Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2022)Volume 11, Issue 6
Background and Purpose: This study aims to evaluate the safety and efficacy of a focused, monopolar, 360° energy distribution radiofrequency (RF) device for non-invasive treatment of dyspareunia in menopausal women with genitourinary syndrome of menopause (GSM). Methods: Thirty-five postmenopausal women with severe dyspareunia and GSM, underwent three sessions of monopolar radiofrequency therapy delivered once a month. Participants were evaluated at baseline and 2 months after their last treatment. The primary outcome was determined by assessing the patient's satisfaction with sexual intercourse at the 2-month follow-up visit. Secondary outcomes included the Vaginal Maturation Index (VMI), Maturation Value (MV), Bachmann´s Vaginal Health Index (VHI), and vaginal pH measurement. Safety outcomes included monitoring any possible complications and adverse events, and patient discomfort was evaluated by the Visual Analogue Scale (VAS). Results: A total of 83.3% of women initially incapable of sexual intercourse due to severe dyspareunia, were able to fully engage in sexual intercourse without pain 2 months post-treatment. VMI and VHI increased significantly in all parameters for all subjects (P<0.01). The Bachmann´s Vaginal Health Index Score (VHI) improved significantly (P<0.01) by 11.2 points. The analysis of vaginal cells demonstrated complete vaginal restoration with the presence of vaginal Lactobacillus flora, a normal acidic vaginal pH, the absence of inflammatory cells, and even the presence of superficial vaginal epithelial cells in initially severely atrophic tissue. Ninety-eight percent of subjects reported mild to no discomfort during their last treatment. No serious side effects throughout the course of the study were reported. Conclusion: The present study demonstrates a positive effect of a focused monopolar RF device for non-invasive and non-hormonal vulvovaginal tissue restoration affected by severe GSM. The results indicate clinical improvement in severe dyspareunia as a bothersome symptom of GSM. The treatment is effective and safe with high patient satisfaction.
Dyspareunia, GSM, Genitourinary, Menopause
Genitourinary syndrome of menopause (GSM), formerly referred to as vulvovaginal atrophy (VVA), is a widespread condition, affecting 27%-84% of post-menopausal women [1]. The new term, GSM, was introduced in 2013 to describe various nongenital signs and sexual symptoms since VVA (and atrophic vaginitis) but did not cover the full spectrum of symptoms and causes of the condition [2]. GSM is caused by a decrease in circulating estrogen levels at the onset of menopause. Genital symptoms include vaginal dryness, itching, tenderness, and burning. Sexual symptoms are lack of lubrication, dyspareunia, and impaired performance. Urinary symptoms such as urgency, dysuria, and recurrent urinary tract infections (UTIs) may occur [3]. All these symptoms negatively affect sexuality and quality of life. GSM features may appear in premenopausal hypoestrogenic women as well, manifesting in approximately 15% [4].
Primarily, the goal of GSM treatment is symptom relief. Conventional approaches for vulvovaginal symptoms include nonhormonal lubricants and moisturizers [5]. Hormonal and topical therapies mostly affect only the surface of the vaginal epithelium, while these therapies are being actively used [6]. An alternative solution is the use of non-invasive energy-based devices which affect vascularization and all levels of connective tissue in the vaginal canal. Besides laser energy (which lacks substantial safety and efficacy data) [7], non-ablative low-dose radiofrequency (RF) energy is widely used for the treatments [8,9]. The effect of RF devices is based on generating an electrical field that results in an oscillating electrical current that heats up intra-vaginal tissues to 40-45°C. These temperatures lead to increased local circulation and remodeling of collagen and elastin fibers located beneath the vaginal epithelium, in lamina propria. Increased blood flow provides nutrition to atrophic tissue and promotes its regeneration which results in the thickening of the vaginal epithelium. Lastly, collagen remodeling leads to tightening and strengthening of the vaginal wall [10,11].
Multiple studies reported reduced laxity of vaginal tissue [12- 14], improvement in symptoms of GSM [8,15,16], better sexual function, and satisfaction [8,13,14,17] following the use of RF devices. Ablation laser energy treatment is superficial and can only treat certain symptoms, whereas non-ablative monopolar radiofrequency (RF) penetrates and affects deeper tissues. The limitation of current RF devices is the design of the applicators which allows treating only one quadrant of the vaginal canal at a time. Such techniques may lead to undertreated or overtreated areas (so-called “hot-spots'') because of the non-homogeneous heating. In this study, 360° homogeneous heating has been improved upon by devising temperature tracking via dynamic impedance technology (DIT), which reduces the risk of under or overheating and significantly speeds up the time needed for treating the entire vaginal area, compared to quadrant heating procedure. Such a device has been successfully used for labial tissue rejuvenation and for the improvement of sexual function [18]. We hypothesize that the treatment could be beneficial also for women with GSM.
