Endocrinology & Metabolic Syndrome
Open Access
ISSN: 2161-1017
ISSN: 2161-1017
Case Report - (2020)Volume 9, Issue 6
Tumour-induced osteomalacia (TIO), also known as oncogenic osteomalacia is a rare paraneoplastic syndrome characterized by severe persistent hypophosphatemia. It occurs due to excess production of phosphatonins, which clinically manifests as severe hypophosphatemia. In our case, a 37-year-old woman presenting with multiple joint pains for last 9 years, progressive weakness of bilateral lower limbs for the last 1 year and past history of long bone fractures was diagnosed with tumor-induced osteomalacia (TIO) although she had normal FGF23 levels. TIO was caused by phosphaturic mesenchymal tumour in right tibia. After surgical resection of the tumour, her symptoms resolved. This is a unique case in that the patient had a normal systemic FGF23 level even with severe manifestations of TIO and also patient had raised parathyroid hormone levels which create a confusion of parathyroid related hypophosphatemia rather than the TIO. So a strong clinical suspicion is needed to diagnose TIO in such atypical cases.
Tumour induced osteomalacia; Fibroblast growth factor 23; Phosphatonins; Hypophosphatemia
Tumour induced osteomalacia (TIO) is a rare paraneoplastic manifestation, commonly due to phosphaturic mesenchymal tumours. These tumours produce phosphatonins, commonly FGF23 (Fibroblast growth factor 23). FGF23 causes impaired tubular reabsorption of phosphate and impaired 1-α hydroxylation of 25- hydroxy vitamin D. this manifests as severe hypophosphatemia. The clinical symptoms of TIO are due to severe hypophosphatemia, which manifests as bone pains, recurrent fractures and other musculoskeletal symptoms. Due to these nonspecific complaints, they are often misdiagnosed as with various musculoskeletal ailments, rheumatological diseases and sometimes even psychiatric disorders. In any patient with history of bone pains, recurrent fractures and investigations revealing severe hypophosphatemia with renal phosphate wasting, TIO should be kept as strong possibility. The median age of presentation is third to fourth decade. In majority of TIO patients FGF23 levels were increased but remember, normal FGF23 levels does not rule out TIO. Once there is a strong suspicion of TIO, next step is functional imaging to look for lesions. Once the lesions are found, anatomical imaging is done for better localization and characteristics. If no lesion found or multiple lesions found, venous sampling should be done to localize the tumour. Treatment includes surgical excision for surgically resectable lesions. If unresectable lesion, radiofrequency ablation was used successfully. If lesion not identified by imaging and in some surgically unresectable lesions, medical therapy was given. Medical therapy includes phosphorus replacement and calcitriol or alphacalcidiol supplements.
A 37 year old female presented to the endocrinology outpatient department with a progressive weakness in bilateral lower limb for last 1 year and a significant past history. In 2012, she started having pain in bilateral hip joints, pain present while getting up from sitting posture and while walking. These symptoms gradually increased over the next 3 years and she was evaluated multiple times at private hospital and was given calcium supplements. In 2015, she was evaluated at private hospital and found to have bilateral fracture neck of femur (Figure 1). ORIF (open reduction and internal fixation) was done, after which her symptoms improved for next 3 years. In 2018, she got slipped on snow and sustained left fibular fracture (Figure 2). Managed with total contact casting and she improved symptomatically. In April 2019, she was evaluated at another hospital where she was found to have Hypophosphatemia and was evaluated for the same but no lesion was localised.
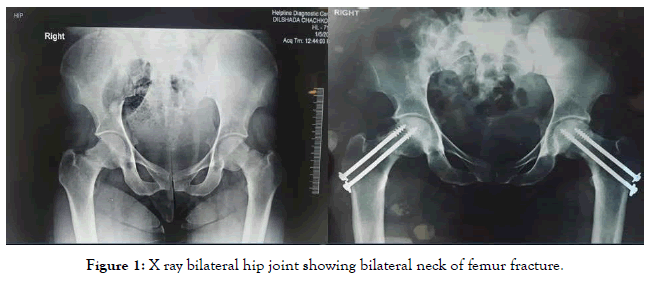
Figure 1. X ray bilateral hip joint showing bilateral neck of femur fracture.
