Internal Medicine: Open Access
Open Access
ISSN: 2165-8048
ISSN: 2165-8048
Research Article - (2023)Volume 13, Issue 5
The quality measures (SEP-1) for compliance with a standardized "bundled" treatment protocol vary widely across hospitals although adherence to bundles is known to improve patient outcomes. The variation in bundle compliance implies the interdependence of a broad array of positive and negative factors associated with patient conditions, clinician competencies, care process and teamwork, and environment. We have a limited understanding of the true complexity behind bundle compliance (or non-compliance) in clinical practice. This article thus aimed to understand frontline care providers’ perceptions associated with sepsis bundle compliance at an acute care hospital in the Midwest. We surveyed 68 clinicians (of nurses and physicians from emergency department) about their perceived difficulties, educational gaps, and confidence with sepsis knowledge, along with sepsis-related education and experience. The survey responses were encoded to a data matrix and transformed using the mathematics of Singular Value Decomposition (SVD) to build a dimensional representation, dubbed “perceptual space”, of collective perceptions surrounding bundle compliance. Two principal dimensions comprising the perceptual space were identified, the first distinguishing “all-or-nothing” versus multifaceted, analytical reasoning for recognition, and the second splitting between system-wide versus case-specific foci for intervention. Both dimensions explained the majority (65.5%) of the total variability in the input data matrix. Additionally, statistical tests revealed that clinicians’ experience with sepsis, level of medical education, and clinical role had significant relationships with perceptions. The proposed representation method has potential for guiding compliance-enhancing strategies in a prospective manner, as opposed to the current quality measures (SEP-1), which is retrospective and outcome-driven.
Sepsis; Sepsis bundle compliance; Survey; Perceptual space; Multiple correspondence analysis
ANOVA: Analysis of Variance; CMS: Centers for Medicare and Medicaid Services; ED: Emergency Department; EMR: Electronic Medical Records; HO sepsis: Hospital-Onset sepsis; LOS: Length- Of-Stay; MANOVA: Multivariate Analysis of Variance; MCA: Multiple Correspondence Analysis; PA: Physician Assistant; RN: Registered Nurse; SA: Situation Awareness; SBT: Simulation-Based Training; SEP-1: The Severe Sepsis and Septic Shock Management Bundle; SIRS: Systemic Inflammatory Response Syndrome; SVD: Singular Value Decomposition
Multifaceted problem of sepsis management in hospitals
SSepsis is a life-threatening organ dysfunction due to a dysregulated host response to infection [1]. Worldwide, it is the number one cause of death in hospitals, and 48.9 million diagnosed cases lead to 11.0 million deaths per year (accounting for 19.7% of all global deaths) [2]. In the United States, sepsis accounted for approximately 1.7 million adult cases and 270,000 subsequent deaths in 2014 and the annual number of sepsis cases has been on the rise [3,4].
In addition, it is the most expensive condition treated in U.S. hospitals, with an estimated cost of $23.7 billion per year [5].
In particular, Hospital-Onset (HO) sepsis, which accounts for 1 in 8 sepsis cases, is associated with even worse outcomes than community-onset sepsis (i.e., sepsis that patients already have upon arrival at the hospital). A retrospective review of large-scale Electronic Health Records (EHR) during hospitalizations revealed that the mortality rate for HO sepsis is twice as high as that for community-onset sepsis; and compared with hospitalized patients who never developed sepsis, HO-sepsis patients bore a three-time higher risk of death and substantially longer hospital Length-of- Stays (LOS) [6]. Despite those severe outcomes and hazard risks, it is unclear to what degree sepsis-related outcomes are due to characteristics of patients (e.g., comorbidities and severity of illness) versus the performance of sepsis management [6].
Standardized sepsis guidelines and a group of quality measures from the Centers for Medicare and Medicaid Services (CMS), also known as “bundle” have been promoted as an effective sepsis management strategy when adhered to, as they can improve the timing of treatment, leading to lower mortality rates and hospital LOS [7-10]. However, despite the evidence that bundle compliance improves patient outcomes, implementation of protocols and bundles in practice remains suboptimal and national compliance rates for bundle adherence are still low [11,12]. Bundle compliance rates and its effects on outcomes vary widely across hospitals and the environments of care delivery (such as staffing ratio) on top of patient-related factors [6,8,13]. Such wide variability associated with sepsis bundle compliance may hint that we have a limited understanding of the true complexity of the problem.
Early recognition and treatment of sepsis is essentially a clinical problem, requiring a set of knowledge of pathophysiology, clinical criteria, and interventions, along with a keen sense of clinical judgment and experience. From another perspective, it is increasingly being viewed as a systems problem requiring continuous improvement and stakeholder involvement to ensure the quality of underlying processes [14-16]. The evidence advocates for various forms of quality-improvement interventions because of the positive outcomes seen with enhanced compliance [12,17-19]. However, time, leadership, and other resources are required to successfully initiate and sustain a campaign of such system-wide interventions. Little has been reported about their hidden costs, such as the burden of increased alerts and workloads due to the intensive monitoring load (and its subsequent impact on other critical patients under clinical workflows), or the consequences of overcompliance if care providers rush to initiate bundles based on insufficient symptom presentation. In that regard, compliance may be reduced to a problem of judgment and decision-making under uncertainty because all patients are unique cases, and early interventions could often precede without the full presentation of symptoms [20]. On the other hand, other researchers allude to the problems of team dynamics, communication, and the sharing of situation awareness [21]. Indeed, there is some truth to all of the above perspectives, because a failure of appropriate sepsis management has multiple root causes [22].
When a problem is multifaceted, and it requires multiple domain experts to handle, it can be difficult to devise an effective solution, because various stakeholders have different perceptions and priorities in the face of the “problem space” [23]. The immediate challenge for sepsis bundle compliance is therefore to have a common representation of all related problems, based on which stakeholders can build a consensus on how to understand its complexity and devise effective strategies through education and best practice solutions.
Motivation of study
Recently, to promote compliance, an acute care hospital in the Midwest (the Carle Health Systems located in Urbana, Illinois) implemented a new sepsis workflow in its electronic medical record system (i.e., Epic EMR) for the nursing and physician providers to use. Early compliance metrics captured in 2023, however, were low, at around 5%. That is significantly below the national average of compliance rates and warrants the introduction of effective strategies to enhance compliance and thus sepsis outcomes, specifically in the Emergency Department (ED) [8,24]. Strong compliance strategies must be set up to address key problems associated with the care providers’ sepsis management in their own work contexts.
