Medical & Surgical Urology
Open Access
ISSN: 2168-9857
ISSN: 2168-9857
Case Report - (2019)Volume 8, Issue 1
We represent a-65-year-old male patient presented with indwelling left JJ stent for obstructed solitary kidney drainage. The obstruction was due to internal iliac artery aneurysm, had been managed by trans-femoral self-expandable coated endovascular stenting. This patient readmitted with recurrent attacks of hematuria with displaced JJ stent and rising serum creatinine twice. In the first admission, the patient was managed by JJ stent readjustment and Percutaneous Nephrostomy tube (PCN) and was discharged safely. Again, he presented with UAF associated with aggressive hematuria mostly due to vascular endoleak rupture. The patient developed severe sepsis and multiple organ dysfunction syndrome.
Uretero-arterial fistula; Ureteric stent; Aneurysm
UAFs are rare and lethal emergency which require a multidisciplinary approach for both analysis and management. Primary UAFs progress with barrier destruction between aneurysm and ureter.
Secondary UAFs form in cases of previous irradiation, pelvic cancer or surgery. Clinical picture varied from asymptomatic to flank pain, hematuria and shock, diagnosed by angiography, ureteral pyelography, Computed Tomography up to surgical exploration.
Mortality associated with UAFs had been reported from 10% to 38% [1,2].
We reported a case of secondary UAF with internal iliac artery aneurysm.
Also, we present a proof for disseminated infection between urinary and vascular systems through UAF.
We reported a 65-years-old male, hypertensive with grade I renal impairment. Presented with indwelling left JJ stent which was used for bypass obstructed solitary left kidney by incidentally discovered internal iliac artery aneurysm 6×6 cm (Figure 1). Later on, successful trans-femoral, self-expandable, covered stent placement for that aneurysm was done and patient maintained on oral anticoagulant.
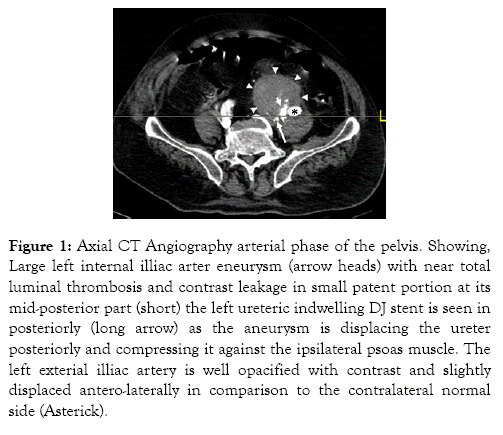
Figure 1: Axial CT Angiography arterial phase of the pelvis. Showing, Large left internal illiac arter eneurysm (arrow heads) with near total luminal thrombosis and contrast leakage in small patent portion at its mid-posterior part (short) the left ureteric indwelling DJ stent is seen in posteriorly (long arrow) as the aneurysm is displacing the ureter posteriorly and compressing it against the ipsilateral psoas muscle. The left exterial illiac artery is well opacified with contrast and slightly displaced antero-laterally in comparison to the contralateral normal side (Asterick).
He was admitted with rising serum creatinine 5.7 mg/dL (basal was 1.7 mg/dL).
Follow up Non Contrast CT (NCCT) showed displaced upper coil of JJ stent at the level of aneurysm with subsequent moderate back pressure changes in solitary left kidney. Also, filled pelvicalyceal system, ureter and bladder with fresh blood density hematoma. The displaced JJ stent was replaced by another one easily under cover of retrograde pyelography. Unfortunately, serum creatinine was still rising to 7.6 mg/dL, so left PCN fixed for better drainage. After Serum creatinine dropped till its basal level with JJ stent in place, patient discharged safely without hematuria. PCN was removed after two weeks with assessing serum creatinine and it was 1.6 mg/dL. Two weeks later, patient came with recurrent attacks of hematuria, fever, serum creatinine was 5 mg/dL, high leucocytic count and back pain with displaced JJ stent at iliac ureter again. Initial suspicious was that upper coil of JJ stent inside the aneurysm that increase in size (10×9) cm with presence of vascular endoleak. Patient was managed again by PCN fixation and NCCT (Figure 2) was done revealing air locules at both pelvicalyceal system and iliac aortic aneurysm. Also, there was increase of endoleak size with positive cultures isolated from both PCN and blood and was serratia mercenes.
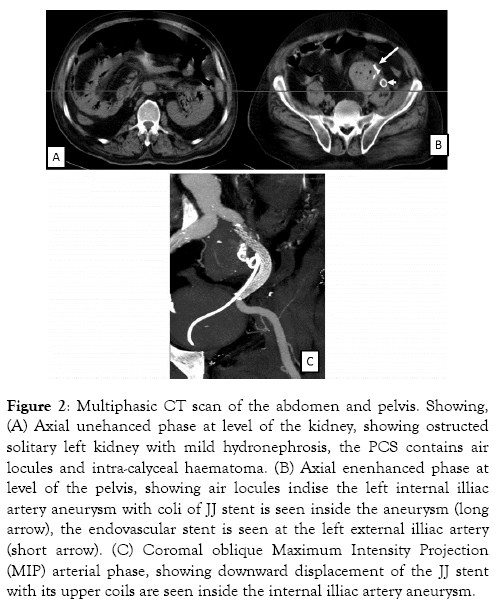
Figure 2: Multiphasic CT scan of the abdomen and pelvis. Showing, (A) Axial unehanced phase at level of the kidney, showing ostructed solitary left kidney with mild hydronephrosis, the PCS contains air locules and intra-calyceal haematoma. (B) Axial enenhanced phase at level of the pelvis, showing air locules indise the left internal illiac artery aneurysm with coli of JJ stent is seen inside the aneurysm (long arrow), the endovascular stent is seen at the left external illiac artery (short arrow). (C) Coromal oblique Maximum Intensity Projection (MIP) arterial phase, showing downward displacement of the JJ stent with its upper coils are seen inside the internal illiac artery aneurysm.
Patient was transferred to intensive care unit with signs of sever septicemia; hypotension, tachycardia and fever maintained on antibiotics and vasopressors. Two days later, the patient developed severe sepsis with multiple organ failure. Both serum creatinine and liver enzymes were elevated then aggressive hematuria developed suspecting ruptured aneurysm and patient died.
UAF caused by inflammation and associated degenerative course that prompt destruction of the ureteral wall with the adjoining vasculature [2]. Displacement of JJ stent at the aneurysm level and its dislodgment is affected by pulsatile arterial flow which came in direct contact with the ureter. Extra luminal compression by mechanical expansion of aneurysmal mass thought to motivate irritation, producing collapse between these structures [1]. UAF with internal iliac artery aneurysm is a rare entity representing just 9.5% [1].
Secondary UAFs, representing 85% of total UAF, encourage fistula formation by causing extensive pelvic fibrosis, augmenting local inflammation, or by redirecting relevant structures within close proximity of one another [3]. With a proper diagnosis for UAF, mortality rate decrease to 8% with possibility for increase up to 64% if misdiagnosed [1].
Different modalities in treatment of UAFs were identified including arterial ligation, bypass grafting, direct artery repair, ureterectomy, ligation/removal of ureter, nephrectomy and nephroureterectomy, coiling, or stenting of ureters [1].
Endovascular Abdominal Aortic Aneurysm Repair (EVAR) is placing a stent-graft within the aorta to exclude the aneurysm from arterial circulation and reduce the risk of rupture. Vascular endoleak is the most common complication post EVAR resulting in blood flow outside the stent-graft but within the aneurysm sac. It occurs in 15%-25% of patients. Endoleak ensuing for aneurysm expansion, leading to erosion, aortoenteric fistula formation and higher mortality rate resulting from rupture.
Endovascular stent infection had mortality in less than 1% of cases [4]. But, Stent-graft treatment of potentially infected sites remains controversial. Communication with the urinary tract certainly introduces a source of infection with no definite previous proof for that, [5]. Presence of simultaneous air locules indicating infection by gas forming organism in pelvicalyceal system and aneurysm carried very poor prognosis leading to death. Based on our finding, we recommend PCN as the optimum drainage method if suspecting UAFs in case of associated aneurysm with vascular stent.
UAF are rare and life threatening condition. Predisposing conditions in the formation of these fistulae include prolonged ureteral stent usage in a patient who has had vascular pathology. The best way for the physician to diagnose UAF is the presence of gross hematuria. PCN could be offered as a choice for drainage of urinary system to prevent UAF.
Citation: Elbaset MA, Hashem A, Atwa A, Badawy MA, Osman Y (2019) Micturition and Defecation, Neuro-Chemical Control. Med Sur Urol 8:217. doi: 10.35248/2168-9857.19.8.217
Received: 28-Dec-2018 Accepted: 20-Feb-2019 Published: 27-Feb-2019 , DOI: 10.35248/2168-9857.19.8.217
Copyright: © 2019 Elbaset MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.