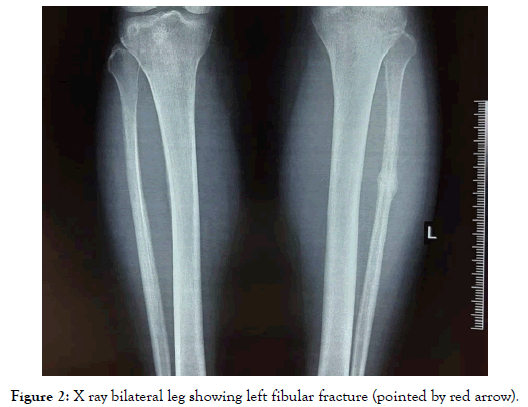
Figure 2. X ray bilateral leg showing left fibular fracture (pointed by red arrow).
Now she presented with chief complaints of multiple joint pains for 9 years and Progressive weakness in bilateral lower limb for 1 year. No sensory disturbances, no bladder and bowel disturbances. No family h/o similar illness (bone d/s). His vitals were stable. General examination was normal. Power 3/5 in hip extensors & flexors, rest of the systemic examination was normal. At admission, Her blood investigations showed hypophosphatemia- serum phosphorus 1.53 mg/dl (normal range 2.5-4.0 mg/dl) with normal serum calcium, normal 25 hydroxy vitamin D, raised parathyroid hormone 145 pg/ml (normal range 15-65 pg/ml) and raised alkaline phosphatase 148 U/L (normal range 42-128 U/L). The blood pH was normal (no acidosis) and Serum Creatinine 0.5mg/dl. Twenty four hour urinary Protein was 136 mg, 24 hour urine Creatinine was 719 mg, 24 hour urine phosphorus 339 mg, 24 hour urine calcium 49 mg. Calculated Fractional Tubular resorption of phosphate (TRP) (TRP=1- fractional excretion of phosphate) 0.87 and The ratio of the renal tubular maximum resorption rate of phosphate to the glomerular filtration rate (TmP/GFR) 1.31 mmol/L. C terminal FGF 23 was normal 141(0-150 RU/ml).
Investigations revealed hypophosphatemic osteomalacia and reduced tubular resorption of phosphate but FGF 23 was normal. Initially neck ultrasound was done to look for parathyroid, which was normal. Although FGF 23 was normal, in view of strong suspicion of tumour induced osteomalacia (TIO), DOTA PET scan was done, which showed somatostatin receptor expressing lesion in right tibia upper part with pseudo-fractures at multiple sites (Figure 3). While waiting for surgical excision, she was managed with oral phosphate. Anatomical imaging MRI knee done showed well defined subcortical area of altered signal intensity in right tibia above tibial tuberosity (Figure 4). She underwent gamma camera guided En bloc right proximal tibia osteolytic lesion excisional biopsy on 14/11/19. HPE analysis showed features of mixed connective tissue variant of phosphaturic mesenchymal tumour. Post-operative x ray showed complete removal of the lesion (Figure 5). On follow-up, serum phosphorus levels returned to normal level. Laboratory values of pre-operative and post-operative were discussed in Table 1. Patient is doing well without any symptoms (Table 2).
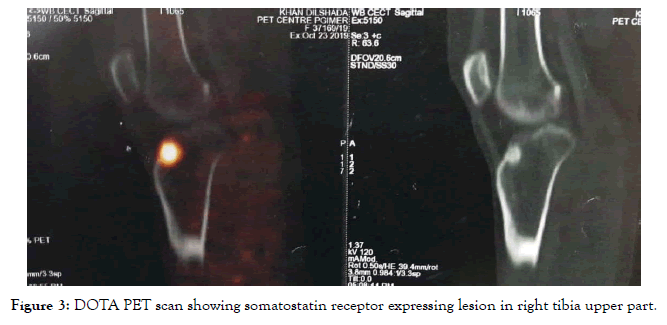
Figure 3. DOTA PET scan showing somatostatin receptor expressing lesion in right tibia upper part.