This study aims to investigate a 360° monopolar RF device with temperature tracking technology for the non-invasive treatment of dyspareunia in menopausal women with GSM.
A total of 35 postmenopausal women (6.3 ± 3.2 years postmenopause) aged 56.6 ± 3.4 years were enrolled in the study. Inclusion criteria were defined as follows: females with at least 3 years of severe dyspareunia as a bothersome symptom of GSM, incapable of sexual intercourse with penile penetration (coitus) for at least 12 months. Exclusion criteria included: sexually transmitted infection, sensitivity disorders or burns in the treatment area, metal implants, and conditions contraindicated by the device manual. No anesthesia was required.
The patients underwent treatment with Emfemme 360 device (BTL Industries Inc., Boston, MA). The treatment regimen consisted of three monopolar RF treatment sessions, each lasting for 8 minutes, delivered once a month. Before beginning treatment, the patient received verbal instructions about what to expect during the treatment procedure. The patient was seated in a gynecological chair and the device’s applicator utilizing heating at 360° was placed in the vaginal canal. The initial treatment setting was 65% and increased gradually during the procedure according to patient feedback and tolerance. During the treatment session, the operator steadily moved the applicator inward and outwards to ensure homogenous heating of the vaginal canal. The therapeutic temperature was continuously monitored during treatment via a temperature indicator screen. The operator communicated with the patient throughout the treatment to monitor safety. The protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. Informed consent was obtained from the patients.
Participants were evaluated at baseline and 2 months after the last treatment. Gynecological examination using a speculum and penetration with a transvaginal device applicator was done. The clinical improvement in dyspareunia was determined using a dichotomous questionnaire about satisfaction with sexual intercourse. Vaginal wall samples were collected using a swab and evaluated at the baseline and follow-up visits. The Vaginal Maturation Index (VMI) analysis was done under a light microscope (Carl Zeiss Axioskop microscope and Carl Zeiss Axiocam Color camera) by a blinded cytopathologist. Maturation Value (MV) was calculated from the VMI and the vaginal lining samples were further examined for the presence of lactobacillus flora, inflammatory cells, and superficial vaginal epithelial cells. In addition, evaluation included vaginal pH measurement and Bachmann´s Vaginal Health Index (VHI). The occurrence of any adverse events was monitored. Patients rated the comfortability of treatment based on a 10-point Visual Analogue Scale (VAS), no pain (zero) to unbearable pain (ten). Patient discomfort and a 5-point Likert scale. Patients expressed their satisfaction with treatment outcome percentage-wise (0% = dissatisfied; 100% = satisfied). The obtained before and after scores were compared and analyzed using the paired Student t-test, α=0.05.
All 35 patients completed the treatment regimen and underwent the examination at baseline and at 2 months post-treatment. At baseline, all patients reported severe dyspareunia. Two months post-treatment, dyspareunia was completely absent in 29 out of the 35 patients (83%).
Vaginal Health Index
The baseline measurement of the Bachman’s VHI score (scale 5-25) comprising the evaluation of ‘elasticity’, ‘fluid secretion type and consistency’, ‘pH’, ‘epithelial mucosa’, and ‘vaginal moisture’ was found to be 7.7 ± 1.2 on average, which corresponds to severe GSM. Two months post-treatment the average score significantly (p<0.01) increased to 18.7 ± 1.9 corresponding to a normal menopausal healthy vagina. Change in each section of the VHI was highly significant (p<0.01) with the highest improvement in pH and epithelial integrity. Figure 1 shows a detailed summary of VHI results (Figure 1).