To that end, this article aims to explore frontline care providers’ perceptions of the difficulties associated with early recognition and treatment of sepsis in the ED and to identify strategic directions for future sepsis education and training. We conducted a survey to collect opinions primarily on perceived barriers and educational gaps, and applied the fundamental mathematics of Singular Value Decomposition (SVD) to construct a “perceptual space” that enables a concise representation of stakeholders’ views of a problem seen from diverse standpoints [25,26]. Our results consist of the principal “dimensions” comprising that space, extracted from the collection of survey responses, and their use to help explain the variation in compliance over different levels of sepsis knowledge, education, and practice. With our emphasis on education and best practice, the proposed space representation method can be used to devise compliance-enhancing strategies tailored to certain healthcare settings.
Related works: Factors and barriers to compliance
The literature provides useful conjectures about factors that might lead to compliance, or the lack thereof. First, knowledge of sepsis is essential for compliance (including knowledge of the definition and mechanisms of sepsis, the Systemic Inflammatory Response Syndrome (SIRS) variables associated with sepsis, screening criteria for septic shock and severe sepsis, interventions, and sepsis bundle elements [27]. Despite that importance, substantial variations in nurses’ levels of knowledge have been reported worldwide, ranging from poor to moderate performance in recalling the relevant knowledge components [27-29]. Such variations are strongly associated with the nature of acute care settings. For example, emergency nurses employed at hospitals with level 3 Intensive Care Units (ICU) scored significantly higher than their colleagues in other settings [29]. For those who tend to treat sepsis patients less frequently in their clinical practice, however, education can effectively help compensate for the knowledge gap [29,30].
In addition, another class of experiential, practically driven, and often subjective “tacit” knowledge is crucial for early recognition and diagnosis of clinical presentations (i.e., accurate interpretation of signs and symptoms, laboratory values, and different levels of severity) [27,31,32]. In the absence of a gold-standard diagnostic test, clinicians are often required to interpret a myriad of nonspecific physiological and laboratory abnormalities among patients with suspected sepsis, and, as a result, overall inter-rater agreement in sepsis diagnoses is poor [33].
Third, upon accurate recognition of sepsis or septic shock, the appropriate way to execute the recommended treatment procedures (including measurements of lactate levels, obtaining blood cultures, and administration of antibiotics and vasopressors) is still not straightforward, as it requires a sequence of decision-making that is tailored to the complex clinical environment, context of care, and patient conditions [27,34]. For example, a survey of 122 critical care nurses on their perceived barriers to the decision to administer antibiotics revealed that 23%–38% of the respondents would delay the initiation of antibiotics to comply with the institution’s other protocols associated with blood pressure and hypotensive conditions [35]. In addition, substantial variation was observed among the respondents regarding the sequence in which fluid, antibiotic, steroid, and vasopressor therapies should be administered. Furthermore, lack of information about a patient’s medical history or baseline cognitive function, and uncertainty about patient conditions associated with comorbidities or altered levels of consciousness, could pose even greater challenges to decision-making [27].
Fourth, team-based, collaborative procedures devised to alert for and manage sepsis could also complicate compliance. Teamwork essentially requires all team members to share and maintain awareness of all relevant states (including sepsis symptoms recognized and IntraVenous (IV) antibiotics ordered and delivered to the unit). Especially in fast-paced and unpredictable ED settings, nursing workloads could substantially affect the ability to initiate sepsis bundles in a timely manner [35].
Survey design
Based on our literature review, a survey questionnaire was designed to help build a comprehensive understanding of care providers’ perceptions and educational gaps associated with sepsis bundle compliance. The survey consisted of four sections: Section A, clinical experiences, education, and role associated with sepsis management; Section B, sepsis knowledge and training; Section C, perceived barriers to compliance; and Section D, potential gaps in sepsis education. The survey study plan was reviewed under the Category-2 Exempt regulations and approved (#23CCC3746) by the hospital’s Institutional Review Board in July 25, 2023 [36].
Data collection and analysis
The survey responses were collected from frontline care providers in the ED using the online survey tool, Qualtrics (Seattle, WA). The period of data collection was from July 26 to August 17 in 2023. The data was preprocessed and organized into the data matrices representing the respondents’ perception, education, and experiences; see Figure 1. The purpose of data analysis are three- fold: Construct a perceptual space with key dimensions extracted from the collection of responses on perceived problems, map educational gaps on to the perceptual space constructed, so that new strategic direction of sepsis training is inferred, and identify significantly contributing factors to the perception from clinical education, experiences, and sepsis knowledge, which will shed light on the tactics to implement the new strategies [1-3]. A data matrix contains a set of numerical or categorical variables in the columns. A row in the matrix represents an individual respondent. As a result, the five data matrices (C, E, K, P, G) were generated, corresponding to the respondent’s clinical education, clinical experiences, sepsis knowledge, perceived problems, and educational gaps, respectively.
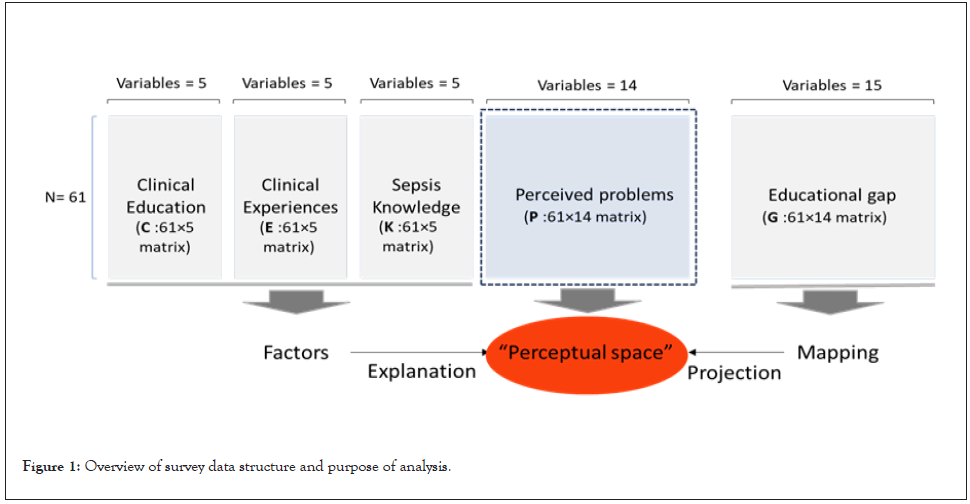
Figure 1: Overview of survey data structure and purpose of analysis.
