
Advances in Pediatric Research
Open Access
ISSN: 2385-4529

ISSN: 2385-4529
Research Article - (2023)Volume 10, Issue 2
Introduction: Maternal mental health has been considered a global health issue by many health partners. Studies have shown that about 10% of pregnant women and 13% of post-partum mothers experience one form of mental health disorders, especially depression. In developing countries, almost 16% of pregnant women and 19.8% women experience depression after childbirth. The prevalence rate of Post-Partum Depression (PPD) in the northern part of Ghana was estimated as 33.5% in 2018 and 16.8% in 2019. PPD has been linked to poor health seeking habits during and after pregnancy, leading to poor birth outcomes. We aimed at identifying prevalence rate of PPD and its adverse effects on pregnancy and birth outcomes in Tano North Municipality.
Methods: An institutional records and child welfare books were reviewed alongside a survey. An analytical cross-sectional design was employed for this study using quantitative methods. The Edinburgh Postpartum Depression Scale [EPDS] was used to screen mothers who utilized the postnatal services at the Municipal Hospital (St. John of God Hospital, Duayaw Nkwanta) for this study. Three-hundred and eighty-six respondents were selected using purposive and systematic sampling technique. The questionnaire used for this study constituted the demographic characteristics of postpartum women and standard 10 points questions from [EPDS].
Results: Results from the study depicts that 44% of the respondents were within the ages of 31-40 years, and 43.8% with ages 21-30 years. Majority (39.9%) of the women had no formal education. Majority (79.8%) of the respondents was married and 75.13% employed. On severity range of PPD, 69.4% of the postpartum women were mildly depressed, 8.6% moderately depressed and 1.3% severely depressed. Ante natal attendance was 74.9% for women who visited ANC within the 1st trimester and 22.0% within the 2nd trimester. Logistic analysis showed that not being married (AOR=6.198, 95% CI=2.926-13.128), unemployed (AOR=1.587, 95% CI=0.778-3.235), women with 3-4 children were associated with increased risk of developing PPD. Complications in birth outcomes included babies with low birth weight (13.5%), 19.7% mild asphyxia and 11.9% severe asphyxia.
Conclusion: PPD was prevalent among 14.8% of postpartum mothers involved in the study, Socio-demographic factors of being single, unemployed and having 3-4 children were positive predictors of the condition. Obstetric risk factors of experiencing pregnancy and/or birth complications, having had a stillbirth and having had a baby born with weight less than 2.5 kg were also found to positively associate with the occurrence of PPD. We recommend early case detection and holistic treatment of cases in among women with PPD.
Children; Infant; Depression; Postpartum
Maternal mental health remains a public health problem globally of which Ghana is no exception. The World Health Organization in 2015, estimated that 10% of pregnant women and 13% of post-natal women experience one of the mental health disorders especially depression. The condition is more prevalent among women in developing countries. Almost 16% of pregnant women and 19.8% women after childbirth experience depression. A more recent meta-analysis indicated that in developing countries, about 20% of postpartum women experience clinical depression [1]. The prevalence rate of Post-Partum Depression (PPD) in the northern part of Ghana was estimated as 33.5% in 2018 and 16.8% in 2019. Another study in Ghana in 2018 reported a prevalence rate of PPD as 7% ranging from mild to severe [2].
PPD has been linked to poor health seeking behaviors during and after the pregnancy period as well as adverse pregnancy and birth outcomes [3]. These adverse birth outcomes may include stillbirth, perinatal deaths, low birth weight, delivery complications and other psychological problems [4]. PPD when not treated leads to poor psychological and physical wellbeing of both mother and newborn as well as on other siblings in the family and subsequent maladjustment in children [5].
Available data from high-income counties cites PPD as a major mental health problem, which disturbs the new mother’s adaption, disables functioning community, family participation and child’s development [6]. However, there is no medical package for helping healthcare providers to link mental, reproductive and child health services.
It is no surprise, that women in Tano North Municipality continue experiencing PPD, which in recent time have contributed to adverse birth outcomes in the Municipality. The numerous attentions are not drawn on the relationship between PPD, maternal and child outcomes. There is also no study conducted on PPD in the Tano North Municipality. This therefore does not show any clear cut direction towards the attainment of the Sustainable Development Goal 3 (SDG 3).
