
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Case Report - (2021)Volume 11, Issue 6
Background: Strychnos nux vomica is a member of Loganiaceae family. It has highly poisonous alkaloids strychnine and brucine, mostly in seeds. It has been used as rodenticides and to kill stray dogs. Homicidal and suicidal cases have also been reported. The use of strychnine is regulated in many countries. However, it is used in indigenous system as treatment for many conditions. But, these have no medical evidence.
Case report: We report the case of a 66 years old lady who presented with episodic spasms after consumption of water in which, this plant stem was soaked overnight. She had tautness of her muscles, multiple episodes each lasting for about 5 to 10 seconds. In between spasms, clinical examination findings were normal. All her blood investigations were normal except for slightly elevated muscle enzymes.
The history of plant product consumption and episodic spasms with intact consciousness made us think of strychnine poisoning. But, no toxicologic tests for the same were available. Hence we proceeded with the toxicologic analysis for alkaloids in the plant stem. The presence of natural alkaloids like strychnine and brucine were confirmed by chemical extraction techniques. She was managed conservatively with diazepam, IV fluids and other supportive care. She recovered completely and was discharged in stable condition.
Conclusion: Ingestion of strychnine (especially fruits, seeds) can cause uncontrolled muscular contractions. The consequences following such uncontrolled seizures is life threatening. Lethality depends on the dose. There is no antidote for strychnine and supportive care is the mainstay of treatment.
Episodic spasms; Strychnine; Awake seizures; Poisoning
Strychnos nux vomica is a deciduous tree, native to India and South East Asia. It belongs to the Loganiacea family. Tree trunk is thick short and has ovate leaves.
Fruits when ripe are orange in colour. Seeds are hard, odourless and have bitter taste (Figure 1). It is known by various names in India like mushidi, kanjiram etc.
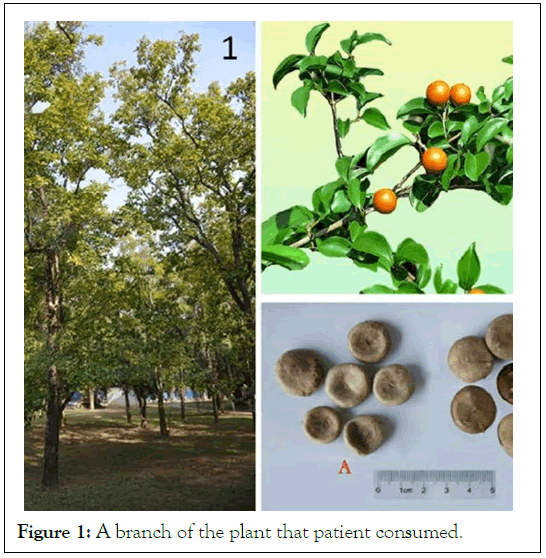
Figure 1: A branch of the plant that patient consumed.
The active alkaloids found in this plant are strychnine and brucine. Varying concentration of these alkaloids are present in almost all parts of the plant however, seeds are the richest source of these [1].
It was earlier used as an arrowhead poison. It had been used as CNS and circulatory stimulant in indigenous system [2]. As per folk medicine, the herb can be used only after various purification procedures or else it acts as poison.
Some of the uses include treatment of diabetes, worm infestations, and erectile dysfunction etc, (not proven scientifically). In India, majority of the cases are due to deliberate self-harm. Accidental cases from indigenous medical products and homicidal cases are also reported.
A 66 years old female diagnosed case of diabetes mellitus and hypertension on regular treatment presented with history of episodic spasms. Patient had tightness around mouth, face and whole body that lasted for five to ten seconds and recurred after thirty to forty seconds. In between she was fine except for pain over muscles. There was no history of tongue bite, frothing of saliva, weakness of limbs, urinary or fecal incontinence or other focal neurologic deficits. She continued to have such spasms for a total of five minutes and hence was taken to our hospital. One such episode occurred in front of us. On examination, her vitals, RBS were normal. In between the episodes, general and system examination were normal. During spasm, she had all her masseters were taut, had tonic posturing of her body but no hyperextension. We managed her with IV diazepam, tetanus toxoid, analgesics and intravenous fluids and were shifted to a dark room. On investigations, ECG, chest X ray and NCCT head were normal. All her blood routine investigations were normal except for slightly raised muscle enzymes.
She did not have any further episodes of spasms. Next day, she gave a history that she had consumed some indigenous drug preparation (remedy to diabetes) the prior morning, 30 minutes before she developed the symptoms. A plant stem soaked overnight in water and consumed the water (bitter in taste) (Figure 2).
