Internal Medicine
Open Access
ISSN: 2165-8048
ISSN: 2165-8048
Research Article - (2019)Volume 9, Issue 4
Patients with fibromyalgia (FM) present with chronic and diffuse musculoskeletal pain, a low pain threshold at specific anatomical points, weakness and fatigue, which eventually lead to reduced physical activity and decreased quality of life. Some studies have indicated a link between FM and personality and mental characteristics, but few have examined differences between women with FM and healthy women. The goals of this research were to investigate these differences, as well as the link between the degree of catastrophizing and coping with the disease among sick women. This comparative and correlative study examined 165 women 75 (46%) with FM and 90 (54%) healthy women. All the subjects filled out a socio-demographic questionnaire, the State and Trait Anxiety Questionnaire, and the Short Form Health Survey (SF-12). In addition, the women diagnosed with FM answered the Pain Catastrophizing Scale and the Fibromyalgia Impact Questionnaire (FIQ). We found that women with FM report high levels of anxiety and low levels of quality of life regarding their disease. It seems that their mental health is linked to their physical status. Interventions to improve mental health in this patient population may also bring enhancement in quality of life.
Fibromyalgia; Anxiety state; Anxiety trait; Pain catastrophizing; Quality of life
Fibromyalgia (FM) is a condition of chronic and diffuse musculoskeletal pain affected by a wide variety of comorbidity complaints and psychological factors [1]. Between 2 and 4 percent of the population suffer from this syndrome, and one of the common symptoms is a low pain threshold at specific anatomical points named trigger points [2,3]. The American College of Rheumatology (ACR) defined FM as the presence of diffuse pain along the skeleton, on the left and right side of the body, above and below the waist, and at 11 out of 18 trigger points for a period of at least three months [4]. These symptoms determine the diagnosis [5]. FM is also characterized by fatigue and sleep disorders, stress, anxiety and depression, difficulty thinking clearly (“fibro fog”), and could present comorbidity of Inflammatory Bowel Syndrome (IBS), headaches, PMS, and more [6].
Fibromyalgia can be found in any society, age or gender, but women between the ages 30-60 are more prone to have FM [7]. Risk factors that could increase the incidence of FM include female gender and low income, but the reasons for this are insufficiently clear [8]. Although some studies have shown that the perception of pain depends on sociodemographic and economic factors, other studies have indicated that anxiety, low self-esteem and decreased quality of life are related to the pain experienced by FM patients [9-12].
Fibromyalgia is a complex syndrome, and includes mental as well as physical elements [13]. Medical staffs often relay a message of “Everything is OK” or “It’s all in your head”, which label the patients as mentally disturbed or as impersonators, and definitely do not contribute to creating a positive and meaningful relationship between doctor and patient [14]. The literature on psychiatric morbidity in FM indicates that psychopathological evaluation of FM patients could shed light on the individual’s personality traits, which could affect the perception of pain and impair his or her quality of life [15]. Studies have shown that the link between FM and anxiety is especially strong, including evidence that anxiety often paves the way for the onset of chronic muscular pains [16,17].
Catastrophizing is the most studied psychosocial factor affecting pain. It is a negative cognitive-emotional reaction, characterized by a tendency to expect the worst about the experience of pain. Catastrophizing is conceptualized as a negative pattern of painrelated thoughts, including cognitions of helplessness, pessimism, rumination about pain, and magnification of pain complaints [18-22]. Negative pain-related cognitions are noticeable in individuals with FM (Loggia et al.). In patients with FM, catastrophizing is associated with enhanced nociceptive sensitivity and increased severity of FM symptoms [23].
A study that examined post-trauma patients who also suffered from FM found exacerbation of the symptoms when the patient’s mood changed for the worse, proving that there is a strong link between FM and psychiatric disorders, primarily mood disorders. About 65% of the FM patients suffered from mood disorders (21.12%) or major depression (43.66%), and significant quality of life deterioration [24].
