
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Case Report - (2021)
Background: Dengue has been emerging as rapidly spreading and dreaded mosquito borne disease caused by the bite of Aedes Aegypti Mosquito. Clinical features are variable and presents with Dengue fever or Dengue Hemorrhagic fever or more severe Dengue shock syndrome. Thrombocytopenia is presenting feature in in all Dengue cases and some often presents with bleeding. Platelet transfusions are given in patients with haemorrhagic symptoms.
Present study thus aims to study the effectiveness of platelet transfusion in management of Dengue patients with Dengue haemorrhagic fever and Dengue shock syndrome.
Results: In present study, a total of 20 patients were diagnosed as dengue confirmed cases by serological testing methods. Out of 20, 12 (60%) patients had dengue fever with platelet count in range of 50,000-80,000 per μl. Two patients with Dengue fever had Petechial spots with platelet count in range of 50,000 per μl and were given prophylactic Single Donor Platelet Transfusions. Eight patients (40%) presented with Dengue Haemorrhagic fever and platelet count of < 20,000 per μl. These patients were given single donor platelet transfusions. Six patients responded good with CCI of > 30,000 per μl and 2 patients recorded as non-responders.
Conclusion: This study suggests that 25% Platelet transfusions are inappropriate. Platelet transfusions are more effective when it is given to patients with platelet count <20,000 per μl. Platelet transfusion should be given based on platelet count and hemorrhagic manifestations, as this decreases hospitalization of patients and complications of dengue.
Dengue; Thrombocytopenia; Platelet
Dengue is the most rapidly spreading mosquito borne viral disease in world and an estimated 50 million dengue infections occur annually [1]. The south East Asian countries like India, Indonesia, Myanmar and Thailand are at highest risk of Dengue Fever/Dengue Haemorrhagic Fever. Dengue is viral disease caused by dengue virus with four serotypes DEN-1 to DEN-4 of flavivirus family transmitted through Aedes Aegypti mosquito [2]. Clinical features of DF are characterized by an abrupt onset of fever associated with headache and retroorbital pain, myalgia, vomiting and weakness. Minor hemorrhagic manifestations signs like petechiae may be observed in some patients. DF is self- limiting disease and most patients recover without complications approximately 10 days after the onset of illness. However, some patients develop severe manifestations such as increased vascular permeability and plasma leakage that lead to death [3]. Bleeding, one of the dreaded complications of Dengue is associated with higher mortality in dengue hemorrhagic fever and Dengue shock syndrome [4]. Platelet transfusions are indicated in patients who are showing bleeding symptoms or other haemorrhagic symptoms with thrombocytopenia [5].
The present study thus aims to study the effectiveness of platelet transfusions in management of dengue patients with Dengue haemorrhagic fever and Dengue shock syndromes and their treatment outcome [6,7]. All dengue seropositive cases admitted and treated in the hospital in Department of Medicine were included in study from 1st September 2017 to 30 November 2019.
This was a retrospective study conducted at Dhiraj Hospital affiliated with SBKSMIRC, Vadodara, on adult patients with dengue fever confirmed positive by dengue serological Rapid test kits. All laboratory investigations and clinical findings were recorded from the time of admission to the time of discharge. The age of patient, duration of fever before admission, result of dengue serological test, hematocrit, platelet count on admission during hospitalization, Presence of haemorrhagic manifestation like petechiae, hematemesis, melena, gum bleeding were recorded. The cases were diagnosed and categorized as per WHO criteria into 1) Dengue fever 2) Dengue Hemorrhagic fever and 3) Dengue shock syndrome based on severity of disease, bleeding manifestations, hematocrit and thrombocytopenia. All these patients were given ABO matched Single Donor Platelets. DGHS guidelines for indication, dose and monitoring of response for platelet transfusion were followed. Patients with post transfusion platelet increment >=10,000 per μl and corrected count increment (CCI) >= 5000 μl, one hour post transfusion were considered responders. Primary outcome was platelet count increment at 24 and 72 hours. Patients having platelet count >20,000 per μl. in the absence of bleeding manifestations were considered to have received inappropriate platelet transfusions. A value of more than 1.5 times the control for PT and APTT were considered abnormal for the assessment of coagulopathy in Table 1.
| Platelet count/cu mm | ≤ 10 | Nov-20 | 21-30 | 31-40 |
|---|---|---|---|---|
| Number of patients with hematemesis | 0 | 1 | 0 | 0 |
| Number of patients with malena | 0 | 1 | 0 | 0 |
| Number of patients who received platelet transfusions | 6 | 2 | 0 | 1 |
Table 1: Dengue Patients with thrombocytopenia and bleeding who received platelet transfusion.