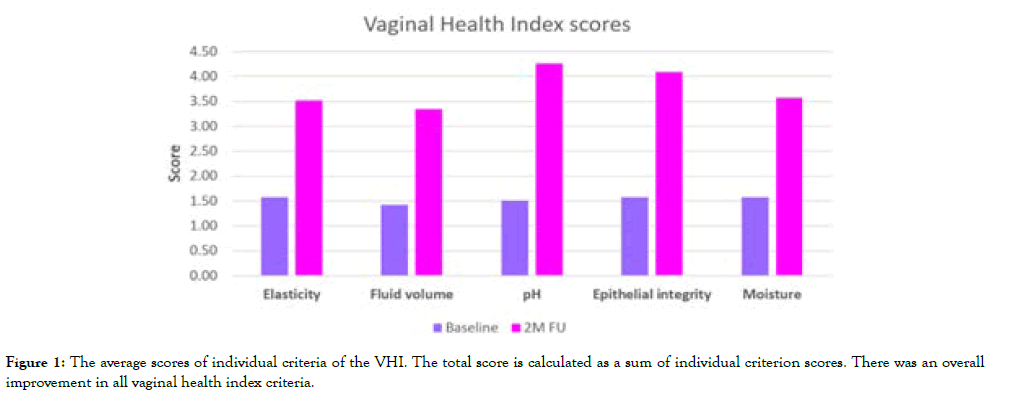
Figure 1: The average scores of individual criteria of the VHI. The total score is calculated as a sum of individual criterion scores. There was an overall improvement in all vaginal health index criteria.
The increase in pH score from 1.5 ± 0.5 to 4.2 ± 0.6 corresponds to the restoration of the pH acidity from a nearly neutral pH of 6.6 ± 0.8 at baseline to acidic pH of 4.6 ± 0.61 two months posttreatment.
Vaginal Maturation Index and Maturation Value
The proportion of para basal, intermediate, and superficial cells in samples, categorized by the vaginal maturation index (VMI) showed significant improvement (p<0.01) as the average baseline VMI improved from 65.1/34.9/00 (parabasal/intermediate/ superficial) to 26.9/66.6/6.6. The corresponding maturation value (MV) calculated from the VMI significantly (p<0.01) improved from 17.4±8.7to 39.9 ± 10.0 (0-100 scale).
Vaginal Flora, Leukocytes, and Inflammatory Cells
At baseline, normal vaginal flora consisting of lactobacilli (Döderlein flora) was present in only 10 out of the 30 patients (28%). Two months post-treatment, healthy vaginal flora quantity with Lactobacilli was present in 30 patients (86%). The improvement corresponded with the decrease of inflammatory cells. At baseline, the samples of 12 patients (34%) showed high levels of leukocytes, and 23 patients (66%) showed low levels of leukocytes. At 2 months follow-up, 15 patient samples (43%) had low leukocyte levels, while the remaining 20 (57%) did not contain any leukocytes. Inflammatory cells that were observed during pretreatment were absent in all samples post-treatment. An example of vaginal wall sample analysis results can be seen in figure 2.
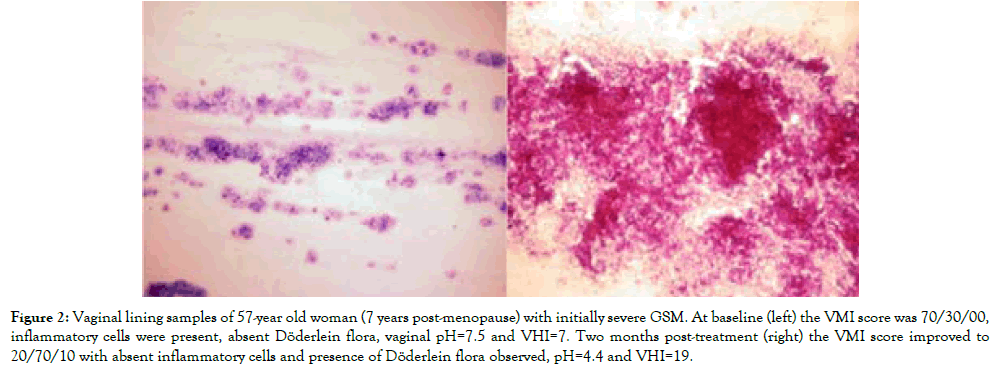
Figure 2: Vaginal lining samples of 57-year old woman (7 years post-menopause) with initially severe GSM. At baseline (left) the VMI score was 70/30/00, inflammatory cells were present, absent Döderlein flora, vaginal pH=7.5 and VHI=7. Two months post-treatment (right) the VMI score improved to 20/70/10 with absent inflammatory cells and presence of Döderlein flora observed, pH=4.4 and VHI=19.
