Journal of Thyroid Disorders & Therapy
Open Access
ISSN: 2167-7948
ISSN: 2167-7948
Research Article - (2020)Volume 9, Issue 1
Introduction: In the older times of thyroid surgery, the operations were performed under local anaesthesia. With the
development of anaesthesia surgeons preferred to use narcosis for most thyroid surgeries. Today, however, regional
anaesthesia has become popular as a safe and effective technique based on numerous clinical studies, surgeons are
still keen on doing surgeries under general anaesthesia. Regional anaesthesia is indicated in high risk patients and
also in case of pregnancy, but in well-fit patients it could lead to faster recovery. In case of a substernal goitre or
infiltrating carcinoma or in case of severe bleeding disables general anaesthesia should be chosen.
Patient materials and methods: At the Department of Multidisciplinary Head and Neck Cancer Center in the
National Institute of Oncology between May 2019 and March 2020, 9 patients underwent thyroid or parathyroid
operations in regional anaesthesia: 7 patients had lobectomy, 1 patient had thyroidectomy, and 1 patient had
parathyroid adenoma removal. In all cases, the regional anaesthesia involved the blockage of the superficial branches
of the cervical plexus, followed by an ultrasound guided thyroid capsule sheath space block. Patients were previously
given 2 mg of i.v. midazolam, and in case of need 50 ug of i.v. fentanyl under haemodynamic monitoring.
Results: One patient had a transient Horner’s syndrome. The average time of the surgery was 42.7 minutes (25-80
minutes). All patients tolerated the procedures very well. The incidence of postoperative pain, such as nausea and
vomiting were reduced. Patients could be discharged earlier and they had a faster recovery.
Conclusion: Based on our limited experience, regional nerve block anaesthesia for uncomplicated thyroid and
parathyroid patients offers several advantages, and provides superior postoperative nausea, and pain control.
Thyroid surgery; Regional anesthesia; Thyroiditis; Thyroid gland
General anaesthesia of thyroid surgery reaches back to 1849, when Pirogoff, a surgeon from Saint Petersburg operated on a 17-year-old young lady with multi-nodular goitre in ether narcosis [1]. Until the 1900s thyroid operations were carried out in general anaesthesia, until Kocher ’ s patient died from Chloroform on the operating table, and most of the postoperative complications were caused by the side-effect of the narcotics [2]. In later days thyroid procedures were operated mostly in local anaesthesia used cocain. Dunhill has performed life-saving interventions under local anaesthesia on patients who could not be anaesthetised and other giants of thyroid surgery have also operated in local anaesthesia [3,4]. Since general anaesthesia has become a safe procedure, surgeries under local and regional anaesthesia have become less common. However, in the last decades, multiple international thyroid gland centres have re-introduced procedures performed under regional anaesthesia, significantly reducing both the length and the costs of hospitalisation [5-7]. No differences have been found between the postoperative results of patients operated under general and regional anaesthesia in a randomised study. Regional anaesthesia requiring shorter hospitalisation and reduced costs has been found to be as safe as general anaesthesia [8]. In 1925, Felix Mandel performed the first parathyroid gland removal under local anaesthesia [2]. Since that time, several thyroid gland centres still prefer regional anaesthesia to general anaesthesia, because it is more cost-efficient, involves fewer postoperative complications and patients do not experience queasiness and nausea in the postoperative period [9]. Additionally, regional anaesthesia may be preferable if the risk of general anaesthesia is high due to the patient’s comorbidities or in case of pregnancy to prevent the exposure of the foetus to high doses of narcotics [10]. Contraindications include allergic reactions to local anaesthetics, signs of fear or claustrophobia, obesity or an enlarged thyroid gland extending to the chest. The anterior and lateral parts of the skin of the neck are innervated by the superficial fibres of the cervical plexus, thus, the primary goal is to anaesthetise these fibres. In order to ensure complete comfort for the patient during the surgery, it is advisable to infiltrate the capsule of the thyroid gland with local anaesthetics via an ultrasound-guided method, combined with superficial sedation (Figure 1).
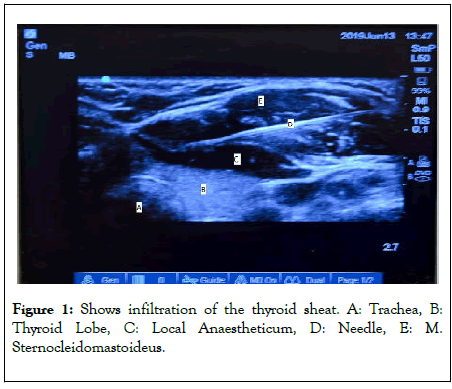
Figure 1: Shows infiltration of the thyroid sheat. A: Trachea, B: Thyroid Lobe, C: Local Anaestheticum, D: Needle, E: M. Sternocleidomastoideus.
Between May 2019 and March 2020, 9 surgeries in total, including 7 lobectomies, 1 thyroidectomy and 1 parathyroid adenoma surgery, were performed under regional anaesthesia in the Multidisciplinary Head and Neck Cancer Center of the National Institute of Oncology. The average age of the patients was 55 years (Range: 41–71 years) (Table 1). The innervation of the skin on the medial neck arises from the superficial fibres of the C1 to C4 cervical segment. Previous studies have shown that several structures of the neck (e.g. platysma) might have dual innervation arising from the cervical nerve and the cranial nerves. Moreover, the visceral innervation of the thyroid gland is provided by autonomic nerve fibres. Before the surgery, superficial anaesthetics on the operated side is applied in the cervical plexus under ultrasound guidance, administering 7 – 8 mL of 0.5% bupivacaine under the middle part of the sternocleidomastoid muscle, between the superficial cervical fascia and the prevertebral fascia, then applying 10 mL of 0.25% bupivacaine on the other side into the skin above the sternocleidomastoid muscle (by this method the fibres of the superficial cervical nerve towards the skin can be anaesthetised without the risk of blocking the phrenic nerve). Next, the virtual space between the true capsule and pseudo-capsule of the thyroid gland is injected with 20 mL of a 0.5% solution containing adrenaline and lidocaine under ultrasound guidance. In order to anaesthetise the platysma, 5 mL of 1% lidocaine is infiltrated subcutaneously before the incision. If the surgical plan includes the complete removal of the thyroid gland, bilateral subcutaneous infiltration of the sternocleidomastoid muscle is necessary, and if it is feasible, anaesthesia of the cervical plexus should not be performed in order to avoid bilateral diaphragmatic paralysis (rarely, the analgesic effect might be enhanced without a substantial risk of diaphragmatic paralysis by subcutaneous administration of a small amount of anaesthetics solely into the Erb’s point above the cervical fascia). Since the standard surgical positioning is uncomfortable, patients are superficially sedated in order to sustain their cooperation (Aim: Richmond Agitation Sedation Scale Score: -1 - (-2)) [11]. The surgery must be performed without face covering in order to ensure that immediate application of definitive airway management can be carried out. The opening consists of a traditional Kocher’s incision, measuring 3–4 cm in length, and a minimal under-preparation of the skin-platysma lobe. After separating the straight cervical muscles, the lobe of the thyroid gland is isolated or the parathyroid adenoma detected by ultrasound is approached. After careful preparation, the recurrent laryngeal nerve, the superior laryngeal nerve and the parathyroid gland are identified. Vessels in the upper and lower poles are coagulated with a high frequency electro-surgical unit. Revision is performed after the removal of the lobe and if necessary, a drain is inserted. Meanwhile, the integrity of the recurrent laryngeal nerve can be monitored continuously by talking with the patient. The platysma is and the skin are closed respectively with 3-0 and 4-0 or 5-0 absorbable running stitch. The wound is covered by Steri-Strip skin closure bandages. The patient is able to communicate immediately after the surgery when he/she is transferred back to the ward (Table 1).
| Indications |
|---|
| Patient preference |
| Gravidity |
| COPD |
| Pneumothorax in history |
| High perioperative complications due to cardiovascular status |
| PONV (perioperativ nausea vomiting) |
| Relative indications |
| Obesity |
| Claustrophoby |
| Pathologic lymph node |
| Anatomy of the neck |
| Neck surgery in history |
| Huge substernal goiter |
Table 1: Shows the indications and relative indications.
Papillary thyroid carcinoma (3 cases), follicular adenoma (2 cases), benign strumosis (2 cases), thyroiditis (1 case) and parathyroid adenoma (1 case) served as indications for surgery as confirmed by imaging techniques (cervical ultrasound or MRI) and fine-needle aspiration biopsy (FNAB). 7 lobectomies, 1 thyroidectomy and 1 parathyroid adenoma removal were performed. The average operating time was 42.7 minutes (Range: 25–80 minutes). The operating time covered the period between the incision and the wound closure. The preparation time for the regional anaesthetics did not take longer than the introduction of narcotics in general. Thus, compared to general anaesthesia, patients do not spend more time in the operation room. Complications occurred, but did not cause complaints to the patients; one patient temporarily suffered from unilateral Horner ’ s syndrome and one patient temporarily experienced paraesthesia in the left shoulder. These complications were presumed to have developed due to the anaesthetics that reached deeper layers. The patients received post-operative care for an average of 1.8 days (1–2 days). Complications requiring reoperation did not occur. Drains were removed the day after the surgery and patients were released from the hospital 1 or 2 days after the surgery.
The patients consumed fluids after the surgery and a few hours later they could take solid food as well. The patients’ need for analgesia was minimal, and they rarely reported nausea or vomiting. None of the cases required switching to general anaesthesia during the operation. Neither recurrent laryngeal nerve damage, nor hypocalcaemia occurred in any of the cases.
Globally, the incidence of thyroid diseases is on the rise. There are numerous indications for surgery including benign hyperplasia, strumosis and malignant tumours. However, some of the patients cannot be anaesthetised due to their comorbidities and some of them are afraid of general anaesthesia. General anaesthesia can be replaced by regional anaesthesia with the above contraindications and indications, thus, the complete removal of the thyroid gland which has not spread into the thoracic region and has not metastasised into the neck, as well as the removal of parathyroid adenoma causing hyperparathyroidism can be performed with the application of regional anaesthesia (Table 2).
| Gender | Age | Histology | Operation | Indication | |
|---|---|---|---|---|---|
| 1 | Female | 51 | Cc. papillare | Lobectomia gland thyr l.d. | 2 spontaneous PTX in history |
| 2 | Female | 48 | Thyreoiditis chronica | Lobectomia gland thyr l.s. | Patient preference |
| 3 | Female | 41 | Struma colloides hyperplastica | Lobectomia gland thyr l.d. | High perioperative complication due to cardiovascular status |
| 4 | Male | 71 | Struma colloides hyperplastica | Lobectomia gland thyr l.d. | High perioperative complication, ischemic cardiac failure in history, cardiac stent |
| 5 | Female | 40 | Cc.papillare | Thyreoidectomia totalis | Gravidity |
| 6 | Female | 40 | Adenoma folliculare | Lobectomia gland. thyr.l.d. | Lobectomia pulmonum in history |
| 7 | Male | 65 | Adenoma parathyreoidea | Exc.adenoma gland.parathyr.l.d. | COPD exacerbation,lobectomia pulmonum in history |
| 8 | Female | 40 | Adenoma folliculare | Lobectomia gland. thyr.l.s. | Patient preference, PONV |
| 9 | Female | 40 | Cc.papillare | Lobectomia gland thyr l.d. | Pulmonectomia az anamnézisben |
Table 2: Thyroid gland and parathyroid gland surgeries are performed on selected patients with the application of regional anaesthesia.
Preparation must be performed in an extremely careful manner, avoiding sudden and forceful movements during surgery. Patients should keep their head in the position required by the operation as long as possible, and only minimal movements are allowed on the operating table. Nausea and vomiting that can increase the risk of postoperative bleeding due to venous congestion occurs less frequently after surgery performed in regional anaesthesia compared to general anaesthesia. Hospitalisation becomes shorter, and patients experience little or no pain. If there is an indication, the day before the surgery the anaesthetist performing the blockade provides the patient with detailed information about the process as well as the advantages and risks of anaesthesia. Thyroid gland and parathyroid gland surgeries at our Department are performed on selected patients in regional anaesthesia, always taking into consideration the oncological principles.
Our previous experience confirmed that in the case of thyroid gland and parathyroid gland surgeries, regional anaesthesia as an alternative to general anaesthesia can be applied safely. Based on the indications and contraindications, this old method may once again take its place in the surgical repertoire and in certain cases, it could be the only feasible method.
Citation: Lévay B, Kiss A, Zelenai F, Elek J, Oberna F (2020) Thyroid Surgery in Local Anaesthesia: Renewal an Old Method. Thyroid Disorders Ther. 9:238. DOI: 10.35248/2167-7948.20.09.238
Received: 16-Jun-2020 Accepted: 30-Jun-2020 Published: 07-Jul-2020 , DOI: 10.35248/2167-7948.20.09.233
Copyright: © 2020 Lévay B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.