Construction of perceptual space
Perceived problems may vary widely depending on individual experiences and attitudes at work. The set of common problem categories identified from the literature was presented to the respondents to help recall their own issues, along with free-form responses to describe the nature of the problems in more detail. The text responses were later parsed to either creates additional problem categories or merged into existing ones. The data matrix of perceived problems, P, has 14 problem categories as the column variables. A respondent marked one or more of the categories, which forms a row vector of 0s and 1s. A total of 61 row profiles were collected to represent a variety of perceptual structures.
Dimensional reduction techniques based on the Singular Vector Decomposition (SVD) are useful to obtain a concise spatial representation of diverse row and/or column profiles. Our input format makes Multiple Correspondence Analysis (MCA) a viable option to carry out dimensional reduction and construct perceptual space [37].
Suppose the input matrix P has rows and columns, the computational algorithm for Correspondence Analysis (CA) conducts the following procedures to calculate the matrix of standardized residuals, perform SVD, extract the principal coordinates of columns, and find principal inertias equations1-4.
MCA extends the CA algorithm to the matrix of multiple categorical variables Q, where each category may break down to a set of dummy variables as columns. The input matrix P for MCA is thus comprised of smaller blocks of dummy variables, and the total inertia is the weighted sum of the inertias of the block matrices.
Mapping and prediction
Once a perceptual space is constructed, along with its key dimensions identified, this space can be used in two ways. First, a set of factors associated with experiences and education will be examined to confirm its relationship to the space. The existence of linear relationships between controllable factors and the abstract space will help predict and improve an individual’s location within that space. Second, mapping a set of educational gaps to the perceptual space helps project new educational directions that are promising to modify existing perception patterns.
Descriptive statistics
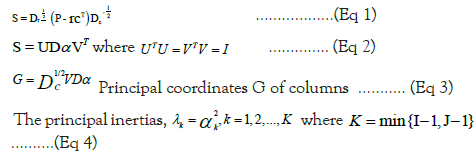
A total of 68 care providers at ED responded to the survey, and 7 responses were filtered out for incomplete data (i.e., the time to run the entire survey was less than one minute, or less than one-half of the survey items were answered). Figure 2 summarizes the profiles of 61 survey respondents, balanced between registered nurses (N=32; 54.2%) and physicians/Physician Assistants (PA) (N=27; 45.8%) (top left). A great number of RNs had a bachelor’s (53.1%) or a master’s degree (15.6%). In the group of physicians/ PAs, most (77.8%) had a doctoral degree (top right). Taking both nurses and physicians/PAs together, a great number of clinicians (N=48; 78.7%) was experienced with sepsis patients for at least 4 years or more (bottom left). Most clinicians (N=50; 83.4%) approximated their frequency of septic case encounters per week as at least 3 or more, and a few (N=4; 6.7%) approximated 20 or more (bottom right).
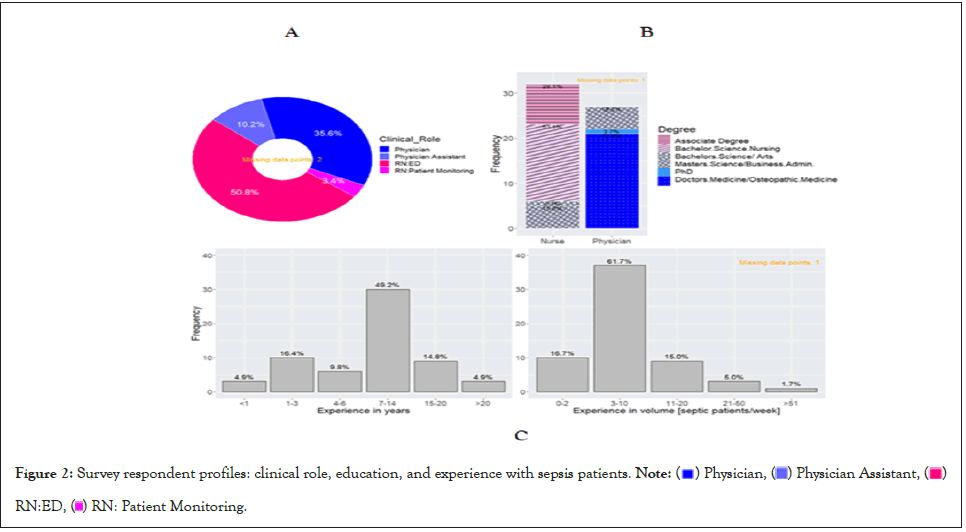
Figure 2: Survey respondent profiles: clinical role, education, and experience with sepsis patients. Note: ( ) Physician, (
) Physician, ( ) Physician Assistant, (
) Physician Assistant, ( )
RN:ED, (
)
RN:ED, ( ) RN: Patient Monitoring.
) RN: Patient Monitoring.
Beyond general medical education, one survey item asked to mark specific type(s) of sepsis education or training received among classroom lecture, self-directed online course, simulation- based training, and clinical placement (e.g., residency, clinical rotations, or other clinical training experiences) (Table 1). Self- directed online course, either alone or in combination with other modalities, accounted for the majority of responses (N=44; 72.1%). About one-half of the respondents (N=34; 55.7%) were trained using multimodal curriculums, but exposure to simulation-based training was not as frequent (N=19; 31.0%).
| Classroom lecture | Self-directed online course | Simulation-based training | Clinical placement | Frequency | |
|---|---|---|---|---|---|
| Count | % | ||||
| ✔ | 14 | 23 | |||
| ✔ | ✔ | ✔ | ✔ | 11 | 18 |
| ✔ | 10 | 16.4 | |||
| ✔ | ✔ | ✔ | 8 | 13.1 | |
| ✔ | ✔ | ✔ | 7 | 11.5 | |
| ✔ | ✔ | 3 | 4.9 | ||
| ✔ | ✔ | 2 | 3.3 | ||
| ✔ | ✔ | ✔ | 2 | 3.3 | |
| ✔ | 1 | 1.6 | |||
| ✔ | ✔ | ✔ | 1 | 1.6 | |
| ✔ | 1 | 1.6 | |||
| ✔ | ✔ | 1 | 1.6 | ||
Table 1: Types (modalities) of sepsis education or training received.