As in other conditions characterized by chronic pain, FM can damage the ability to work, and social and family relationships, and as such, according to the World Health Organization, the health-related quality of life (HRQoL), which relates to the emotional, physical and social aspects of one’s daily experience that is affected by the syndrome and/or its treatment [6]. Studies have indicated that FM patients can lose their ability to work because of the symptoms that they suffer [25,26]. However, it was found that certain traits allow an individual to cope with the symptoms and improve quality of life: gratitude, hope, and positive thinking were found to be effective, to reduce pain, and to decrease the patients’ degree of fatigue [26].
The better we understand the mechanisms responsible for FMrelated chronic pain, and the factors related to the syndrome and its severity, the better we will be able to effectively help these women by adjusting the interventions and treatments. Also, providing care that helps FM patients and improves their symptoms could improve the medical and nursing staff’s communication with their patients [1].
Consequently, the goals of the present study were: 1) To examine the state and trait anxiety personality traits and quality of life of fibromyalgia patients in comparison to healthy subjects; and 2) examine the relationship between the degree of catastrophizing and coping with the illness among the FM patients.
Participants
The sample included 165 women 75 fibromyalgia patients (46%) and 90 healthy women (54%), aged between 18 and 64 (M=31; SD=9.7). The participants were recruited based on personal acquaintance with women diagnosed with the syndrome and designated social network groups.
Hypotheses
H1: Differences will be found between women with fibromyalgia and healthy women on state anxiety, trait anxiety, and quality of life.
H2: Women with fibromyalgia who demonstrate high pain catastrophizing will suffer from a higher degree of anxiety, decreased quality of life, and limited daily functioning.
Tools
A sociodemographic questionnaire included questions about the participants’ background data such as age, education, employment, country of birth, religion, comorbidity, medication, etc.
Anxiety was measured by means of a questionnaire first used [27]. This study used the Hebrew version of the questionnaire [28]. The first part of the questionnaire examines state anxiety, which relates to the present situation that is usually linked to an anxiety-increasing event. The subject rates her feelings on the day the questionnaire is answered. The second part measures trait anxiety, i.e. the subject’s usual, daily emotional state, and represents her potential to develop and experience state anxiety, which is typically determined by her past experience with various stressful situations (such as pain) and the tools with which she copes with these situations. Each part includes 20 items rated on a scale of 1 to 4. In this study, Cronbach’s α = 0.973.
Quality of life was measured by the Short Form Health Survey [29]. The questionnaire measures the respondent’s physical and mental health, and whether this state affects her day-to-day functioning and quality of life. It 12 questions and 8 scales: physical functioning (PF - 2 items on limitations doing moderate activities and climbing several flights of stairs), role limitations due to physical problems (RP - 2 items on less accomplishment than one would like to achieve and limitation in kind of work or other activities), bodily pain (BP - 1 item on pain interference with one's normal work), general health (GH - 1 item on general health perception), vitality (VT - 1 item on having energy), social functioning (SF - 1 item on interference of physical health or emotional problems with one's social activities), role limitations due to emotional problems (RE - 2 items on less accomplishment than one would like to achieve and not being careful in doing activities as usual) and perceived mental health (MH - 2 items on feeling calm or peaceful and feeling sad or blue). Response categories for items vary from 2- to 6-point scales, and raw scores for items range from 1 to 6. In this study, Cronbach’s α = 0.913.
The group of women diagnosed with FM completed two additional questionnaires; namely, the Fibromyalgia Impact Questionnaire (FIQ), and the Pain Catastrophizing Scale (PCS) [30,31].
The Fibromyalgia Impact Questionnaire includes 13 statements, and examines the effect of the syndrome on the patient’s everyday life, how many days a week she felt well and painless, whether she took days off work, etc. The symptom domain retained items on pain, fatigue, morning tiredness, stiffness, anxiety, and depression and added four additional items on tenderness, memory, balance, and environmental sensitivity. The symptom items are visual analog scales (0-10 cm), with higher numbers indicating greater symptomatology and greater severity. In this study, Cronbach’s α = 0.906.