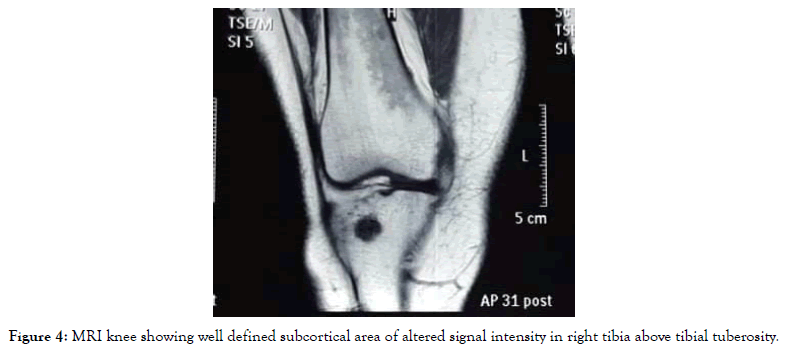
Figure 4. MRI knee showing well defined subcortical area of altered signal intensity in right tibia above tibial tuberosity.
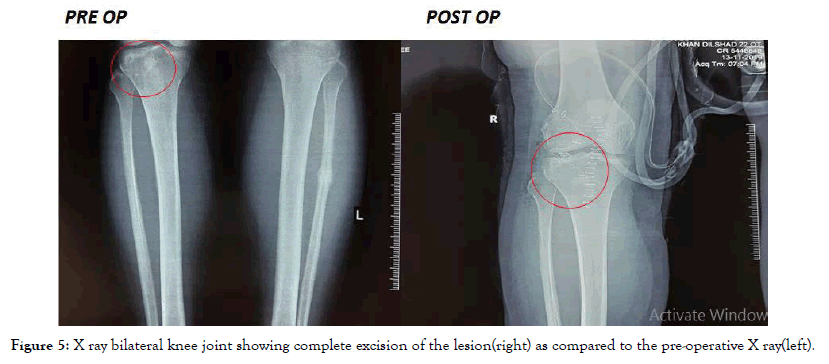
Figure 5. X ray bilateral knee joint showing complete excision of the lesion(right) as compared to the pre-operative X ray(left).
| PREOP | POSTOP | NORMAL REFERENCE | |
|---|---|---|---|
| Serum calcium | 8.6 | 8.54 | 8.5-10.3 mg/dl |
| Serum phosphorus | 0.99 | 2.44 | 2.5-4.0 mg/dl |
| ALP | 148 | 146 | 42-128 U/L |
| Albumin | 4.4 | 4.27 | 3.4-4.8 g/dl |
| 25 hydroxy vitamin D | 39 | 35.29 | 11-43 ng/ml |
| iPTH | 100.7 | 62.43 | 15-65 pg/ml |
| %TRP | 80 | 85-95% | |
| TmPGFR | 1.12 | 2.2-3.6 mg/dl |
Table 1: Blood investigations–original.
| BMD(Bone mineral density) | T score | Z score | |
|---|---|---|---|
| L1-L4 lumbar vertebrae | 0.909 | -1.3 | -0.3 |
| Neck of femur | 0.874 | -1.1 | -0.3 |
| Radius+ ulna distal one third | 0.882 | -1.3 | -0.4 |
Table 2: Dexa scan.
Tumour Induced Osteomalacia (TIO), Also known as oncogenic osteomalacia was first described in 1947 by Robert McCance [1]. It’s a rare paraneoplastic syndrome commonly caused by mixed connective tissue variant of Phosphaturic Mesenchymal Tumours (PMT). TIO occurs due to phosphatonins which include FGF-23, FGF-7, secreted frizzled-related protein 4 (SFRP 4) and Matrix Extracellular Phosphoglycoprotein (MEPE) [1]. These phosphatonins are secreted commonly by PMT, which result in a rare manifestation known as TIO. The other tumours like Sino nasal hemangiopericytomas, osteosarcomas, and fibromas also present as TIO [1]. Most of the tumours causing TIO are benign, although malignant disease also can cause it [2]. Patient commonly develops symptoms not due to tumour itself rather due to consequences of severe hypophosphatemia. Thus, owing to nonspecific complaints, they are often misdiagnosed as with various musculoskeletal ailments, rheumatological diseases and sometimes even psychiatric disorders. Laboratory findings commonly seen are given in the Table 3.
| Typical TIO presentation | Our case presentation | |
|---|---|---|
| Serum calcium | Normal | Normal |
| Parathyroid hormone | Normal | Increased |
| 25 hydroxy vitamin D | Normal | Normal |
| Alkaline phosphatase | Increased | Increased |
| 24 hour urinary calcium | Normal | Normal |
| FGF23 | High | Normal |
| TRP | Low | Normal |
| TmPGFR | Low | Low |
| Median age of presentation | 3rd to 4th decade | 4th decade |
Table 3: Difference in our case presentation as compared to typical TIO presentation.