Tables 2 and 3 define the most important variables for this study, which constitute the perceived problems (P) and educational gaps (G) in Figure 1. Table 2 summarizes the frequency of indicator variables that correspond to the list of common problems associated with sepsis bundle compliance. To elicit responses to common issues identified from the literature, respondents were presented with an initial set of problem classes and were asked to mark all that apply to their perception of perceived difficulties [15,22,27,30,35,38,39]. Simultaneously to broaden the scope of the initial classes, respondents were also asked to add a new class if needed, as well as elaborate on their perception of the problem with their own words. The final description in Table 2 reflects both the initial and respondent-elaborated classes.
| Rank | Class label | Definition of problem class* | Count* | %** |
|---|---|---|---|---|
| 1 | Recognition | p1: Delayed recognition of sepsis | 39 | 63.9 |
| 2 | Symptoms | p2: Delayed presentation of symptoms in sepsis patient, existence of alternative explanation of presenting symptoms, unknown patient information about altered level of consciousness, or lack of patient history | 36 | 59 |
| 3 | Other protocols | p3: Conflict of sepsis bundle with other protocols | 34 | 55.7 |
| 4 | Comorbidity | p4: Comorbidities in sepsis patient | 27 | 44.3 |
| 5 | Patient flows | p5: Unexpected impact on clinical workflows of other acute patients | 26 | 42.6 |
| 6 | Teaming | p6: Inefficient teaming, team communication, or team situation awareness | 23 | 37.7 |
| 7 | Process | p7: Lack of streamlined process to facilitate rapid sepsis management, or specific procedure serves as bottleneck in the process | 19 | 31.1 |
| 8 | Systems | p8: Lack of systems, tools, or aids to support sepsis management | 17 | 27.9 |
| 9 | Recognition only | p9: Only recognized patient condition matters in one’s decision to initiate bundle (no other situational factors are considered) | 17 | 27.9 |
| 10 | Staff workload | p10: Concerns about the increased level of staff workload expected from compliance | 13 | 21.3 |
| 11 | Education | p11: Insufficient level of education or training related to sepsis management | 10 | 16.4 |
| 12 | Culture | p12: Organizational culture related to sepsis management | 10 | 16.4 |
| 13 | Skill fluency | p13: Concerns about the fluency of skills needed when executing the bundle | 10 | 16.4 |
| 14 | Physical environment | p14: Concerns about the physical settings when executing the bundle | 7 | 11.5 |
Note: *Counts the number of respondents that perceived the class to be applicable to their own experiences. The maximum number of counts for each class cannot exceed the total number of respondents; ** The proportion of counts over the total number of respondents. Since multiple responses over the problem classes were permitted, the sum of the percentages over the rows exceeds 100%.
Table 2: Class of perceived problems defined and indicated by respondents.
Table 3 summarizes the respondents’ evaluation of the importance of current gaps in sepsis education and training. That list of current gaps was derived from the failure modes observed during pre-diagnosis, diagnosis, treatment, and post-treatment phases of in-hospital infection control [40].
| Stages | Definition of gaps | (Mean ± SD)* |
|---|---|---|
| Pre-diagnosis/screening | g1: Capturing critical patient information related to sepsis | 7.70 ± 2.46 |
| g2: Initial prioritization over patient severity | 6.98 ± 2.75 | |
| g3: Documenting initial judgment on the patient based on his/ her complaints | 5.63 ± 2.79 | |
| g4: Conducting early screening for sepsis before diagnosis | 6.30 ± 3.01 | |
| Diagnosis/recognition | g5: Administering antibiotics in a timely fashion | 7.54 ± 2.49 |
| g6: Resolving ambiguities associated with sepsis recognition/ diagnostic evaluation | 7.48 ± 2.38 | |
| g7: Reducing delays in seeing the patient | 6.74 ± 2.97 | |
| g8: Handling non-specific evidence to strengthen sepsis recognition/ diagnosis | 7.18 ± 2.56 | |
| Treatment | g9: Reducing delays in drawing blood cultures from septic patient | 6.29 ± 2.92 |
| g10: Handling complications resulting from sepsis treatment | 5.46 ± 3.09 | |
| g11: Appropriate patient monitoring during sepsis treatment | 6.62 ± 2.96 | |
| g12: Capturing critical patient information during sepsis treatment | 6.56 ± 2.82 | |
| g13: Reducing delays in placing orders | 6.52 ± 3.03 | |
| Post-treatment | g14: Follow-up care with sepsis patient after treatment | 6.96 ± 2.65 |
| g15: Post sepsis patient education | 6.88 ± 2.71 |
Note: *The respondents were asked to rate the importance (0-10) for each one of the gaps in Table 3, identified through the entire stages of sepsis management, to address using new education/training.
Table 3: Evaluation of the importance of current gaps in sepsis education/training.
In addition, the respondents’ self-assessed confidence of knowledge (K) for sepsis bundle compliance was quantified in Table 4. Our comprehensive survey scope did not allow us to measure the actual knowledge components in scores. Survey studies on sepsis knowledge, however, support that knowledge scores are weakly or moderately correlated with the level of confidence [28,30].
| Knowledge subsets essential for sepsis bundle compliance | (Mean ± SD)* |
|---|---|
| k1: Definition of sepsis | 3.90 ± 0.768 |
| k2: High-risk patient profiles for sepsis | 3.75 ± 0.907 |
| k3: Screening criteria for Systemic Inflammatory Response Syndrome (SIRS) | 3.80 ± 0.891 |
| k4: Screening criteria for septic shock | 3.87 ± 0.957 |
| k5: Screening criteria for severe sepsis | 3.80 ± 0.910 |
| k6: Sepsis bundle elements | 3.72 ± 0.968 |
Note: *The respondents were asked to assess their perceived level of confidence against the five categories presented (0: Not at all confident- 5: Extremely confident). Those responses were analysed as nominal, rather than categorical, variables.