The Pain Catastrophizing Scale includes 13 items that measure the three elements of catastrophizing in the context of previously-encountered clinical pain: rumination, for example “I can’t stop thinking about the pain”; magnification, for example “I feel something terrible may happen as a result of the pain”; and helplessness, for example “I thought there was nothing I could do to stop the pain”. The catastrophizing questionnaire was translated and validated in Israel by Granot and Goldstein- Ferber (2005). In this study, Cronbach’s alpha for each of the elements was: rumination α=0.93, helplessness α=0.92 and magnification α=0.65. The general validity of the questionnaire was α=0.909.
The questionnaires were distributed personally and via social networks dedicated to fibromyalgia (Internet forums of women diagnosed with fibromyalgia). All participants were informed of the goal of the study, and written informed consent was obtained from them to use the data obtained. Confidentiality and anonymity were guaranteed. The Committee of Bioethics of the Academic Center approved the investigation.
Statistical analysis
The data were analyzed using SPSS version 22.0. Independent ttests were used to examine the first hypothesis – finding the differences in state and trait anxiety levels and quality of life between women diagnosed with FM and the control group. Pearson correlations were performed to examine the relationship between the degree of pain catastrophizing and anxiety, quality of life, and daily functioning of FM women.
The research population is described in Table 1. Regarding comorbidity, the women diagnosed with FM are divided – about half of them reported comorbidity, whereas among the control group – 93% reported no comorbidity. 36% of the FM patients are not satisfied with their medical treatment and 29% are partially satisfied. Among the healthy women, 32% are partially satisfied and 29% are satisfied. It can also be seen that about half of the FM patients take medication regularly, but only 22% of the control group do (Figure 1). In addition, the findings indicate that other common illnesses reported by FM patients, besides neural disorders, include gynecological and pulmonary disorders.
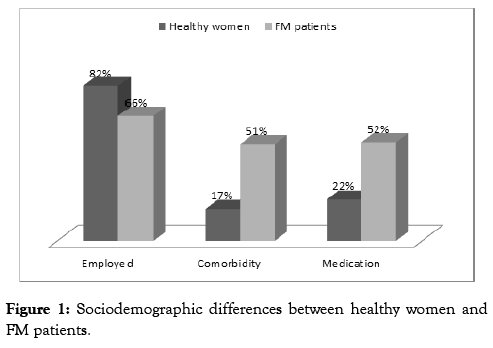
Figure 1: Sociodemographic differences between healthy women and FM patients.
| Fibromyalgia patients | Healthy women | ||
|---|---|---|---|
| Mean age | 32 | 26 | |
| Education | High school | 44% | 33% |
| First degree | 45% | 53% | |
| Second degree | 10% | 13% | |
| Employed | 66% | 82% | |
| Physical activity | 51% | 56% | |
| Salary compared to average | Low | 56% | 40% |
| Medium | 36% | 48% | |
| High | 8% | 10% | |
| Country of birth | Israel | 85% | 80% |
| US | 8% | 3% | |
| Former Soviet Union | 5% | 16% | |
| Europe | 1% | 1% | |
| Marital status | Single | 48% | 74% |
| Married | 39% | 26% | |
| Divorced | 11% | 0% | |
| Widowed | 2% | 0% | |
| Years of marriage | 1-5 years | 22% | 57% |
| 6-10 years | 11% | 5% | |
| 11-15 years | 22% | 5% | |
| 16-20 years | 15% | 23% | |
| Over 20 years | 30% | 10% | |
| Has children | 50% | 20% | |
| Religion | Jewish | 95% | 96% |
| Moslem | 4% | 1% | |
| Other | 1% | 3% | |
| Degree of religiosity | Secular | 71% | 80% |
| Traditional | 20% | 16% | |
| Religious | 9% | 4% | |
| Comorbidity | 51% | 17% | |
| Takes regular medication | 52% | 22% |
Table 1: Sociodemographic data of participants (N=165)
To examine the hypothesis that differences would be found between women with fibromyalgia and healthy women on state anxiety, trait anxiety, and quality of life we conducted t-tests for independent samples for each of the variables. We found that trait anxiety of women with FM is significantly higher compared to that of healthy women (t=8.2, p<0.01), and state anxiety of women with FM is also significantly higher than that of healthy women (t=6.1, p<0.05). Quality of life of women with FM was found to be significantly lower than that of healthy women (t=5.3, p<0.05).