Comfort and Satisfaction
At baseline, all patients reported painful gynecological examination using the speculum, and the transvaginal device applicator caused great discomfort, bleeding, and posterior vulvovaginal irritation. The average baseline VAS score was 6.6±1.3 (moderate to severe pain). At the 2-month follow-up visit, most of the patients indicated no to mild discomfort during gynecological examination with the speculum. The average VAS score decreased significantly (p<0.001) to 1.4±1.1 (mild to no pain) at the follow-up visit. Figure 3 demonstrates the exceptional difference between the first and last treatment.
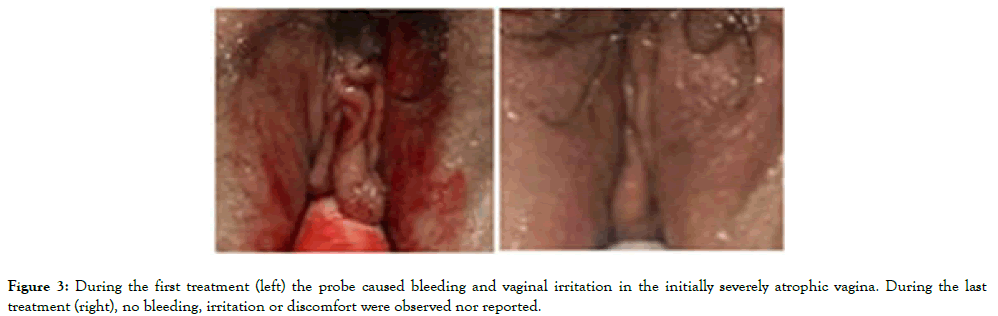
Figure 3: During the first treatment (left) the probe caused bleeding and vaginal irritation in the initially severely atrophic vagina. During the last treatment (right), no bleeding, irritation or discomfort were observed nor reported.
The overall patient satisfaction with the treatment results was high (92.9±6.7%). There were no dissatisfied patients. Moreover, at baseline 11 patients suffered from mild stress or mixed urinary incontinence, and 5 patients suffered from overactive bladder. All of these patients reported improvement and nearly 100% control of urination.
Side Effects and Complications
Immediate treatment effects were mild and transient, most of which occurred only during the first session and resolved within 1–2 days. The vaginal discharge occurred in 70% of patients, vaginal bleeding in 50%, introitus itching (45%), burning sensation (30%), and painful urination (20%). No complications or serious side effects were reported. No anesthesia, medications, or downtime was necessary.
This is the first study examining the efficacy of 360° monopolar RF technology for the treatment of GSM. The results presented herein show that the application of 360° radiofrequency in postmenopausal women with severe GSM leads to restoration of sexual life and vaginal wall quality, including the restoration of acidic vaginal pH and vaginal flora. The procedure effectively treated dyspareunia. VHI and VMI improved, reaching levels corresponding to those of menopausal women with normal vaginal health.
The novel Emfemme 360 device utilizes state-of-the-art temperature tracking technology in real-time, enabling the operator to monitor temperature throughout the therapy, thus, does not have to rely on patient feedback alone. The uniform heating is achieved through dynamic impedance technology, which continuously regulates RF energy flow. The impedance continuously changes; however, the results are constant since there is no fluctuation. The use of a temperature tracker gives the operator complete control over the treatment, which leads to consistent results as the risks of undertreating or over-treating are reduced. The DIT is a smart algorithm-like technology that measures vaginal tissue bioimpedance [19] 1000 times per second and, based on the measurements, adjusts the power in order to constantly deliver the desired energy. This feature avoids energy fluctuations during the treatment as the impedance changes with changes in temperature. Volumetric RF-generated heat is homogeneously distributed through the applicator tip in the treatment area. The highly advantageous uniform heat distribution ensures there are no hot-and-cold spots in the vaginal canal, resulting in short, and uncomplicated treatment administration. The vaginal probe has an ergonomic fit with various tips to suit different patients’ needs.