Table 4: Self-assessment of confidence in the subset of core knowledge for sepsis bundle compliance.
The current section summarized the aggregated responses to a total of 43 survey items where each one of the items was encoded to an appropriate variable type (20 categorical and 23 ordinal/numeric variables). The next section will show the interdependence among those heterogeneous variables, first through the construction of a perceived problem space and mapping of educational gaps onto the space, and then by proving statistical significance of the factors associated with experience, education, and knowledge to the space.
Space construction, mapping, and linear modeling
Singular Value Decomposition (SVD) is the fundamental result of Multiple Correspondence Analysis (MCA) [37]. It substantially reduced the initial 28 dimensions (approximated by the total number of categories spanned by the fourteen variables constituting the problem class in Table 2), down to the two dimensions of Euclidean space, along which each one of the problem classes (P={pj}) was located. For a problem class pi, a pair of “principal” coordinate, i.e., pi=(xj, yj), was obtained using the SVD, such that the weighted sum of squares of the 1st principal coordinates xj‘s (j=1, …, J), is equal to the first principal inertia (0.021), and the weighted sum of squares of the 2nd principal coordinates yj‘s (j=1, …, J) to the second principal inertia (0.004). Since the total inertia for the problem classes (P={pj}) was 0.039, those two principal dimensions were shown to explain approximately 65.5% of the total variability.
Figure 3 depicts the location of the problem classes on the twodimensional space. To help interpret the meaning of the dimensions 1 and 2 based on the problem classes, each problem class was made distinct in terms of shape and color; an “up-pointing” triangle indicates that a problem class was explicitly perceived, whereas a down-pointing triangle indicates the lack of perception of that same problem; “solid-fill” triangles indicate substantial impact on one of the dimensions measured by contribution coordinates (the contribution to the inertia of the respective dimension), whereas unfilled triangles indicate marginal impact; and in addition, the “colors” indicate contribution to the dimension 1 (red), 2 (blue), and none (gray) [37].
Interpreting Figure 3, it can be inferred in Figure 4, that Dimension 1 primarily distinguishes a “unidimensional” focus on only recognizing the criteria for sepsis, versus a broad consideration of “multi-dimensional” resources needed and available to manage sepsis, including staff skills, workload, education, environment, and unexpected impact of sepsis management on other acute patients within current clinical workflow. On the other hand, Dimension 2 appears to distinguish between “system-wide” (e.g., processes and teaming) and “case-specific” (e.g., presentation of septic symptoms and comorbidities in patient) problems.
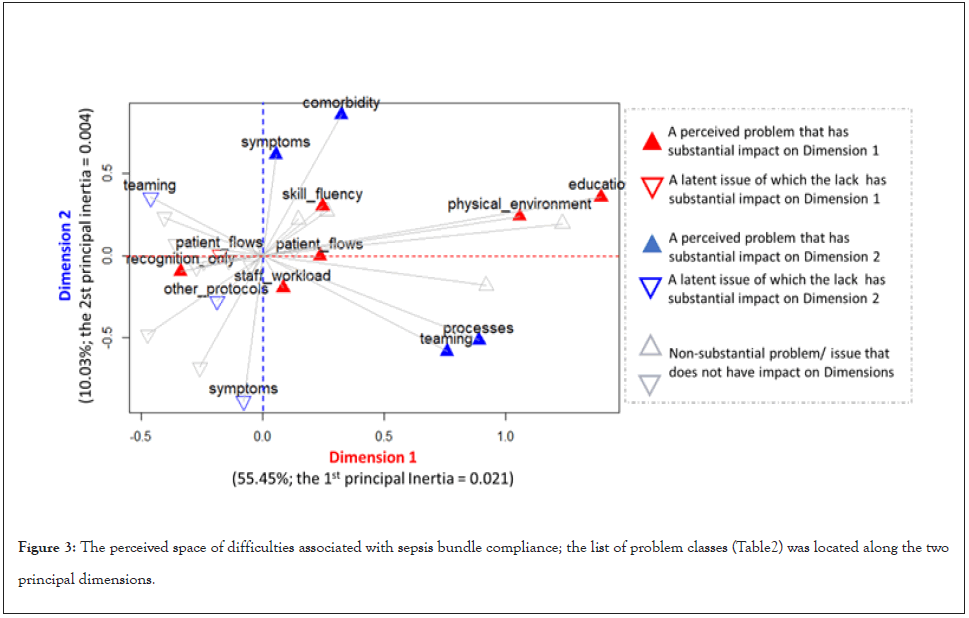
Figure 3: The perceived space of difficulties associated with sepsis bundle compliance; the list of problem classes (Table 2) was located along the two principal dimensions.
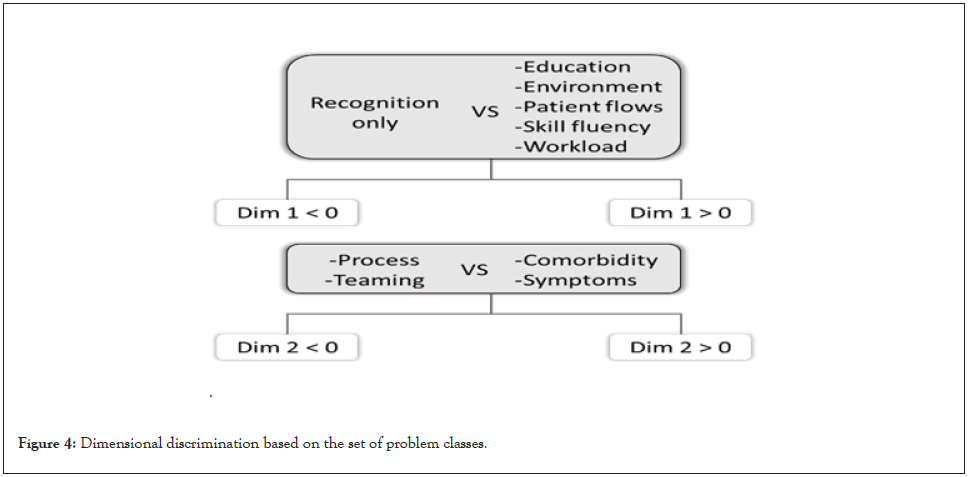
Figure 4: Dimensional discrimination based on the set of problem classes.
The space constructed can be used to interpret semantic (dis) similarities among different problem classes based on their Euclidean distances, which often justifies the combined use of clustering with the MCA [41]. In addition, an input data matrix to the MCA permits the barycentric transition between rows and columns, so that the respondent’s profiles can also be mapped onto the space [42]. The two sets of clusters for distinct problem classes and respondent profiles, respectively, were generated using the hierarchical cluster analysis, and the cluster boundaries were visualized using 85%-confidence ellipses see Figure 5.
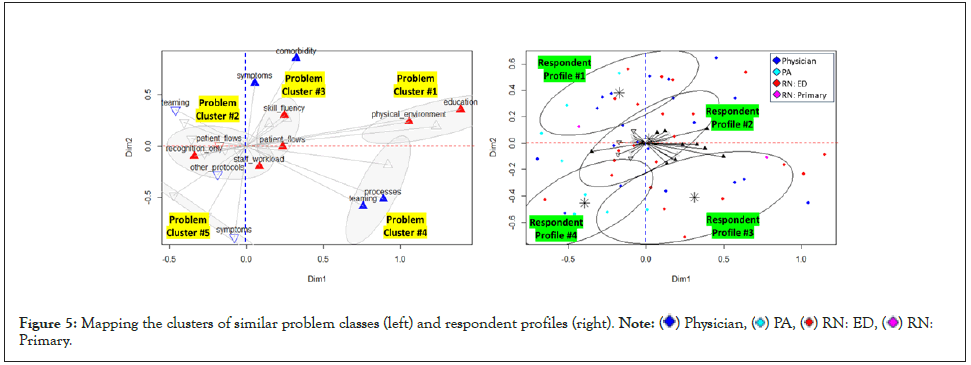
Figure 5: Mapping the clusters of similar problem classes (left) and respondent profiles (right). Note:  Physician,
Physician,  PA,
PA,  RN: ED,
RN: ED,  RN:
Primary.
RN:
Primary.
Another major purpose of the analysis was to map current gaps in sepsis education/training onto the problem space. This mapping would enable us to locate educational gaps in the context of perceived difficulties and thus helps project future educational directions.
Figure 6 depicts the mapping of fifteen gaps defined in Table 3, where the gaps were semantically grouped into those associated with recognition and treatment, respectively. Connecting adjacent gaps for each group in space shows that the gaps associated with recognition tend to span only the positive side of Dimension 1, whereas the gaps associated with treatment tend to span both the positive and the negative sides of Dimension 2.
For any group of gaps, those patterns of horizontal and/or vertical span across the dimensions have implications for their impact on the problem space. Suppose a new training curriculum is targeted at, say, the gap g6, “resolving ambiguities associated with sepsis recognition/diagnostic evaluation”. If the curriculum is successful, it will contribute to improving the related problem of recognition, because the nearest problem class to g6 is “p1: recognition” in Figure 6.
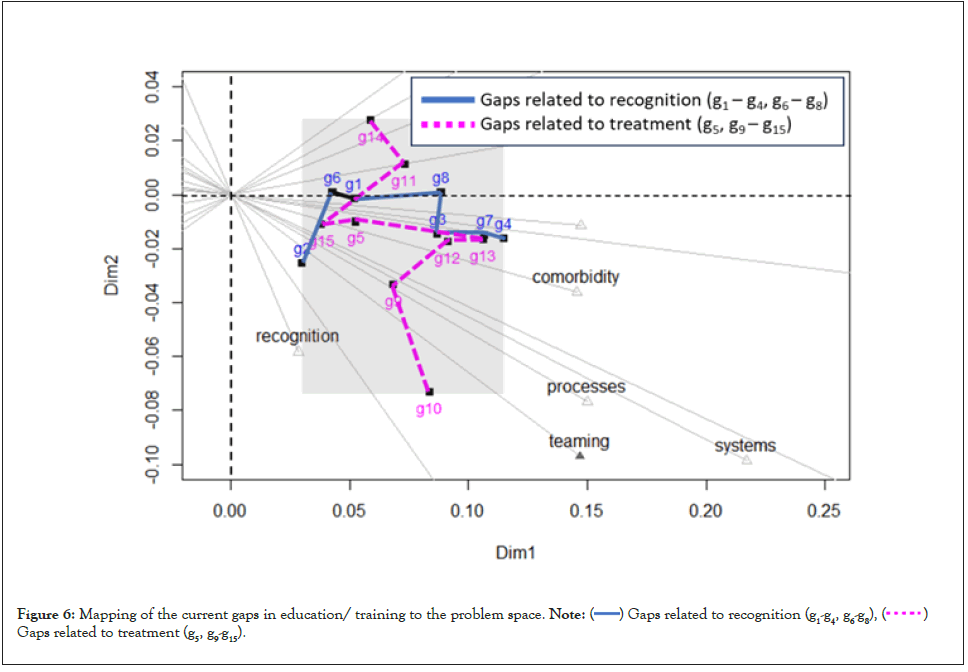
Figure 6: Mapping of the current gaps in education/ training to the problem space. Note:  Gaps related to recognition (g1-g4, g6-g8),
Gaps related to recognition (g1-g4, g6-g8),  Gaps related to treatment (g5, g9-g15).
Gaps related to treatment (g5, g9-g15).
The list of gaps in Table 3 is not exhaustive and new gaps may continue to be discovered, evaluated, and mapped onto the space. For greater impact, a generally desirable direction for education/ training is to tackle certain gaps that tend to span larger areas in the problem space. Examining the shaded region in Figure 6 with respect to the full-scale space in Figure 3, the horizontal and vertical boundaries spanned by the gaps g1-g15 still occupy a small area (x=[0.029, 0.114], y=[-0.073, 0.027]) in the space.
