‘triangle of Petit’, is generally advocated and supported by the cadaveric and imaging studies published to date [16]. A single injection can achieve sensory block over a wide area of the abdominal wall and provides analgesia to skin and muscle of the anterior abdominal wall [17].
Another approach to control post-operative pain and limit postoperative opioid usage is Local Anesthetic wound site Infiltration (LAI) prior to wound closure. These approaches lessen peripheral and central hyperalgesia and minimize wound inflammation producing less post-operative pain without impairing wound healing [18]. Local anesthesia wound infiltration is technique of obtaining postoperative pain relief by single injection of local anesthesia into skin and subcutaneous tissue layer at surgical incision sites, which decrease post-operative pain. Wound infiltration technique commonly used alone or in combination to improve postoperative analgesia, reduce opioid and speed patient recovery [19].
TAP-block reduces analgesia requirements, consequently reduces opioid-mediated side effects and it provides highly effective postoperative analgesia in the first 24-48 h post-operatively [20]. The administration of a local anesthetic via infiltration of the surgical wound is one component of a multimodal approach that results in immediate pain relief, which has been proven to increase patient satisfaction [21-23].
There are many studies done in different countries which compare the efficacy of LAI with TAP-block as part of multimodal analgesia but there are conflicting results. Hence, the primary outcome of this study is to compare the time to first analgesia request time between bilateral Transversus Abdominis Plane (TAP) block and wound site Local Anesthesia Infiltration (LAI) for post-operative pain relief for lower abdominal procedure under general anesthesia. The secondary outcomes are to compare the analgesia effectiveness of the two groups and to compare total 24 h analgesia consumption between TAP and LAI groups.
Ethical clearance was obtained from Addis Ababa University ethical clearance committee before the start of the study. This study was conducted in Empress Zewditu Memorial Hospitals, one of the public hospitals in Addis Ababa, capital of Ethiopia.
Study design
Institution based comparative observational cohort study was conducted from Jan 1, 2018 to March 30, 2018.
Source population
All surgical patients who are admitted for lower abdominal procedures at Empress Zewditu Hospital during study period.
Study population
Patient who underwent lowers abdominal surgery under general anesthesia at Empress Zewditu Hospital during study period and fulfills the inclusion criteria.
Inclusion criteria
ASA I and II patient and Age (18-65) years.
Exclusion criteria
Allergy to local anesthetic drug, Patients receiving cardio vascular drugs, BMI>30 Kg/M2, Medical disorders other than the surgical case.
Sample size and sampling technique
Time to first analgesia request was one of outcome indicators and we take previous observational study [24,25] which reported Time to first analgesia request (hour) in TAP-block 6.11 ± 6.2 and LAI group 2.63 ± 1.83. By assuming 1:1 ratio, the sample size was determined by the formula as,
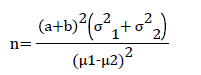
Where, 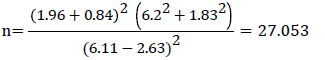
Where, n=the sample size in each of the groups
a=conventional multiplier for alpha=0.05, which is 1.96
b=conventional multiplier for power=0.80, which is 0.842
σ1-Standard deviation for time to first analgesia request
σ2-Standard deviation for time to first analgesia request
μ1-Mean for first analgesia request
μ2-Mean for first analgesia request
Ten percent of additional sample was included by assuming loss to follow up and a total of 30 samples for each group were calculated.
During the study period 198 patients were estimated to undergo lower abdominal procedure under general anesthesia in the hospital. With systematic random sampling every 3rd patients who were scheduled for lower abdominal procedure, fulfill inclusion criteria and volunteer were recruited to take part in the study. Since randomized control trial (RCT) was not yet allowed in our university, the patients were not randomized for anesthetic management. Rather by starting at random, every selected participant was placed to either group based on the responsible anesthetist’s post-operative pain management plan (whether they received local anesthesia infiltration or TAP-block). Anesthetic management including perioperative and pain management was at the discretion of the personnel anesthetist assigned to each case. We the investigators did not involve in the perioperative management of patients. Those patients who received bilateral TAP-block with 20 ml of 0.25% bupivacaine by technique of using a ‘two pop’ sound (blind technique) after the end of procedure were considered as TAP-block. The LAI group was defined, in this study, as those patients who receive wound site local anesthesia infiltration by the surgical residents after the end of procedure with 20 ml of 0.25% bupivacaine. This continues until the desired sample in each groups were achieved. Patients were given training and instructed on how to self-report pain using the eleven Point Numeric Rating Scale (NRS) score 0 to 10 in the morning of operation day at the ward with trained nurse. Participant’s involvement in the study was on voluntary bases, participants who were not willing to participate in the study and those who wish to quit their participation at any stage was informed to do so without any restriction.
In the postoperative period patients were transferred to recovery room and then to surgical ward. In the recovery and ward patients were observed by two blinded data collectors (nurses) and pain is managed by intravenous tramadol based on the request or complains of pain by the patient.
At post-op recovery room, patients were asked to report their pain based on 11 point NRS score as soon as patient fully respond to verbal command. Verbal numeric rate scale (VNRS) score and other variables were documented at 30 min, 1st h, 2nd h, 4th h, 6th h, 12th h and 24th h at recovery and surgical wards after the end of surgery. A time in minutes from end of surgery to first analgesia request were documented together with total analgesia (opioid) consumption in the first 24 h. Data were checked for completeness, accuracy and clarity by the investigators.
Data processing and analysis
Data was coded, edited and then entered and cleaned using Epi Info version 7 and exported and analyzed using Statistical package for Social Sciences (SPSS) software version 20.0. Shapiro Wilk test were used to test for distributions of data while homogeneity of variance were assessed using Levene’s test for equality of variance. Numeric data were described in terms of mean ± SD for symmetric and median (Interquartile range) for asymmetric data respectively. Comparisons of numerical variables between study groups were done using unpaired student t-test (independent t-test) for symmetric data and Manny Whitney U test were used for asymmetric data. Frequency and percentage were used to describe categorical variable and statistical difference between groups were tested using Chi square or Fisher’s exact test, as appropriate. Significance was determined at P value <0.05.
Operational definition
The following definitions were used for this study
Local anesthesia wound site infiltration: Using local anesthetic wound infiltration prior to wound closure for the purpose of postoperative pain management.
Lower abdominal procedures: Surgical procedures done on abdomen which is below umbilicus.
Numeric rating scale: Is a valid pain intensity assessment tool that involves asking a patient to rate his or her pain from 0-10 (11 point scale) with the understanding that 0 equal to no pain and 10 equal to the worst possible pain [26,27].
Pop sound: Sound feels during the needle pierce external and internal oblique muscle.
Time to first analgesia request: A time in minutes from the end of surgery to first time analgesia were administered for the patient.
Total analgesia consumption: Total dose of medication given in mg within the first 24 h after the end of surgery.
Transversus abdominis planes block: Regional anesthesia technique that provides analgesia to skin and muscle of the anterior abdominal wall.
Demographic and perioperative characteristics
Sixty patients (30 patients in each group) were analyzed based on whether they received TAP-block or local anesthesia wound site infiltration after lower abdominal procedures at end of the surgery. There was no statistical significant difference between the two groups in demographic and perioperative characteristics such as age, sex, ASA classification and anesthesia induction agent used (P>0.05) as shown in Table 1. For analgesia, during the induction, intraoperative and post-operative period tramadol were used for all patients with no significant difference of Tramadol dose at induction and intraoperative period (Table 1).
| Variables | TAP-Block (n=30) | LAI Group (n=30) | P-Value |
|---|---|---|---|
| Age ( years ) | 41 (28-59) | 50 (26-61) | 0.673 |
| Sex | |||
| Male (n %) | 15 (50%) | 19 (63%) | 0.297 |
| Female (n %) | 15 (50%) | 11 (37%) | |
| ASA Status | |||
| ASA I (n %) | 10 (33%) | 11 (37%) | 0.787 |
| ASA II (n %) | 20 (67%) | 19 (63%) | |
| BMI# | 26 (26-28) | 26 (24-28) | 0.269 |
| Types of lower abdominal Procedures | |||
| C/S (n %) | 15 (50%) | 11 (37%) | 0.571 |
| Hernioraphy (n %) | 9 (30%) | 12 (40%) | |
| TVP (n %) | 6 (20%) | 7 (23%) | |
| Induction agent used | |||
| Thiopental (n %) | 8 (28%) | 8 (20%) | 0.851 |
| Propofol (n %) | 11 (37%) | 13 (43%) | |
| Ketamine (n %) | 11 (37%) | 11 (37%) | |
| Analgesia (Tramadol) before induction(mg) | 0.00 (.00-100) | 100 (0.00-100) | 0.2 |
| Intraoperative analgesia (Tramadol) received (mg) | 25.00 (0.00-50) | 0.00 (0.00-50) | 0.408 |
| Size of surgical incision site in (cm) | 13 (8-15) | 10 (8-15) | 0.232 |
| Duration of surgery (min) | 50 (45-80) | 58 (45-80) | 0.829 |
| Duration of anesthesia (min) | 58 (50-90) | 65 (50-90) | 0.947 |
| Estimated intraoperative blood loss (ml) | 540 (150-640) | 480 (100-570) | 0.196 |
Table 1: Demographic and perioperative characteristics of patient who undergo elective lower abdominal procedures. TAP: Transversus Abdominis Plane; LAI: Local Anesthesia Infiltration. Data are mean ± SD, median (range), or number (%).
Postoperative hemodynamic status between groups
After the surgery ended immediately at the recovery room, at 30 min, 1st h, 4th h and 6th h vital signs (PR, SBP, DBP, MAP) shows that statistical significant different between the two group (P<0.001) (Table 2). There was no statistical significant difference regarding the postoperative PR, SBP and DBP at 2nd h, 12th h and 24th h postoperatively between the two groups (Table 2).
| Vital sign | TAP-Block (n=30) | LAI Group (n=30) | P – value |
|---|---|---|---|
| Immediate recovery room (PACU) vital sign | |||
| PR (Median and IQR) | 114 (109-119) | 75 (67-89) | <.001* |
| SBP (Mean and SD) | 138 ± 9 | 11 ± 7 | <.001* |
| DBP (Median and IQR) | 84 (89-72) | 71 (67-74) | <.001* |
| Vital sign at 30 min | |||
| PR (Median and IQR) | 115 (110-117) | 72 (68-84) | <.001* |
| SBP (Mean and SD) | 137 ± 9 | 114 ± 7 | <.001* |
| DBP (Median and IQR) | 85 (76-89) | 70 (69-76) | <.001* |
| Vital sign at 1st Hour | |||
| PR (Median and IQR) | 103 (92-105) | 72 (68-82) | <.001* |
| SBP (Mean and SD) | 124 ± 10 | 113 ± 7 | <.001* |
| DBP (Mean and SD) | 76 ± 7 | 72 ± 6 | <.031* |
| Vital sign at 2nd Hour | |||
| PR (Mean and SD) | 85 ± 6 | 81 ± 11 | 0.081 |
| SBP (Mean and SD) | 118 ± 7 | 124 ± 9 | 0.079 |
| DBP (Median and IQR) | 74 (70-79) | 73 (70-82) | 0.923 |
| Vital sign at 4th Hour | |||
| PR (Mean and SD) | 87 ± 10 | 93 ± 14 | 0.056 |
| SBP (Mean and SD) | 116 ± 8 | 131 ± 7 | <001* |
| DBP (Mean and SD) | 79 ± 9 | 94 ± 6 | <.003* |
| Vital sign at 6th Hour | |||
| PR (Mean and SD) | 85 ± 8 | 92 ± 11 | <.006* |
| SBP (Median and IQR) | 113 (110-119) | 129 (125-133) | <001* |
| DBP (Mean and SD) | 74 ± 6 | 79 ± 6 | <001* |
Table 2: Postoperative hemodynamic status for 6 h in postoperative periods between TAP and LAI group. SD: Standard Deviation; IQR: Inter-Quartile Range; PR: Pulse Rate; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; *Statistically significant.
Comparison of time to first analgesia request and total analgesia consumption between groups
The Mann Whitney U test showed that the median time to first analgesia request in minutes were longer in TAP-block with 672 min compared to median time of 225 min in the LAI group (PCitation value<0.001). There were also statistical significant difference with regard to median Tramadol consumption within 24 h between the two group with P-value<0.001 as shown in Table 3.
| Variables expressed as Median (IQR) | TAP-Block (n=30) | LAI Group (n=30) | P-Value |
|---|---|---|---|
| Time to 1st analgesia request (Minute) | 673 (620-765) | 226 (195-235) | <.001* |
| Total analgesia consumption (Tramadol) | 100 (100-100) milligram | 175 (150-200) milligram | <.001* |
Table 3: Comparison of time to first analgesia request in minutes and total analgesia consumption in milligram between TAP &LAI groups at Empress Zewditu memorial Hospital, Ethiopia. IQR: Interquartile range; TAP: Transversus Abdominus Plane; LAI: Local Anesthesia Infiltration; *Statistically Significant.
Comparison of postoperative pain severity by verbal numeric pain rating scale
The Mann Whitney U test showed that the median VNRS score were lower in the LAI group at 30 min and 1st h postoperatively (P<0.05), but at 4th h, 6th h and 12th h there were statistical significant difference showing lower median pain score in TAP-block group when compared to the LAI group (p<0.001) as shown in Table 3. There was no statistically significant difference results at 2nd h and 24th h between the two group with P-value>0.05 (Table 4).
| Variables expressed as Median (IQR) | TAP-block (n=30) | LAI group (n=30) | P –value |
|---|---|---|---|
| VNRS @30 Min | 4 (4-5) | 2 (2-3) | < .001* |
| VNRS @1st Hour | 2 (2-3) | 2 (2-2) | <.014* |
| VNRS @2nd Hour | 2 (2-3) | 2 (2-3) | 0.157 |
| VNRS @4th Hour | 2 (2-2) | 5 (2-6) | < .001* |
| VNRS @6th Hour | 2 (2-3) | 4 (4-6) | < .001* |
| VNRS @12th Hour | 4 (3-6) | 6 (5-6) | < .001* |
| VNRS @24th Hour | 4 (4-6) | 5 (4-6) | 0.859 |
Table 4: Comparison of postoperative pain severity using VNRS score (0-10) between TAP and LAI group. IQR: Interquartile range; TAP: Transversus Abdominis Plane; LAI: Local Anesthesia Infiltration; VNRS: Verbal Numeric Rating Scale; *Statistically Significant.