Effective postpartum care in the community can prevent short, medium and long-term consequences of unrecognized and poorly managed problems. Therefore, it is important that postpartum care be integrated into primary health care. However, there appears to be inconsistency about the timing and content of routine care for mothers and infants. This paper therefore used descriptive cross-sectional study to determine the prevalence, demographic and risk factors of postpartum depression among Postnatal Clinic Attendants at St John of God Hospital, Duayaw Nkwanta.
Aims of the study
The study aimed at identifying prevalence rate of PPD and its adverse effects on pregnancy and birth outcomes in Tano North Municipality.
Specifically, the study was to identify:
1. The prevalence rate of PPD in Tano North Municipality.
2. The association between demographic characteristics and PPD.
3. The perceived adverse effects of PPD on pregnancy and birth outcomes in Tano North Municipality.
Analytical cross-sectional study design was employed for this study using quantitative methods. Quantitative methods in the form of review of institutional records and survey using questionnaires and a standard tool for screening for PPD among women Edinburgh Postpartum Depression Scale [EPDS]. Mothers that utilized the postnatal services at the Municipal Hospital (St. John of God Hospital, Duayaw Nkwanta) were recruited for the study. Three-hundred and eighty-six respondents were selected using purposive and systematic sampling technique.
The sample size was computed based on Cochran (1977) sample size calculation for categorical data and is computed as follows with the formulae indicated below:

From the formulae,
n=sample size in relation to the confidence interval of 95%
p=an estimated proportion of postpartum mothers utilizing the Municipal hospital (50%)
e=the margin of error accepted or prepared to be accepted by the researcher (here since the confidence interval was 95%, it implies that 5% margin of error is anticipated).
q=1-p=0.5
From a pre-testing of the data collection instrument 0.50 proportions of postpartum mothers. This gives p=0.50 and q=1-p=0.5, in which case the sample size becomes,
St. John of God Hospital was purposively selected due to its position as the referral point for Tano North Municipality. Systematic sampling technique was also employed in this study to choose respondents at an interval of 3. At the initial stage, a sample frame (register of postpartum mothers that attended PNC services) was obtained and at an interval of three (3), chose postpartum mothers that utilize the health facilities at the period of the study. The total number of postpartum mothers was 1158 and so looking at the computed sample size, a systematic sampling strategy was adopted with a sampling interval of 3. A number was generated with excel (6th person on the register) which became the starting point and from there every third mother was considered for the study till the required sample was achieved.
Data collection procedures
Primary and secondary source of data were collected. Questionnaires were administered to postpartum mothers by the research team personally in order to obtain quality data for the study. The questionnaire constituted the demographic characteristics of postpartum women and standard 10 points questions from [EPDS]. EPDS was developed to ascertain PPD among women. Each question on the EPDS was given answers with scores 0 to 3 and was analyzed based on a maximum score of 30. Data were collected using the local language to enable the respondents especially those who cannot read and write to understand the questions and answer appropriately. The Mental Health unit and the Biostatistics unit of the hospital were tasked for the data collection in order to ensure data validity. Data collection was done from the month of February to August (2022).
The secondary source of data was employed to ascertain adverse pregnancy and birth outcomes reported by each sample unit of the study. By so doing, a checklist was designed for documentary review from the delivery registers. Additionally, maternal and child health records was included for documentary review if the woman was not delivered at St. John of God Hospital.
Institutional study right was obtained from St. John of God Hospital management. Permission was sought from the Public Health Department of the hospital whiles written and oral consent were sought from postpartum mothers that participated in the study. The Researchers explained the purpose and benefits of the study to the participants.
Data analysis technique
The Edinburgh Postpartum Scale Calculator was used to compute the overall PPD for each of the sample unit. According to the calculator, a score of more than 10 suggests moderate or severe depression [7]. Socio-demographic, history of pregnancy complication and birth outcomes data and overall score of postpartum depression were entered in Microsoft Excel (version 2016).
Data was exported from the Microsoft Excel into STATA, where codes were generated for build in commands and analysis commands.
To obtain the severity ranges, the recommended EPDS severity ranges by McCabe-Beane scale and Walker, et al. [8] was used to build a command for the ranges as shown below;
• None or minimal depression (0–6),
• Mild depression (7–13),
• Moderate depression (14–19),
• Severe depression (19–30).