Majority of TIO patients have increased levels of FGF23 but still normal FGF23 does not rule out TIO. Till now there is only one case report in literature of TIO patients with normal FGF23 levels. Amblee A et al. [3] presented a case report in 2014, where a giant cell tumour in right foot resulted in severe TIO but with normal FGF23 levels, low vitamin D and normal PTH levels. Our case has similar presentation of TIO with normal FGF23 levels, but the difference lies in the fact that our case had raised PTH and normal vitamin D levels. The difference between our case presentations is shown in the Table 4.
| Amblee A et al case presentation | Our case presentation | |
|---|---|---|
| FGF 23 levels | Normal | Normal |
| Vitamin D | Low | Normal |
| PTH | Normal | Raised |
| Serum Calcium | Normal | Normal |
| Serum phosphorus | Low | Low |
Table 4: Difference in presentation of cases between amblee a et al case report and our case report.
Pal R et al. [4] conducted a retrospective analysis of 30 patients of TIO diagnosed at three tertiary care hospitals in India. In this retrospective analysis they found two TIO patients had inappropriately normal FGF23 levels and they came to a conclusion that TIO patients can have elevated or even inappropriately normal FGF23 levels. They highlighted the fact that after surgery, percentage decline in FGF23 rather than the absolute value correlates with disease cure.
Once we have a strong suspicion of TIO or diagnosis of TIO is made, then next step is to localize the lesion by functional imaging followed by anatomical imaging. Functional imaging includes FDG-PET/CT scan which is most sensitive and 68Ga DOTATATE PET/CT scan which is most specific for localizing lesions in TIO [5]. Once lesions found by functional imaging, anatomical imaging is done for better localization and characteristics. Anatomical imaging includes x ray, CT scan and MRI scan. If single lesion identified, then surgical resection should be done. If multiple lesions found, selective venous sampling with measurements of FGF23 levels done. The side with higher FGF23 levels was localized and resected. If no lesion found or if multiple lesions found, do whole body venous sampling with assessment of average values from different anatomical regions [6]. The algorithm for localizing the lesion is given below.
Treatment of TIO is always localizing the lesion followed by surgical resection. But if lesion is not localized or unresectable, then medical management to be followed. Medical treatment includes phosphorus and vitamin D supplements. Recently trials are been done on anti FGF23 human monoclonal antibody Burosumab (also known as KRN23) [7].
Prognosis of TIO depends upon percentage decline in FGF23 after surgery, rather than the absolute value. The mean percentage decline in FGF23 that was associated with clinical and biochemical cure was 81.1% (range 27.5%–99.2%). After surgical excision, local recurrence of less than 5% was documented in literature.
In a retrospective analysis by Pal R et al. [4], serum phosphorus never returned to normal values in 18.2% of patients
Thus any patient presenting with persistent hypophosphatemia, normal calcium levels, raised alkaline phosphatase, and raised or inappropriately normal FGF23 levels, strong suspicion of TIO should be kept. From this case report, it is clear that although majority of TIO patients have increased levels of FGF23 but still normal FGF23 does not rule out TIO. Also this case is unique in that the parathyroid levels were raised which creates a confusion in diagnosing TIO. So a strong clinical suspicion is needed to diagnose TIO.
Citation: Chinnadurai KK, Jayachandran A (2020) Tumour Induced Osteomalacia–Unique Presentation. Endocrinol Metab Syndr 2020; 9:317. doi: 10.35248/2161-1017.20.9.317
Received: 08-Aug-2020 Accepted: 10-Sep-2020 Published: 17-Sep-2020 , DOI: 10.35248/2161-1017.20.9.317
Copyright: © 2020 Chinnadurai KK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : None