Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Case Report - (2020)Volume 10, Issue 4
Neuropsychiatric Systemic lupus Erythematosus (NPSLE) is a common manifestation in systemic lupus erythematosus, however pure psychosis without no other CNS symptoms is less common. Differentiating between lupus psychosis and steroid induced psychosis can even be more challenging. In this case report, we present a 53-year old African American female with longstanding SLE overlapped with dermatomyositis manifested with acute psychotic events. The late onset of psychosis and the absence of typical lupus flare serological test results differed from classical NPSLE. Especially, in the setting of withdrawing steroids several months prior to presentation. The exclusion of other etiologies and a trial of steroid prompted quick resolution of her symptoms.
Lupus erythematosus; Steroid; Psychosis; Neuropsychiatric
Systemic Lupus Erythematosus (SLE) is a chronic autoimmune process with a variety of clinical and serological presentations involving multiple organ systems, including the nervous system. Neuropsychiatric systemic Lupus Erythematosus (NPSLE) predominantly affects central and peripheral nervous systems. The most common symptoms in NPSLE are fatigue [1], headache, cognitive deficit, depression, less commonly, lupus headache, seizures, and cerebrovascular events or myelopathy [2]. Psychosis remains rare, accounting for only 1.53% in SLE patients in a large international cohort study [3]. It was estimated that 19% to 38% of patients with NPSLE manifest before or around the time of diagnosis of SLE [4]. This case report aims to describe a 53-yearold female with a history of longstanding SLE without previous psychiatric history who presented with acute psychosis, in the absence of any other alternative etiology of psychosis.
A 53-year-old African American female with longstanding systemic lupus erythematosus (SLE), no previous psychiatric history, and treated latent syphilis was sent by her family and the police to the emergency department for a multitude of hallucinations, delusions, even with suicidal and homicidal ideations. At baseline, she was a pleasant person with normal behavior who was compliant with her medications. Two weeks prior to admission, she was noticed to behave distinguished from her baseline, progressively worsening violent, erratic, and irrational. One week prior to admission, she was diagnosed with a urinary tract infection, however, she refused antibiotics. Meanwhile, she threatened to take all of her medications at once to commit suicide, as well as to kill her children. She was reported to throw glass dishes at her family. She thought that her healthy grandchildren were dead and that her currently alive daughter died from a car accident. She obstinately believed “a guardian angel holding a spear” next to her as she “saw and heard the voice of the angel”. During this time, she also refused to eat, drink, take her medications, or shower. She was wearing a garbage bag while defecating and urinating on herself. Otherwise, she suffered from dyspnea, which remained stable compared to the baseline. She denies any alopecia, sicca syndrome, chest pain, new skin rash, any Raynaud’s phenomenon, any headache or any muscle weakness.
Regarding the past medical history, the diagnosis of SLE was established 7 years prior to admission, with oral ulcers, rash, leukopenia and positive Antinuclear Antibody (ANA). She was started on hydroxychloroquine since then. Methotrexate was initiated and then discontinued due to the finding of interstitial lung disease. She was unable to tolerate mycophenolic acid due to side effects. She developed overlap syndrome with dermatomyositis in the setting of rash, muscle weakness, Raynaud’s phenomenon, as well as interstitial lung disease 3 years prior to admission. She received 1 dose of rituximab at the time of overlap syndrome diagnosed. Azathioprine was started combined with low-dose prednisone and hydroxychloroquine with remission of SLE and dermatomyositis. Azathioprine was discontinued 1 year prior to admission and prednisone was tapered off 3 months prior to admission. She was compliant to hydroxychloroquine until 1 week prior to admission. Besides, she was diagnosed with latent syphilis 6 years prior to admission and finished the course of penicillin. Prior to hospitalization, the patient did not start on any new medications or herbal supplements.
On physical examination, the patient was labile, confused; she was afebrile on admission, but developed low-grade fever of 100.2°F (37.8°C) during hospitalization, tachycardic up to 124 beats per minute, hypotensive with blood pressure of 96/51 mmHg, oxygen saturation 98% on ambient air. Physical exams were notable for an oral aphthous ulcer, but no other pertinent finding. Mental status examination showed normal conscious, normal orientation, disturbed perception, guarded cooperation, limited recent memory, intact remote memory, intact concentration, normal motor, speech, appeared anxious, circumstantial thought process, noted for paranoia and limited insight.
Upon arrival at the emergency department, she was found hypoglycemic with random blood glucose of 56 mg/dL, quickly improving after dextrose was given. However, her mental status remained unchanged. Initial laboratory tests showed White Blood Cells (WBC) count 2.70 × 103/μL, neutrophils 66%, no anemia or thrombocytopenia. On hospitalization day 2, her WBC dropped to 1.60 × 103/μL. Venous blood gas with mild metabolic contraction alkalosis, with no lactic acidosis of 1.4 mmol/L. Comprehensive metabolic panel was notably with mild electrolyte abnormalities, including hyponatremia of 133 mEq/L, hypokalemia of 3.2 mEq/L, and hypochloremia 93 mEq/L, liver function and kidney function, Creatine kinase (CPK) within normal ranges. There was no abnormality in the coagulation profile. Vitamin B12, folate, Thyroid Stimulating Hormone (TSH), and cortisol levels were within normal limits. Urine toxicology screen was completely negative and urinalysis was unremarkable. Inflammatory markers were elevated with C-reactive Protein of (CRP) 25.4 mg/L, Erythrocyte Sedimentation Rate of (ESR) 74 mm/hr. The syphilis enzyme immunoassay was positive for IgG antibody and the rapid plasma reagin test was reactive with 1:4 on titer. The HIV screening test was negative. The immunology panel was positive for ANA titer greater than 1:640, speckled pattern. However, anti-double stranded DNA antibodies and complements, including C3 and C4, were both within normal limits. No significant findings were detected on head computerized tomography without contrast. The brain magnetic resonance imaging and angiography were performed with no active abnormality, both (Figures 1A, 1B and 2). To determine the etiology of her acute psychosis, lumbar puncture was preceded. Cerebrospinal Fluid (CSF) studies demonstrated WBC at 14/uL, predominantly mononuclear cells of 64%, mildly elevated total protein at 57 mg/dL, and normal glucose at 49 mg/dL.; N-methyl-D-Aspartate (NMDA) receptor antibodies were negative. Venereal Disease Research Laboratory test (VDRL) in CSF wasere nonreactive. Bacterial, viral and fungal tests were negative, including CSF culture, mycobacterium, herpes, enterovirus, cryptococcus. 2 doses of intravenous haloperidol 1 mg were given without any significant change of her mental status.
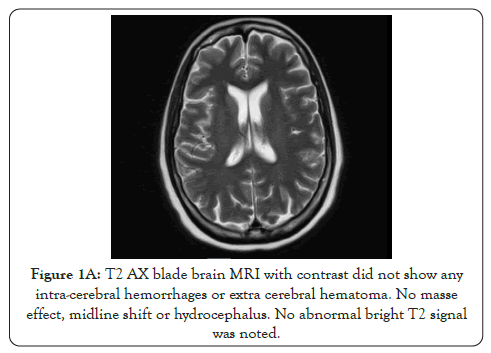
Figure 1A: T2 AX blade brain MRI with contrast did not show any intra-cerebral hemorrhages or extra cerebral hematoma. No masse effect, midline shift or hydrocephalus. No abnormal bright T2 signal was noted.
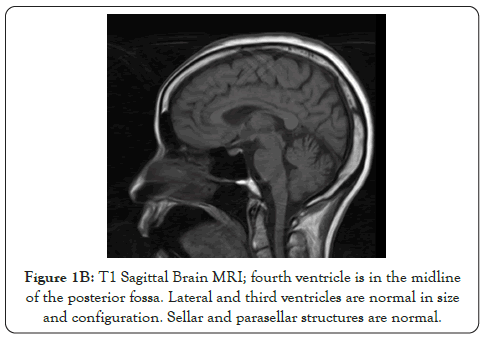
Figure 1B: T1 Sagittal Brain MRI; fourth ventricle is in the midline of the posterior fossa. Lateral and third ventricles are normal in size and configuration. Sellar and parasellar structures are normal.
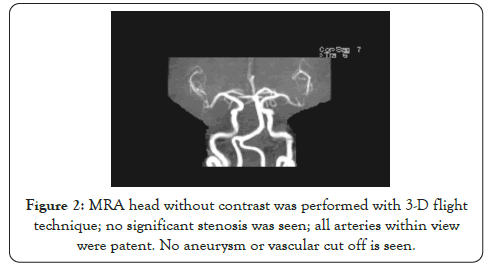
Figure 2: MRA head without contrast was performed with 3-D flight technique; no significant stenosis was seen; all arteries within view were patent. No aneurysm or vascular cut off is seen.
Based on the findings above, her acute presentation of psychosis was considered most likely secondary to lupus psychosis. Neurosyphilis was less likely as she finished penicillin treatment 6 years prior to admission and VDRL test was negative in CSF. Urinary Tract Infection (UTI) was diagnosed 1 week prior to admission, while the patient did not take the antibiotics due to poor insight. However, the urine analysis was not suggestive of bacteriuria and clinical manifestations not consistent with UTI upon admission. Septic meningitis was ruled out via lumbar puncture and there were no other sources of infection. Therefore, infection was not considered as a trigger of altered mental status in our patient. Metabolic derangement, ischemic encephalopathy, subarachnoid hemorrhages were less likely from the above results. Prednisone was completely stopped prior to admission; therefore, corticosteroidsinduced psychosis was unlikely. Thus, the patient was given methylprednisolone 80 mg every twelve hours for 3 days, tapering down to prednisone 10 mg daily. No antipsychotic medications barrier, autoantibody-mediated neural destruction, vasculopathy or coagulopathy [11,12]. Anti-DNA antibodies were found to insult the blood-brain barrier and cross-react with the N-methyl-D-aspartate (NMDA) receptor to damage brain tissue in SLE [10]. But there was no statistical significance with psychotic events in SLE [13]. In a meta-analysis, psychotic symptoms are associated with increased titers of serum anti-ribosomal P antibodies [13], but with only 9.9% positivity [3].The anti-NMDA receptor antibody was undetectable and other antibodies were not tested in our case.
The initial attempt of antipsychotic, such as haloperidol, in the emergent situation, has not achieved significant effect on our patient. Antipsychotics alone are not sufficient enough to fully control psychiatric symptoms in lupus psychosis [5]. The quick response to steroids in our patient further confirmed our hypothesis. The adjunctive immunosuppressant was not applied as our patient responded well to sole corticosteroid treatment. However, around two-thirds of patients with lupus psychosis might require immunosuppressant, even biologic agents [3]. The psychotic events put patients with SLE with a high burden on quality-of-life, but with an improvement after symptoms resolution [3]. In a cohort study, 93% of patients did not experience any recurrent psychotic events [3,14,15]. Therefore, the prompt recognition and treatment were given other than the 2 initial doses of haloperidol. The psychotic symptoms improved significantly and her mental status was back to the baseline since the initiation of the steroids. The monitoring lab shows WBC back to 2.6 × 103/μL range, around the baseline. Oral ulcers had resolved. The patient was discharged with low-dose prednisone and continued on hydroxychloroquine.
AAcute psychosis is relatively rare in patients with SLE, with an estimated rate of 1.53% to 11.3% [3,5,6]. Our patient met the criteria of psychosis with delusions, hallucinations without insight, inducing social functioning impairment [7]. It is crucial to consider infections as a differential diagnosis as the symptoms may mimic NPSLE and even trigger lupus flare, especially under long-term immunosuppressive regimens [8]. The use of 0.75-1.0 mg/kg/day of prednisone upon the psychotic events should take corticosteroidinduced psychosis into account [5]. And the management of steroid use in infection or corticosteroid-induced psychosis is opposed to that of NPSLE. The combination of detailed history, comprehensive test results and exclusion of other causes in our case placed lupus psychosis highly on our differential.