According to our study the median time to first analgesia request in minutes were longer with median and IQR of 672l (765-620) min in TAP-block group compared to 226 (235-195) min in LAI group (p<0.001). It has been reported that TAP-block group not only reduced postoperative opioid need but also extended first analgesia application time in previous studies. This finding is in line with the study by Sivapurapu et al. done in lower abdominal surgeries under general anesthesia with the time to first analgesia longer in group TAP (148 ± 46.7 min) as compared to in LAI group (85.38 ± 38.07) (P<0.001) [9]. Also a study done in Pakistan showed that the time to first analgesia was longer in group TAP (8.92 ± 1.509 h) as compared to in group Infiltration (5.1 ± 1.971 h) with P value<0.05 [25]. Same results were reported in other studies [24,26].
The result of this study showed the median and inter-quartile Tramadol consumption within 24 h is 100 (100-100) milligram in TAP-block group compared to 175 (200-150) milligram in LAI group (p<0.001). This finding is in line with study done in turkey (RCT) in lower abdominal surgeries with total morphine requirement in the first twenty-four hours was significantly less in TAP-block group when compared with LAI group (22.15 ± 4.14 vs. 29.15 ± 3.93) (P<0.001) [9]. Another study in Egypt (2015) showed that total morphine requirement in the first twenty-four hours was significantly less in TAP-block group compared to LAI group (6.2 ± 1.04 vs. 8.4 ± 1.2) (P<0.001) [27].
Verbal numeric rating scale is regularly favored in clinical setting for pain scale measurement due to their simple administration, relatively consistent result and its correlation with that of VAS [22]. VNRS and VAS equally effective and interchangeably used for assessment of postoperative pain [23]. This study showed that during recovery room (PACU) time the median postoperative pain score (VNRS) were 2 (3-2) in LAI group and 4 (5-4) in TAP-block group (p<0.001). The comparison also shows lower median pain score 2 (2-2) in LAI group compared to 2 (3-2) in TAP-block group at 1st post-operative time (p=0.014). There were statistically significant different at 4th, 6th and 12th h showing lower median pain score in the TAP-block group compared to LAI group. There was no statistically significant different result at 2nd h and 24th h between the two groups.
Our finding is in line with Prospective RCT study done in Istanbul (Turkey) 2014. According to this study VNRS values immediately after operation in the TAP-block were found to be significantly higher than those of in LAI group (p=0.012). According to the same study VNRS values of LAI group at 2, 6, 12 and 24th h were found to be significantly higher than those of in TAP-block group [24]. Comparable results were also reported in the study done in India (2016) with no statistically significant difference of Visual Analogue Score (VAS) scores between the LAI group (2.32 ± 1.180) and TAP-block group (2.36 ± 1.186) at 1st h (P=0.905) and at the 3rd h, LAI group (3.04 ± 1.719) and TAP-block group (3.68 ± 1.651) (P=0.186) were recorded respectively [26].
This study shows that the immediately at recovery Room, at 30 min, 1st h, 4th h and 6th h vital sign (PR, SBP, DBP) shows statistical significant different (P<0.05). There was no statistical significant difference regarding the postoperative PR, SBP and DBP at 2nd h, 12th h and 24th h between the groups. The likely explanation for this difference is due to onset of the block. The main limitation of this study includes that the study was not randomized and variability in the performance of the block since different anesthetist was involved.
The first analgesia request was significantly longer in addition to less total analgesia consumption in the TAP-block group when compared to LAI group. Furthermore the TAP-block showed extended pain relief with lower pain VNRS but for immediate and early postoperative pain relief LAI group recorded lower pain VNRS score than the TAP-block group.
This work was funded by Addis Ababa University.
The authors have no conflicts of interest to declare.
Research registration number
Not required.
Availability of data and material
The data used in this study was collected by trained data collectors and authors are willing to share the data upon request from peer researchers.
We would like to thank Addis Ababa University College of Medicine and Health Science for funding this research. Our gratitude goes to supervisors, data collectors and study respondents. Finally, we would like to thank all those, who in one way or another have contribute in this work.