The second hypothesis, namely that women with FM who demonstrated high pain catastrophizing would suffer from higher levels of anxiety, decreased quality of life, and limited daily functioning, was tested by Pearson tests for each variable separately. We found a positive relationship between high pain catastrophizing and the degree of trait anxiety (r=4.1, p<0.01), but not between catastrophizing and state anxiety. Additionally, a significant negative relationship was found between pain catastrophizing and quality of life, so that the higher pain catastrophizing was, the lower quality of life was (r=4.3, p<0.01). The level of pain catastrophizing was found to be positively related to the FM women’s degree of limited daily functioning (r=3.7, p<0.05). FM patients’ level of fatigue and their sensitivity to strong sounds and smells and touch were also found to be high (Figure 2).
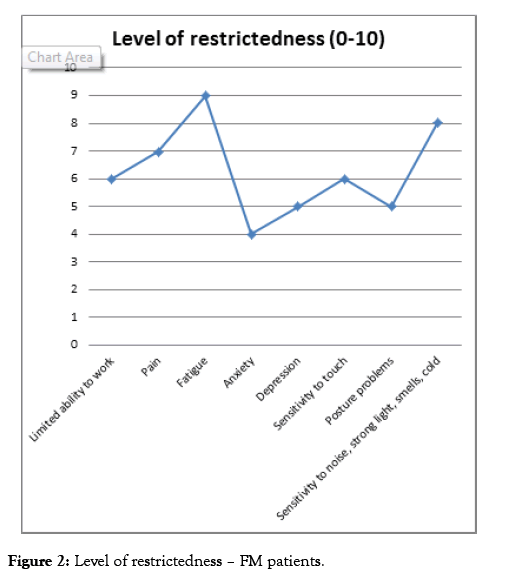
Figure 2: Level of restrictedness – FM patients.
Concerning FM women’s rating of their difficulty to perform everyday tasks, the tasks that were especially difficult were yard work, climbing stairs, washing dishes and preparing meals, vacuuming carpets, and changing bedding (Figure 3).
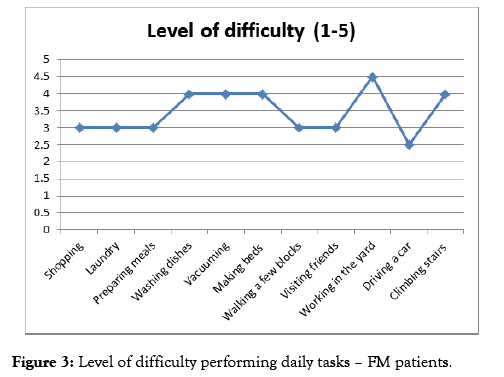
Figure 3: Level of difficulty performing daily tasks – FM patients.
The present study compared the perception of quality of life and state and trait anxiety and personality characteristics of women diagnosed with fibromyalgia and a control group of healthy women. It is also examined the relationship between the degree of catastrophizing and coping with the illness among FM patients. The findings indicate that the quality of life of healthy women is better than that of FM women. Furthermore, the level of anxiety of FM patients is higher than that of healthy women. In addition, a correlation was found between the levels of pain catastrophizing of women diagnosed with FM and their levels of trait anxiety, physical limitations, and quality of life.
These findings are similar to previous research that studied women diagnosed with FM, which found that FM patients reported more severe symptoms of depression, anxiety, insomnia and fatigue than controls, which constitute typical bodily and mental symptoms accompanying FM pain [32]. Elevated levels of pain catastrophizing and negative affect have also been previously observed [33-36].
It is known that patients with nonorganic somatic symptoms have elevated rates of psychological distress, anxiety and depression, and functional impairment. Studies found that FM negatively affects functioning at the physical, psychological, and social levels, impairing social relationships, ability to fulfill family and work responsibilities, daily life activities, and mental health [37-40]. The more unexplained somatic symptoms a patient presents with, the more psychiatric comorbid conditions she or he is likely to have.