In the present study, 20 Patients were reported as serologically confirmed dengue cases with 12/20 (60%) presented with clinical features of Dengue fever and 8/20 (40%) presented with clinical features of Dengue hemorrhagic fever (Figure 1). The age range of positive patients was 18-35 years, with Male to Female ratio of 2:1. Out of 20 (12) patients presented with Dengue fever and there Platelet count was in range of 50,000-80,000 per μl. Two patients with Dengue fever and Platelet count in range of 50,000 per μl were given platelet transfusion. Out of 20 (8) patients presented with symptoms of DHF and were in platelet count range of <20,000 per μl. These 8 patients with count of <20,000 per μl were transfused with single donor platelets and Post transfusion increment was seen in 6 out of 8 patients. The CCI (corrected count increment) and Platelet percentage recovery was calculated on first two consecutive transfusions. Only 2 cases reported with bleeding manifestations where the increment was <30,000 per μl after each unit of transfusion. The number of platelet in each unit ranged from 3 × 1011 Platelets in Single Donor Platelet concentrates method (Tables 2 and 3).
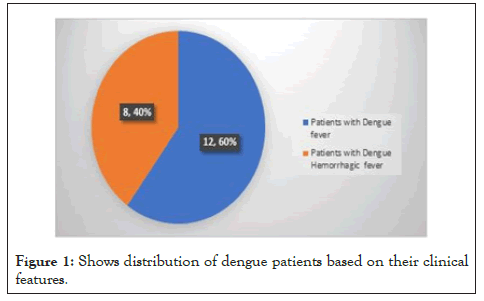
Figure 1: Shows distribution of dengue patients based on their clinical features.
| Disease (n=) | CCI (mean value) After first unit | After second unit | Percent platelet recovery. After first unit | After second unit (%) |
|---|---|---|---|---|
| Dengue =20 | 18000 | 19000 | 52 | 55.2 |
| Dengue with bleeding=2 | 4000 | 4000 | 10 | 10 |
Table 2: Distribution of corrected count increment and platelet percentage recovery.
| Diagnosis | Responders | Non responders | Total |
|---|---|---|---|
| Dengue | 6 (75%) | 2 (25%) | 8 (100%) |
Table 3: Response to platelet transfusions.
In India, Dengue epidemics occur after every 2 to 3 years and they are a major health concern. The diagnosis is largely on clinical suspicion supported by Laboratory evidence of recent infection in the form of IgM antibodies against the virus.
In present study, Dengue infection including Dengue fever was reported in 12/20 (60%) cases and Dengue Haemorrhagic fever, was reported in 2/20 (10%) cases. Fever was accompanied with skin rash and haemorrhagic manifestations in DHF. Similar presentations were reported in studies done by Narayan et al. and Lum et al. [8,9] Thrombocytopenia in dengue fever is often associated with complications and morbidities [10]. The etiology of thrombocytopenia in Dengue infection can be due to
1. Bone marrow suppression
2. Destruction of megakaryocytes
3. Formation of antiplatelet antibodies
The DHS guidelines stipulate that platelet transfusions should be given to patients with platelet count <20,000 per cumm [3]. In present study 60% Patients had a platelet count greater than 20,000 per cumm, 10% had hemorrhagic manifestations like petechiae, gum bleeding, epistaxis etc. that necessitated the use of platelet transfusions? Inappropriate platelet transfusions received in present study was 5%. In a similar study by Makroo RN, et al, inappropriate platelet transfusions received was 13.77%.
In Present study about six patients responded well to platelet transfusions and only 2 patients were non responders to platelet transfusions where platelet increment was observed less than 30,000 per cumm after 24 hours of Single donor platelet post transfusion.
The various reasons for non-responders can be
1) Immune causes
*Alloantibodies directed against platelet alloantigens, ABO antigen or HLA class I antigen. (induced by pregnancy or transfusion).
*Auto antibodies e.g (ITP).
2) Non immune causes like Active bleeding, fever, sepsis, splenomegaly, DIC [2].
This study suggests that 25% Platelet transfusions are inappropriate. Platelet transfusions are more effective when it is given to patients with platelet count <20,000 per μl. Platelet transfusion should be given based on platelet count and hemorrhagic manifestations, as this decreases hospitalization of patients and complications of dengue.
Citation: Dogra A, Rana K, Gosai D (2021) To Study the Effectiveness of Platelet Transfusion in Management of Dengue Patients in Tertiary Care Hospital. J Clin Toxicol. S16:003.
Received: 08-Mar-2021 Accepted: 22-Mar-2021 Published: 29-Mar-2021 , DOI: 10.35248/2161-0495.21.s16.003
Copyright: © 2021 Dogra A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.