The final analysis intended to check the statistical significance of the factors associated with experience and education, to the perceptions of Problems (P), Gaps (G), and confidence in Knowledge (K). If no factors surveyed are significantly related to the perceptions, even though their perceptual mapping is valid, there would be no practical way to change a location or direction in the perceptual space. Significant factor-perception relationship, on the other hand, could improve explainability of the space and thus help its validation.
Table 5 summarizes a set of statistical tests conducted between the combination of factors and perceptions. Five factors were tested against the null hypothesis that there are no statistically significant differences in perception among any one of the factor levels. Due to the difference in variable types, the perceptions of Problems (P), Gaps (G), and Confidence (K) were tested using different statistical methods. First, the perception of problem (P) was encoded using 14 dichotomous variables defined in Table 2. Conducting the MCA produces the principal coordinates for the rows, as well as for the variables. The row principal coordinates along the dimensions 1 and 2, may represent an aggregated outcome of the perception by individual respondents. Therefore, the perception of problems was tested against each one of the factors using one-way Multivariate Analysis of Variance (MANOVA), where the dependent variables were the principal row coordinates of the first and second dimensions [43]. On the other hand, the perceptions of Gaps (G) and Confidence (K) were encoded using ordinal/numerical variables, and thus One-way Analysis of Variance (ANOVA) was tested against the five factors presented in Table 5.
| Dependent variables | Factor(X) | Experience with sepsis | Terminal degree | Clinical role | An exposure to Simulation-Based Training (SBT) | |
|---|---|---|---|---|---|---|
| Years | Volume | |||||
| Perception of problems: P= {pj} (j=1, …, 14) | Model: {Dim1 (MCA(P)), Dim2 (MCA(P))} ~ X | Pillai’s Trace=0.050, F(10, 110)=0.28, p=0.9837 | Pillai’s Trace=0.158, F(8, 110)1.18, p=0.3176 | Pillai’s Trace=0.182, F(10, 110)=1.10, p= 0.3642 | Pillai’s Trace=0.023, F(2, 56)=0.68, p=0.5079 | Pillai’s Trace=0.019, F(2, 58)=0.56, p=0.571 |
| Perception of gaps: G = {gk} (k=1, …, 15) | Model: {g1; …; g15} ~ X | F=8.36, p<0.001*** | F=7.768, p<0.001*** | F=7.796, p<0.001*** | F=8.107, p=0.00453** | F=9.688, p=0.00193** |
| Perception of confidence in knowledge sets: K = {ks} (s= 1, …, 6) | Model: {k1; …; k6} ~ X | F=18.49, p<0.001*** | F=7.71, p<0.001*** | F=13.27, p<0.001*** | F=28.25, p<0.001*** | F=0.124, p=0.725 |
Note: ***Significant at 0.001; **Significant at 0.01.
Table 5: Summary of tests for the statistical significance of factors on the three different perception datasets.
Sepsis bundle compliance: a matter of cognition or process?
Perception is the first step to Situation Awareness (SA) through the integration of different bits of information from external world, as well as relevant schema retrieved from one own memory [44]. Collective perception is, therefore, foundational for a group of individuals to understand current situations in a coherent manner and refine actions to better respond to new situations. In this regard, a formal representation of perceived difficulties obtained through a dimensional reduction technique can be called a “perceptual space” of a problem, a term originated from neuroscience to represent the structure of neurons in charge of providing information about external world [45].
The construction of perceptual space of sepsis bundle compliance implies the fundamental properties of dimensionality and intrinsic geometry, which allow for metrics to determine perceived distance, similarity, proximity, and match for generalization. As a result, the two dimensions extracted using the SVD (Figure 4) effectively partition the perceptual space into the four distinct quadrants, where (dimension 1, dimension 2)=(+, +) (+, -), (-, +), (-, -). Especially, the partitions (+, -) and (-, +) seem to represent two opposing perspectives on the main barriers to compliance. The former attends to the “process” of multifaceted decision-makings and cooperations among a team of care providers (process-oriented view), and the latter to predominantly clinical “judgment” given patient symptoms and severity of conditions (cognition-oriented view).
Both perspectives appear to gain support from the literature. Starting with a different perceptual view, however, solutions differ widely. Studies in favor of the process-oriented view do not necessarily take light of recognition, but tend to seek solutions from systems design, analysis, and improvement, such as introducing advanced information systems, process optimizations, and teambased interventions [15,17,18,46-50]. Cognition-oriented views, to the contrary, pursue solutions to enhance the recognitionprimed decision-making through enhanced experiences (e.g., an exposure to diverse care contexts and dynamic patient conditions, by familiarizing with relevant visual cues on sepsis patient and care settings and through improved reasoning skills to connect disjoint information pieces for sepsis recognition/diagnosis [51-59].
Further on the process versus cognition-orientation, the relative proportion of physicians and nurses appears to vary by each quadrant in the perceptual space, as observed from the mapping of care providers onto the space; see the right panel in Figure 5. The process-oriented quadrant tends to be associated with a higher proportion of nurses over physicians (9 over 6), whereas the cognition-oriented quadrant has more physicians over nurses (8 over 4). Although those small numbers do not permit a conclusion, this difference in proportion by clinical role may be attributed in part to the different nature of clinical reasonings assumed by physicians and nurses respectively, i.e., hypothetico-deductive reasoning aimed at correctly identifying a septic patient versus epistemological process of finding what will “get it progressively less wrong” throughout the compliance process [60-62]. A further investigation is needed to identify factors, besides clinical role, that predispose one to a certain orientation on the perceptual space.
Using perceptual space to guide best practice and learning
In general, dimensional representation of perception has been a favored approach in psychology and educational research (for example, the keywords search in September 2023 for “perception” and “correspondence analysis” in the Web of Science returned 1,589 publications, among which psychological research accounted for 20%). If the proposed space offers a generalized representation of collective perception associated with sepsis management, the next step would be using the perceptual space to guide design, implementation, and improvement of best practices and learning tools for enhanced compliance.
Current best practice and education of sepsis bundle compliance are guided by a set of “all-or-nothing” requirements, i.e., SEP-1 measures [9]. To demonstrate compliance, all intervention requirements must be satisfied, and resistance against this protocolized care has raised several concerns [63]. For example, forcing a quick administration of antibiotics following the bundle could pose the risks of premature diagnostic closure, overclassification of patients as infected, and overuse of antibiotics to patients who do not benefit from them [64]. Furthermore, concerns over the culture of “treat first, ask questions later” as an unexpected result of compliance or frustrations due to the lack of teamwork and leadership needed to implement compliance persist [63,65]. The above risks and concerns cannot be properly addressed using the SEP-1 measures alone, because the SEP-1 counts actions, not the perceptions and reasoning behind those actions.