The present study did not examine whether the anxiety stems from the existence of the syndrome or whether the anxiety itself could cause the syndrome. It is possible that the fact that a woman gets up in the morning and knows that the pain will attack at some point, or if she already gets up with the pain, she experiences more anxiety than a healthy woman does. The pain can appear in various social situations or at work, and generate feelings of helplessness, discomfort, lack of control, and problems with everyday functioning – which could in turn contribute to her anxiety. It is known that coping with chronic pain has severe psychological and physical effects such as anxiety, constant stress, over-sensitivity to any incidence of pain, seclusion, depression, and more. Hence, coping with FM in itself is not easy in a woman’s daily routine. It may be that this could explain the link between these women’s pain catastrophizing and their anxiety, functioning and quality of life. The results of this study also suggest that pain catastrophizing is related to poorer QOL outcomes. Similar to the findings of the present study, other studies have also suggested a relationship between pain catastrophizing and quality of life among patients suffering from chronic pain conditions [41,42]. Catastrophizing is defined as the tendency to mentally focus on pain and evaluate one’s ability to manage pain negatively.
Although the mechanisms by which catastrophizing influences the experience of pain are not known, one hypothesis is that pain catastrophizing influences the attentional focus on painful or potentially painful events. Persons who catastrophize have difficulty shifting their focus of attention away from painful or threatening stimuli, and attach more threat or harm to nonpainful stimuli [43-46]. These studies suggest that catastrophizing increases painrelated fear.
The present study also found that about half of the women with FM suffered from comorbidity, and about half of them took medication on a regular basis. This could be important to the results of the study, because fibromyalgia is frequently associated with psychiatric comorbid conditions, which may contribute to the development or persistence of symptoms or both. Patients who have an aspect of central pain amplification associated with mechanical or inflammatory pain and patients with FM are likely to exhibit higher levels of psychological distress and illness behaviors [47-51]. Galvez-Sánchez and colleagues (2019) found that FM reduces functioning in physical, psychological, and social spheres, and also has a negative impact on cognitive performance, personal relationships (including sexuality and parenting), work, and activities of daily life.
The present study points to the complexity of fibromyalgia and its uniqueness. The medical and nursing staff should take into account that the quality of life of FM patients is lower than that of healthy women. The personality characteristics such as anxiety and pain catastrophizing might be negative among women diagnosed with FM, and their degree could affect how they cope with the syndrome. Emotional aberrances may also be relevant with respect to optimizing psychological therapy of FM. The syndrome and its symptoms, and the relationship with personality anxiety levels characteristics and perception of pain, should be further investigated in an attempt to better understand the mechanisms of fibromyalgia and to tailor better treatment to each patient. Hence, future therapies for fibromyalgia will need to address the pain pathways involved in fibromyalgia; its associated comorbid conditions; or, more likely, both. Furthermore, clinicians should consider the present data and the associated studies as providing support for the clinical assessment of pain and catastrophizing in order to improve FM patient adjustment and their quality of life.
The sample of this study is not big and may not fully represent the entire population of FM patients and healthy women. Also, the data are subjective and were obtained through self-reporting and social networks. Regarding the group of FM patients, they may have answered the questionnaires when in pain and their medical condition while filling out the questionnaire is unclear. The timing may have affected the results.
All authors contributed to the design of the study and to the analysis and interpretation of the data. KG conducted the experiment, acquired data, and drafted the first version of the manuscript. All authors critically revised and completed the manuscript and approved the submitted version.
Citation: Grinberg K, Meshalhov D, Adadi D, Biton T (2019) The Role of Pain Catastrophizing and Anxiety Levels on Quality of Life in Fibromyalgia Compared with Healthy Women. Intern Med 9: 313. doi: 10.35248/2165-8048.19.9.313
Received: 12-Oct-2019 Accepted: 25-Oct-2019 Published: 02-Nov-2019 , DOI: 10.35248/2165-8048.19.9.313
Copyright: © 2019 Grinberg K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.