A single treatment session lasts for only 8 minutes, which is sufficient for heating the vaginal tissues up to desired temperature range of 40-45°C, and presumably triggers regenerative processes of neocollagenesis, neovascularization, and growth factor infiltration [20-22]. Increased levels of growth factor ultimately revitalize and restore the elasticity and moisture of the vaginal mucosa and induce epithelial thickening and structural changes [10]. The change in epithelial structure has been observed in vaginal lining cytologic analysis through an increase in VMI/MV in this study. The observed improvements correspond with previous studies using RF for restoring vaginal health in postmenopausal women such as Leibaschoff et al. [20] who reported improvement in VHI from 11.5 ± 0.67 to 19.3±2.01. However, the majority of RF studies does not include quantitative assessment and rely mainly on questionnaire evaluation [14,16,17,23] (Figure 4).
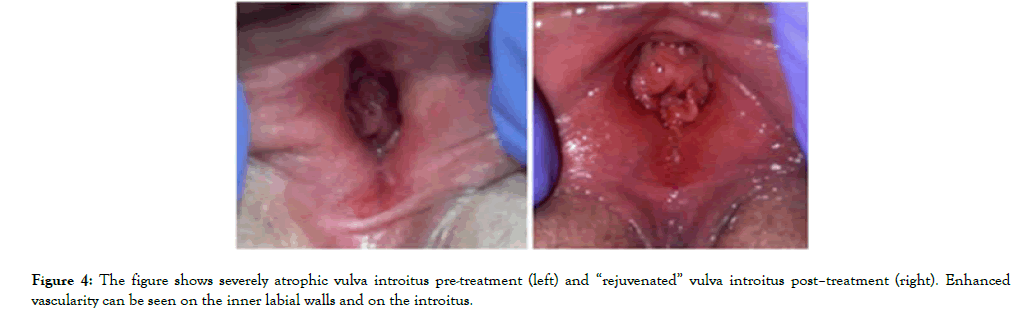
Figure 4: The figure shows severely atrophic vulva introitus pre-treatment (left) and â??rejuvenatedâ? vulva introitus postâ??treatment (right). Enhanced vascularity can be seen on the inner labial walls and on the introitus.
Besides the measured parameters, the patients reported improvement in the vulva appearance even though the treatment was intravaginal and did not include a labial procedure. The improvement in the vulva appearance is demonstrated in figure 4. Additionally, most of the patients reported improved sensitivity in the entire genital area, which was also documented by Alinsod et al [23]. This observation corresponds with the results of Lalji et al., [12]. who reported significantly reduced urine leakage after treatment procedure with the 360° RF technology. In a patient group that was composed only of women with severe GSM unable to engage in sexual intercourse (coitus) for three or more years, the results showed complete restoration of the vaginal health. Based on these outcomes it may, therefore, be assumed that the treatment could reverse certain symptoms of GSM.
Nevertheless, the patient group (35 post-menopausal women) was rather limited. Although such samples cannot be used for generalized conclusions, the results give a good overview of the expected treatment outcomes. Patients were evaluated 2 months post-treatment, and certainly, this time period is insufficient to provide information about the sustainability of results. Thus, future studies should include longer follow-ups to address the longevity of the outcomes and whether additional treatments to maintain the achieved results are necessary. A comparative arm group and evaluation of tissue biopsies may be incorporated in upcoming studies. The major strength of this study is that multiple methods for evaluating treatment effects were used to avoid inferring biased conclusions, which could occur when using a single evaluation method, as well as to provide deeper insight into the patient’s condition. The statistically significant changes and participants’ recovered sexual function (despite prior severe dyspareunia that prevented penetrative sexual intercourse) demonstrated in this study provides strong evidence for the treatment efficacy.
Vulvovaginal monopolar radiofrequency resulted in highly significant clinical improvements in all measured parameters in postmenopausal women with severe dyspareunia GSM. Most of the patients recovered the ability to have satisfying sexual intercourse, after years of no sexual life. The monopolar 360° technology is an effective, safe, easy, and time-saving treatment for severe GSM symptoms and dyspareunia without any serious adverse events.
The authors declare that there is no conflict of interest.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Citation: Aznar F, (2022) 360° Radiofrequency Technology for Treatment of Dyspareunia in Women with Genitourinary Syndrome of Menopause. J Women's Health Care 11(6):585
Received: 19-May-2022, Manuscript No. JWH-22-17569; Editor assigned: 21-May-2022, Pre QC No. JWH-22-17569(PQ); Reviewed: 04-Jun-2022, QC No. JWH-22-17569; Revised: 08-Jun-2022, Manuscript No. JWH-22-17569(R); Published: 15-Jun-2022 , DOI: 10.35248/2167-0420.22.11.585
Copyright: © 2022 Aznar F, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.