Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Perspective - (2022)Volume 11, Issue 1
Incidences of a new disease which ravaged the population living in around Lake Victoria shores and boarder district of Rakai emerged in the early 1980’s is HIV. It was characterized by severe diarrhea, malnutrition, respiratory disease and finally death. It was first defined by Dr. Mayanja at Kalisizo Hospital as a slimming disease and later to be changed as Silimu in the local Kiganda language. The causative agent of the new disease was later described and defined by Dr. Robert Gullow as the Human Immunodeficiency Virus (HIV) which causes Acquire Immunodeficiency Syndrome which is characterized by a hallmark of opportunistic infections. In the early through the mid-1980s the prevalence of HIV/AIDS was estimated to have been way above 18% coupled with a turbulent civil conflict, this had a severe toll on the national economy and quality of life.
Several efforts were directed towards understanding the life cycle of the new disease and possible preventive measures. This saw the formation on the Ugandan AIDS commission and others. Government and civil society worked together to find workable solutions too. Advances in medical science created possibilities in decoding the HIV genome which saw the development of antiretroviral drug molecules which have been further improved and made available to treat HIV patients improving their longevity and quality of life. Further research efforts have been directed towards understanding the different ports of HIV entry into the human host. Several routes were suggested including direct inoculation with infected blood through sharp instruments, intercourse with an infected individual and vertical transmission.
In the early 2000, large multination multisite randomized control trials were conducted in Kenya, South Africa at Orange farm and Uganda in Rakai to assess efficacy of male medical circumcision among sexually active males in the prevention of HIV acquisition. Interim findings from all sites reported protective effect of the intervention above 53% and the trials were stopped and UNAIDS and WHO recommended safe medical circumcision to be promoted and offered and public health level.
If male circumcision is to be promoted in HIV-infected areas, the following basic ethical requirements must be fulfilled: Sufficient material and human resources for circumcisions to be carried out safely; International and national commitments to low-cost circumcisions to allow fair access; thorough monitoring of the quality of follow-up care; adaptable policy based on community concerns over whether, when, where, and how circumcisions should be performed; monitoring of circumcision promotion messaging to ensure that prospective clients are aware of potential benefits and constraints; careful attention to the consent procedure and ongoing condom promotion to reduce the possibility of behavioral dis-inhibition;Initiatives to educate mothers and girls about male circumcision to combat possibly fatal misconceptions; Regarding the compliance of circumcision policies with international rules, which limit the extent to which individual rights can be violated in the sake of the benefit of the public.
The mechanism of HIV entry in by far known to be through the less keratinized inner layer of the foreskin of uncircumcised penis, which is prone to bruises and tears during sexual intercourse and has large surface area in direct contact with sexual fluids which usually have higher concentration of HIV and is resident for Langerhans cells rich in HIV target cells need in the transmission.
Over the course of 24 months, circumcision of HIV-infected men did not diminish HIV transmission to female partners; longer-term consequences could not be determined.
The usage of condoms following male circumcision is critical for HIV prevention. All these coupled together demise the foreskin and its removal reduces the risk of infection (Figure 1).
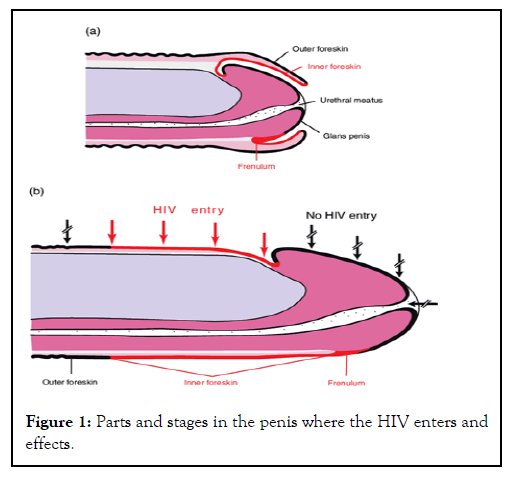
Figure 1: Parts and stages in the penis where the HIV enters and effects.
Citation: Katambala P (2022) The Intersect between Clinical Research and Health Policy: Ugandan Safe Male Circumcision Policy for HIV Prevention. Andrology. 11:250.
Received: 03-Jan-2022, Manuscript No. ANO-22-250; Editor assigned: 06-Jan-2022, Pre QC No. ANO-22-250(PQ); Reviewed: 17-Jan-2022, QC No. ANO-22-250; Revised: 24-Jan-2022, Manuscript No. ANO-22-250(R); Published: 31-Jan-2022 , DOI: 10.35248/2167-0250.22.11.250
Copyright: © 2022 Katambala P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : NO