The acute psychotic event occurred 7 years after the diagnosis of SLE in our patient. It was estimated that one-fourth of patients presented with psychiatric symptoms 2 months prior to diagnosis of SLE and 80% of patients with NPSLE, 90% of psychotic events manifest within 3 years of diagnosis [3]. This late onset of psychosis should not be regarded as exclusion of lupus psychosis, but needed to be more cautious about the other differential diagnosis.
The SLE Disease Activity Index-2000 (SLEDAI-2k) in our patient accounts for 11 points, including 8 points for psychosis, 2 points for oral ulcer, 1 point for leukopenia. Despite the possibility of benign leukopenia in African American ethnicity, the lower level of WBC than her baseline more points to lupus flare. Other than the psychosis, oral ulcer and leukopenia, our patient did not experience other signs of lupus flare, such as alopecia, pyuria, hematuria, proteinuria; sign of pleuritis, pericarditis, elevated antidsDNA antibody, and low complement level, etc. There remains controversy on the associations between NPSLE and other aspects of SLE disease activity. Segui et al. discovered the correlation between low C3, high anti-dsDNA levels and higher psychosocial distress, mainly among the generalized anxiety, depression or panic disorders [9]. It was considered that some manifestations of NPSLE were discorded with lupus flare or severity [10].
There was no previous case report on psychosis primary to dermatomyositis. Moreover, no new rash, muscle weakness or any elevation of CPK posed a low possibility of psychosis due to her overlap syndrome with dermatomyositis.
Until now, the pathogenesis of NPSLE remains not completely clear. Thus, there still lacked validated and unequivocal laboratory tests to determine the associations between neuropsychiatric events and SLE. It may be secondary to insult to blood-brain barrier, autoantibody-mediated neural destruction, vasculopathy or coagulopathy [11,12]. Anti-DNA antibodies were found to insult the blood-brain barrier and cross-react with the N-methyl-D-aspartate (NMDA) receptor to damage brain tissue in SLE [10]. But there was no statistical significance with psychotic events in SLE [13]. In a meta-analysis, psychotic symptoms are associated with increased titers of serum anti-ribosomal P antibodies [13], but with only 9.9% positivity [3].The anti-NMDA receptor antibody was undetectable and other antibodies were not tested in our case.
The initial attempt of antipsychotic, such as haloperidol, in the emergent situation, has not achieved significant effect on our patient. Antipsychotics alone are not sufficient enough to fully control psychiatric symptoms in lupus psychosis [5]. The quick response to steroids in our patient further confirmed our hypothesis. The adjunctive immunosuppressant was not applied as our patient responded well to sole corticosteroid treatment. However, around two-thirds of patients with lupus psychosis might require immunosuppressant, even biologic agents [3]. The psychotic events put patients with SLE with a high burden on quality-of-life, but with an improvement after symptoms resolution [3]. In a cohort study, 93% of patients did not experience any recurrent psychotic events [3,14,15]. Therefore, the prompt recognition and treatment of lupus psychosis plays an important role.
The later onset of psychotic events and the absence of typical lupus flare serological results distinguished our case from typical neuropsychiatric systemic lupus erythematosus. The psychological assessment and the exclusion of other alternative etiology of psychosis are crucial to diagnose lupus psychosis, especially with atypical presentations in our case. Prompt management provides patients with lupus psychosis with promising prognosis.
Citation: Bizanti A, Ni R, Ahmed A, Regmi M (2020) While Balancing Steroid in SLE, the Brain was Victimized. Rheumatology (Sunnyvale). 10: 267. DOI: 10.35248/2161-1149.20.10.267.
Received: 01-Oct-2020 Accepted: 15-Oct-2020 Published: 22-Oct-2020 , DOI: 10.35248/2161-1149.20.10.267
Copyright: © 2020 Bizanti A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.