Data analysis was done using STATA version 14. Both descriptive and inferential statistical models were used for the study. For the inferential statistical model, logistic regression analysis was performed at a confidence interval of 95% and a significant value of 5% (P-value=0.05). Test values less than 0.05 were considered significantly associated.
Demographic characteristics of postpartum depression
Results from Table 1 depicts that 44% of the respondents were within ages 31-40 years and 43.8% with ages 21-30 years. From the table, there were more women with no formal education, 39.9%, followed by 32.9% with basic and 11.9% secondary education. On marital status, 79.8% of the respondents were married whiles 20.2% unmarried. The table further shows that 75.13% of the women were employed whiles 24.9% were unemployed. Women with children 1-2 formed 44.6%, with 41.7% having 3-4 children. The table also shows 74.9% of the women had visited ANC within the 1st trimester and 22.0% within the 2nd trimester (Table 1).
| Visit 1 | Visit 2 | Visit 3 | Visit 4 | Visit 5 | |
|---|---|---|---|---|---|
| (21 days) | (2 months) | (4 months) | (6 months) | (12 months) | |
| Informed consent | X | - | - | - | - |
| Selection criteria | X | ||||
| Randomization | X | ||||
| Weight (g) | X | X | X | X | X |
| Length (cm) | X | X | X | X | X |
| Head circumference (cm) | X | X | X | X | X |
| Triceps and subscapular skinfolds (mm) | X | X | X | ||
| Mid-arm circumference (cm) | X | X | X | ||
| Feces characteristics (consistency and nº bowel movements/day) | X | X | X | X | X |
| Digestive tolerance (flatulence, | X | X | X | X | X |
| vomiting and regurgitation) | |||||
| Daily behavior (restlessness, colic, nocturnal awakenings) | X | X | X | X | X |
| Overall assessment of the parents/ r. legal | X | X | X | X | X |
| Tolerability of infant formula | X | X | X | X | |
| 3 days dietary questionnaires’ | X | X | X | X | |
| Gut microbiota count and distribution in feces (qPCR and NGS analysis) | X | X | X | X | |
| Morbidity | X | X | X | X | X |
Note: X: Absence
Table 1: Gantt chart of the trial.
Prevalence of postpartum depression
Results from Figure 1 illustrate 14.8% PPD with score above 10. On severity range of PPD, 69.4% of the postpartum women were mildly depressed, 8.6% moderately depressed and 1.3% severely depressed as illustrated in Figure 2.
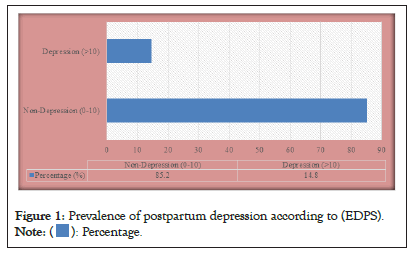
Figure 1: Prevalence of postpartum depression according to (EDPS). 
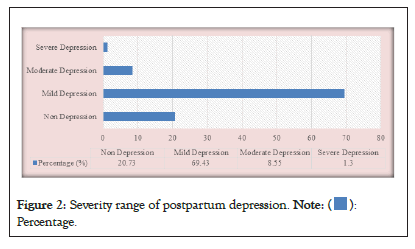
Figure 2: Severity range of postpartum depression. 

Association between socio-demographic characteristics and postpartum depression
Logistic regression analysis was performed to determine the relationship between demographic characteristics and PPD. Unadjusted logistic regression analysis was first performed after which the significant variables were adjusted for. Table 2 depicts results of the regression analysis of socio demographic characteristics and postpartum depression.
| Formula 1 (Nutriben Innova 1 or INN) | Formula 2 (Nutriben or STD) | |
|---|---|---|
| *Fat | Vegetable oils and fat milk | Vegetable oils |
| *GOS | Yes | Yes |
| Proteins | 8% less protein per 100 kcal than the standard. 70:30 Whey protein: Casein enriched with α-lactalbumin (20% of total proteins) | 60:40 whey proteins: casein. α-lactalbumin (10 % of total proteins) |
| DHA/ARA | -AA 24 mg/100 kcal | -AA 10 mg/100 kcal |
| -DHA 24 mg/100 kcal | -DHA 10 mg/100 kcal | |
| BPL1TM HT | Yes (thermally inactivated) | No |
Note: *Same amount per 100 kcal for both formulas
GOS: Galacto-oligosaccharides; DHA: Docosahexaenoic Acid; ARA=Arachidonic Acid; BPL1TM HT: Bifidobacterium animalis subsp. lactis
Table 2: Comparison of the composition of the study formulas.