Figure 2: Plant stem used by patient.
Episodic spasms with intact consciousness following the consumption of a plant product a possibility of strychnine poisoning was kept. Adding on to this was the local name of this drug “Mushidi”; the vernacular name for strychnine in Telugu (A language in India). None of the laboratory was doing tests for evidence of strychnine in urine or serum. Hence, we proceeded to do chemical analysis of the plant stem. The scientists at the Indian Agricultural Research Institute (IARI) at Pusa did extraction and alkaloid testing in the specimen. Nitric acid test and sulphuric acid dichromate tests were done and these confirmed the presence of brucine and strychnine in the specimen respectively.
She was managed conservatively with IV fluids, diazepam and supportive care. An injection of tetanus toxoid was given and was shifted to a dark room (tetanus was a close differential for strychnine poisoning). Her spasms stopped after diazepam injection. Analgesics were given on day one for muscle pain. Lethality depends on the dose. Bark and roots have relatively low concentrations of the alkaloids when compared to seeds. Moreover, she consumed water in which the plant stem was soaked. Hence, a small dose only had reached her bloodstream. She responded to our treatment. She recovered fully and was discharged on the fourth day.
Strychnine is rapidly absorbed from all routes [3]. There is negligible plasma protein binding and hence is rapidly cleared off from the blood [4,5]. 20% of the ingested drug is excreted unchanged in urine, upto 70% in the first 6 hours [4,6]. The major route for removal of Strychnine is the liver microsomal enzyme system [7].
The lethal dose for human adults ranges between 30 mg to 120 mg. The lethal dose for children is about 15 mg [8]. Strychnine prevents glycine uptake at the inhibitory synapses in the spinal cord and blocks the recurrent inhibition of Renshaw cells in the spinal cord, this causes uncontrolled stimulation of post synaptic neurons leading to involuntary diffuse muscle contractions [9]. However, it does not affect the higher centres and so mental status would be preserved until late in the disease.
Clinical manifestations begin with a prodromal stage followed by a clinical stage [8]. Onset of clinical features of strychnine poisoning varies with routes of exposure (5 minutes after inhalation, 30 minutes after ingestion and upto 24 hours after transdermal exposure) [10,11]. The prodromal symptoms include apprehension, restlessness, heightened sense of awareness, hyper-reflexia and muscular stiffness.
The sine qua none of clinical stage is awake seizures or spinal seizures, wherein the patient demonstrates tonic clonic seizure activity but remains fully alert throughout and afterwards. Convulsions may last from 30 seconds to 2 minutes. Severe cases may be associated with opisthotonus, trismus and risus sardonicus. Uncontrolled muscle contractions can lead to tachycardia, hyperthermia, airway compromise due to laryngeal spasm, rhabdomyolysis, lactic acidosis, hyperkalemia, metabolic acidosis, renal failure etc. Thus, if unchecked severe strychnine poisoning can cause death in several hours due to these complications.
A close differential diagnosis of strychnine poisoning is tetanus. Tetanospasmin prevents release of glycine, causing excitation of motor neurons in spinal cord. The onset of symptoms are more gradual in tetanus. All muscles are not involved simultaneously and the muscles are not completely relaxed in between convulsions in it. To detect strychnine, thin layer chromatography can be done on gastric aspirate and urine samples within initial hours. Blood testing is unreliable due to transient nature.
The principles of management of strychnine poisoning are similar to any other poisoning. There is no antidote for strychnine. The role of gastric lavage with saline, activated charcoal are only in the initial hours to reduce systemic absorption in cases of ingestion. The goals of management are to secure airway by endotracheal intubation and mechanical ventilation, to control seizures using diazepam with or without other short acting barbiturates, to maintain adequate hydration and to manage complications related to rhabdomyolysis and kidney failure with hemodialysis. Cooling blankets and dantrolene can be used for hyperthermia.
Strychnine is a lethal poison. Symptoms are sudden, mostly related to motor nervous system. Severe convulsions can cause a myriad of consequences that can lead to death if not treated promptly. There is no antidote for it and management is supportive. This is a concern for countries where even today indigenous medicines are used widely.
Dr. Moolchand Singh, Senior scientist, Indian Agricultural Research Institute (IARI), Pusa for chemical testing in the plant specimen.
Citation: Bindu IM, Tonk RS (2021) The Dose Makes the Poison: A Case Report on Strychnine Toxicity. J Clin Toxicol. 11:497.
Received: 10-Dec-2021 Accepted: 24-Dec-2021 Published: 31-Dec-2021
Copyright: © 2021 Bindu IM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.