In this regard, the perceptual space for sepsis can possibly complement the SEP-1, thanks to its ability to trace any changes in the perceptions of cognition, process, protocols, patient, workload, environment, and culture, both for an individual or team of care providers. This ability will enable us to trace short and long-term effects of a particular practice or education strategy with respect to the multi-dimensional problem clusters (the example clusters in the left panel of Figure 5), and thus will help select best strategies leading to a desirable direction of changes.
Mathematically, the space constructed using SVD has a property of transition between the row and column profiles. The column principal coordinates G in Equation (3) is related to the row principal coordinates F through the equation (5):
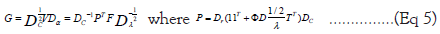
In our data matrix (Figure 1), the perceived difficulties were encoded using a 61-by-14 matrix for input to Multiple Correspondence Analysis (MCA), in which the 14 columns represented a set of problems perceived in a collective manner, and the 61 rows represented individual differences in terms of the subjective weights given to the problem set. Here, two scenarios can be assumed for tracing changes in the data matrix. In one scenario, suppose a new type of problem emerges due to the introduction of new practice in a clinical unit. This emerging problem class will be added to the 15th column in the data matrix. Using the transition property, this supplementary column can be converted to a new row in the row principal coordinates. The transition property thus enables us to map additional column(s) to the previously constructed space without the need to recalculate all other coordinates. In the other scenario, suppose a person received a new sepsis education and we may want to trace the effects of learning gain on the space. In this case, the individual’s change in perceptions will be represented using a new row-profile having an altered vector of weights, stacked below the data matrix as the 62nd row. Similar to the supplementary column(s), additional rows can be mapped to the space without impacting the coordinates of other row profiles. Those techniques are detailed in supplementary and subset correspondence analysis [37].
Limitations and future works
Revisiting the summary of statistical significance in Table 5, a care provider’s clinical experience with sepsis, level of medical education, and clinical role had significant relationships with his/her own perceptions of gaps and confidence, respectively. Additionally, one’s previous exposure to Simulation-Based Training (SBT) was significantly related to their perception of gaps. Those outcomes are in line with the literature on the sepsis-related perception of care providers [28,30]. To the contrary, an individual’s location on the perceptual space was not significantly related to these factors of experience, education, and training.
This distinction can be partly explained by the violations of equal variance assumption found in several models tested significant (including the models for G={gk}: {gk}~ Xexperience_in_years; {gk}~ Xexperience_in_volume, {gk}~ Xterminal_degree; {gk}~ Xclinical_role; and the model for K={ks}: {ks}~ Xterminal_degree). Levene’s test on those models revealed significant deviations from equal-variance assumption at a 1%-significance level (F=11.813, p<0.001; F=3.4653, p=0.008149; F=9.447, p<0.001; F=14.06, p<0.001; and F=3.1055, p=0.009288, in the order of the models listed) [66].
The finding that the locations of row profiles in the perceptual space is not related to the factors of experience, education, and training can be considered positive evidence testifying for the robustness of the dimensions and space structure, but further investigation is needed to identify related factors that can possibly change the locations of row profiles.
To unveil the complexity behind the actions of bundle compliance or non-compliance in clinical practice, this article aimed to understand frontline care providers’ perceptions at an acute care hospital in the Midwest. In general, perception is a precursor to situation awareness and action. In difficult sepsis cases, particularly, the quality of perception can help quickly identify relevant cues from the patient, seek appropriate information from the care environment, and determine the best course of actions to achieve plausible goals with bundle compliance. Beyond an individual level, a collection of perceptions from a group can help generalize on the structure and relationship among its constituent elements. This study conducted a survey to 68 clinicians at emergency department regarding their perceived difficulties, educational gaps, and confidence with sepsis knowledge. The fundamental mathematics of Singular Value Decomposition (SVD) was applied for Multidimensional Correspondence Analysis (MCA) to build a perceptual space of collective perceptions surrounding early management of sepsis.
As a result, two principal dimensions were identified for the perceptual space. The first dimension distinguished “all-ornothing” versus multifaceted, analytical perspective in compliance, and the second dimension appeared to split between system-wide versus case-specific foci in sepsis interventions. Both dimensions could explain 65.5% of the total variability. Then, the respondents’ perceptions of educational gaps were mapped onto the perceptual space, and the mapping occupied only a small area within the space, advocating new educational strategies targeted at comprehensive foci. Finally, statistical tests confirmed that clinicians’ experience with sepsis, level of medical education, and clinical role had significant relationships with the perception of educational gap. To the contrary, an individual’s location on the perceptual space was not significantly related to these factors of experience, education, and training. A systematic investigation is needed to identify factors that shift an individual’s location on the perceptual space.
In conclusion, the proposed perceptual space for sepsis has potential to complement in a prospective fashion, the current quality measure of sepsis compliance (SEP-1) which is retrospective and focuses on outcomes. For example, this novel representation method enables us to trace changes in the perceptions related to cognition, process, protocols, patient, workload, environment, and culture, both for an individual or team of care providers. This traceability will help assess the effects of a new compliance strategy with respect to the multi-dimensional problem clusters, and thus select the best one that leads to a desirable direction of changes.
Citation: Cohen M, Kim I, Rehg J, Hawknuff C, Brown C, Jamison S, et al. (2023) Understanding Sepsis Bundle Compliance Perceptions using Dimensional Representation of Survey Responses from Frontline Care Providers, Intern Med. 13:426.
Received: 14-Sep-2023, Manuscript No. IME-23-26951; Editor assigned: 18-Sep-2023, Pre QC No. IME-23-26951 (PQ); Reviewed: 02-Oct-2023, QC No. IME-23-26951; Revised: 09-Oct-2023, Manuscript No. IME-23-26951 (R); Published: 16-Oct-2023 , DOI: 10.35248/2165-8048.23.13.426
Copyright: © 2023 Cohen M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.