Age, level of education and first time visit to ANC were not statistically related to PPD (P>0.05). However, not being married was associated with increased risk of developing PPD (AOR=6.198, 95% CI=2.926-13.128). Again, unemployed women were also associated with increased risk of developing PPD (AOR=1.587, 95% CI=0.778-3.235). Additionally, women with 3-4 children were associated with increased risk of developing PPD than women with 5-6 children (AOR=4.315, 95% CI=2.113-8.810).
Pregnancy and birth outcomes
64.8% of the respondents had no complications during pregnancy whiles 35.2% had complications during pregnancy. Again, 88.9% encountered no complications during delivery whiles 11.1 had complications. 13.5% of the respondents had children with birth weight less than 2.5 kg. About a third (68.4%) of the women had non-asphyxiated babies, 19.7% mild asphyxia and 11.9% severe asphyxia. 91.2% of the women had their children born alive whiles 8.8% recorded stillbirth.
Association between postpartum depression and adverse birth outcomes
Complications in pregnancy was associated with increased risk of developing PPD (AOR=2.665, 95% CI=1.054-6.738). Results indicates that women with delivery complications were associated with increased risk of developing PPD (AOR=43.247, 95% CI=13.682-136.697).
Additionally, women with birth weight less than 2.5 Kg were significantly associated with increased risk of developing PPD(AOR=36.692, 95% CI=12.175-110.579). The table also reveals that women with severe asphyxiated babies were significantly associated with increased risk of developing PPD than those with mildly asphyxiated babies (AOR=3.834, 95% CI=0.904-16.252). Women that experienced stillbirth were also significantly associated with increased risk of developing PPD (AOR=29.324, 95% CI=8.227-104.532) as revealed.
This study sought to determine the prevalence and associated factors of PPD among mothers seeking post-natal care at the St. John of God Hospital, a referral hospital in the Tano North Municipality of Ghana. This is one of few studies conducted among rural and peri-urban women in Ghana to determine demographic, pregnancy, labour and birth outcomes associated with PPD, and the first in the study municipality. The findings of this study provide evidence for important health policies of health education and interventions to reduce the burden of postnatal care among new mothers. The sample was predominantly youthful with more than seventy percent having had less than secondary education, married, employed and having initiated ANC in the first trimester of their pregnancy. More than a third of the sample reported pregnancy complications and about 11% having birth complications. About 8% of the total sample had had a stillbirth.
Out of the total of 386 mothers, a PPD pprevalence of 14.8% was recorded. This rate is much higher than a previous Ghanaian study which found a prevalence of 7% in an urban setting but consistent with other results from the Northern part of Ghana [1,3]. Other studies have reported different prevalence rates depending on the setting, country, socioeconomic status and stage of the postpartum period [4]. PPD has been shown to be associated with hormonal changes that contribute to the vulnerability of being depressed. Frican women after childbirth are required to engage in activities that promote the growth of their new-borns whilst at the same time caring for other members of the household. Even though a period of rest has been traditionally practised in Ghana (usually for the first 40 days) where the new mother is expected to rest and reduce domestic chores, this new role of motherhood may exert feelings of frustration emanating from breastfeeding problems, feelings of helplessness, lack of sleep and loneliness. The severity of depression ranged from mild to severe with more than half recording mild depression and a little over one percent recording severe depression. Mild to moderate depression have been described as self-limiting episodes which may usually require psychosocial and psychological psychotherapy [9].
The results further revealed a significant association between the status of being non married women and PPD (OR=5.388, AOR=6.198). A possible explanation can be in two ways (i) since this period of parenting thrives well in a setting of stable social support, a woman who is unmarried may lack this support from the father of the new-born and/or (ii) societal and cultural norms regarding single motherhood. The presence of a husband/partner improves the new mother’s health by offering the opportunity to manage the stress of breastfeeding, sleeplessness and a break from new-borns who cry excessively. Research is conclusive on the fact the babies who cry excessively may not breastfeed well causing anxiety in mothers who may themselves become depressed. Other infantile behaviours that have been found to be associated with PPD include but are not limited to irritability and inconsolability. The offer of paternal support during this phase is likely to promote the growth of the mother and child while at the same time fostering a paternalinfant bonding [10]. The existence of such phenomena as social stigma, abuse, gossip and shame have been shown to have an association with PPD among single mothers and in traditional conservative rural and peri urban communities such as the study area, chances are that these may also be predictors, though the scope of this research did not cover issues of social stigma. Future research can explore factors such as emotional and social stigma on single motherhood and how they may predict PPD.
Stressful events in people’s lives have been reported as triggers to depression. Pregnancy and childbirth can be described as major life events that cause significant physical, mental and hormonal changes in women. Even though some women experience uneventful pregnancies, others develop conditions such as bleeding, miscarriages, amniotic fluid and placental complications, preeclampsia amongst others. Having a history of labour complications have also been shown to have a positive association with PPD. The process and duration of labour can sometimes result in perineal tears, excessive vaginal bleeding, maternal fatigue, emotional instabilities which can eventually lead to distress and depression [4]. Results from the logistic regressions found that experiencing complications during pregnancy and/or delivery and having a stillbirth were positive predictors of PPD. Women who reported having had complications during their pregnancy were twice more likely to be depressed than those who had no complications. Currently, post-natal care practices in Ghana include skilled health care in labour and delivery, as well as the immediate post-partum period, two visits within the first week of life (3rd and 7th day) and at 6 weeks as advocated by the WHO [9]. These are to promote healthy behaviours in the new mother and detect early warning signs of illness in the dyad please check the word for me. However, it is possible that before the sixth week visit, some women may have issues of maladjustments in their homes. We therefore advocate for the reinforcements of home visits by community volunteers and Community Health Nurses and Workers (CHNs and CHWs) to continuously encourage and screen for postpartum psychiatric disorders such as (i) Postpartum Blues (PBs), (ii) PPD, (iii) Postpartum Psychosis (PP), (iv) Postpartum Post-Traumatic Stress Disorder (PTSD), and (v) postpartum anxiety and Obsessive-Compulsive Disorder (OCD). Where feasible, as is done in the Focused Antenatal Care (FANC), a postpartum nurse can be assigned to a new mother as her primary care provider with whom there will be regular communication and remote check-up [11]. For a sample with little or no formal education, new mothers, fathers and/or caregivers will benefit from the institution of childbirth education classes where constant education is given on early warning signs, reassurances given for those going through familial and personal problems, echoed by radio and TV advertisements and education in local languages on signs and symptoms of various mental disorders linked to the period following childbirth. These efforts duly complemented by home visits by CHNs/CHWs will reduce further exacerbation of the episodes that may require medications and hospitalizations.
PPD was prevalent among 14.8% of mothers interviewed in this study. Socio-demographic factors of being single, unemployed and having 3-4 children were positive predictors of the condition. Obstetric risk factors of experiencing pregnancy and/or birth complications, having had a stillbirth and having had a baby born with weight less than 2.5 kg were also found to positively associate with the occurrence of PPD. Early detection can foster a holistic treatment including familial and social support, reassurance and counseling by qualified and skilled health providers as well as pharmacologic treatment where necessary. This is one of few studies done in the area to explore the prevalence of the condition and its association with socio-demographic and obstetric risk factors. As a crosssectional study, no causal implications can be drawn between the variables and PPD. However, these results give empirical insight into the existence and magnitude of the condition in the municipality to inform intervention and management strategies. We recommend that future Ghanaian studies look at the social and infant factors that are likely to associate with PPD especially among single mothers and those who already have children.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Amponsah SK, Apenkwa J, Asante LS, Boakye-Boateng SK, Donkor M (2023) Prevalence, Demographic and Obstetric Risk Factors of Postpartum Depression among Postnatal Clinic Attendants at St John of God Hospital, Duayaw Nkwanta. Adv Pediatr Res. 10:058.
Received: 06-Jun-2023, Manuscript No. LDAPR-23-24913; Editor assigned: 09-Jun-2023, Pre QC No. LDAPR-23-24913 (PQ); Reviewed: 23-Jun-2023, QC No. LDAPR-23-24913; Revised: 30-Jun-2023, Manuscript No. LDAPR-23-24913 (R); Published: 07-Jul-2023 , DOI: 10.4172/2385-4529.23.10.058
Copyright: © 2023 Amponsah SK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.