Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Research Article - (2016) Volume 6, Issue 3
Background: The accuracy and reliability of non-invasive oximetry for haemoglobin measurements were reported in operating rooms and intensive care units, though few studies evaluated this technology in emergency departments. The purpose of this study was to evaluate the accuracy and reliability of non-invasive SpHb readings from a portable device, in emergency department patients, compared to synchronous LabHb measurements. The authors sought to minimise external variables that could influence device performance, including learning curves and patient conditions, thus performed measurements by one trained user on stable adults only.
Methods: The authors enrolled 24 consecutive adults admitted to the emergency department suspected or manifest active bleeding, and excluded cases of incarceration, pregnancy and burns. Haemoglobin concentrations were synchronously measured by phlebotomy laboratory analysis (LabHb) and using non-invasive readings (SpHb) from a portable Pronto-7 Pulse CO-Oximeter.
Results: The non-invasive SpHb concentrations were recorded in 24 patients (100%), but the device it aborted during one or more measurement in 8 patients (33.3%) due to tremor and shivering. Paired comparison of SpHb and LabHb revealed a mean absolute error of 1.2 ± 1.3 g/dL (median 0.7, range 0.1 to 0.5), which equates to relative error of 9% ± 14% (median 5%, range 1% to 59%).
Conclusions: Non-invasive SpHb measurements deviate from the ‘gold standard’ LabHb by an average of 1.2 g/dL (10%), but that outliers could be up to 5.2 g/dL (59%), which could lead to conflicting clinical decisions. Furthermore, the device functioned correctly in only 16 of 24 patients (66.6%), which should be reviewed in the light of difficult emergency department settings.
Keywords: Anaemia, Pulse CO-oximetry, Non-invasive, Haemoglobin
Anaemia is the most common haematological disorder, affecting 24.8% of the population, is age and gender depended and is frequently encountered in the emergency department [1,2]. Moreover, in surgical patients anaemia has an incidence of 30.4% and trauma-related haemorrhages are a leading cause of death and disability, particularly in patients with brain injuries [3,4]. The emergency physician therefore needs to monitor external or internal bleeding in trauma patients, in order to decide whether they should be discharged, or if they require blood transfusion or further treatment [4,5].
Blood loss is typically monitored by sequential phlebotomy assessments of haemoglobin concentrations [6]. The repetitive withdrawal of blood needed for laboratory haemoglobin (LabHb) measurements has a number of drawbacks, as it is invasive to the patient [5,7], exposes health workers to biohazards [4,5], and incurs considerable time and costs [8]. With critically ill patients, time is of paramount importance, and emergency departments (ED) need rapid assessments, where even ‘point-of-care testing’ may be too slow [8].
Increasing demands for in situ or real-time monitoring of haemoglobin concentrations recently led to development of noninvasive Signal Extraction Technology (SET) that can determine blood constituents based on light absorption or spectrophotometric analysis [5]. Advanced signal processing algorithms and unique adaptive filters work together to quantify haemoglobin concentrations [5,6]. The portable Pronto-7 Pulse CO-Oximeter (Masimo Corp. Irvine CA, USA) was developed for spot-checks of haemoglobin (SpHb) concentrations in patients with trauma (including brain or arterial polytrauma) or gastric bleeding, as well as for triage of patients with different levels of anaemia at emergency departments.
The aim of the present study was to evaluate the accuracy and reliability of non-invasive SpHb readings from a portable device, in emergency department patients, compared to synchronous LabHb measurements. The authors sought to minimise external variables that could influence the performance of the portable device, including user learning curves and different patient conditions, thus designed the study to be performed by a single user on stable adults only. The hypothesis was that limiting user and patient variations, the device could demonstrate sufficient accuracy and reliability, which could render it a useful tool for decision-making in a category of cases in the emergency department.
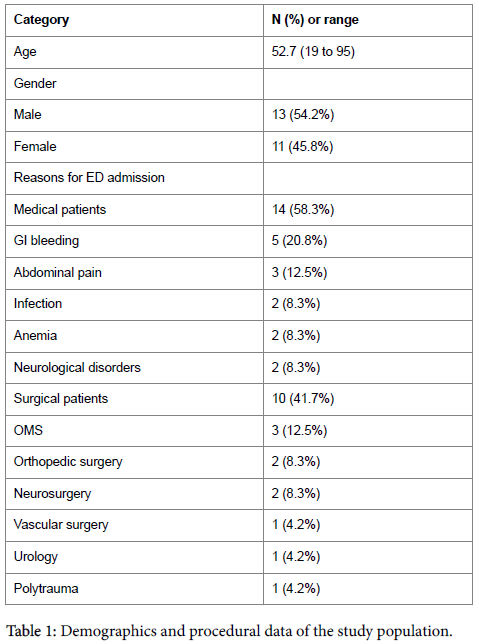
This observational study was conducted over a period of one week at a level-one emergency department of a university hospital. The authors enrolled 24 consecutive adults admitted for various reasons, with suspected or manifest active bleeding (Table 1), and excluded cases of incarceration, pregnancy and burns. Their haemoglobin concentrations were synchronously measured after clinical examination using: (i) phlebotomy samples analysed at the hospital central laboratory (LabHb) with an ADVIA 2120i haematology analyser (Siemens Corp., Munich, Germany), and (ii) non-invasive readings (SpHb) from a portable Pronto-7 Pulse CO-Oximeter (Masimo Corp. Irvine CA, USA).
The non-invasive measurements were acquired by one registrar who had sufficient training with the portable device. These readings were not used for clinical decision-making as the device was not approved for routine use in the emergency department at our centre. The portable device was systematically connected to the patient’s finger while blood was being withdrawn for laboratory analysis. If the measurement was successfully performed, the device reported total haemoglobin as well as arterial oxygen saturation and pulse rate. If the measurement aborted due to excessive movement or agitation, the device simply displayed an error message.
Haemoglobin concentrations (LabHb and SpHb) were measured on admission (Phase 1) and multiple times thereafter as required (Phase 2). The frequency repeats measures depended on evolution of clinical symptoms and diagnostic tests. In addition, blood pressure and pulse rates were also monitored, in most patients
The study was performed according to the Good Clinical Practice guidelines of the university hospital. As the device evaluated was already available commercially, it was not necessary to obtain approval of the ethics committee, as per local law.
Statistical analysis
The analytic approach between the two methods was based on a Blant-Altman analysis, calculating bias as the mean difference between the two methods and limits of agreement as the range in which 95% of the differences between the two methods are expected to lie.
The correlation between paired non-invasive and invasive measurements was evaluated by a paired t test and repeated measures analysis and trend analysis, using SPSS 17.0 and Sigma plot 12.5 and setting significance to p<0.05.
To assess the studies power to detect a significant difference between the two methods of Hb measurement we calculated achiever Power using G*Power Version 3.1.9.2 [9] using an alpha probability of 0.05 and assuming a two-tailed test of two dependent means.
24 patients, aged between 19 to 95 years, were enrolled in the study. Demographic and procedural data are presented in Table 1. A total of 26 blood samples were taken. In 8 of the patients pulse CO-oximetry has failed to detect SpHb at first sample time point (phase 1). In only one of those patients detection at the second sample time point (phase 2) was possible. In two patients laboratory measurement of haemoglobin was not performed at phase 1.
In the remaining 14 patients 14 paired measurements at phase 1 and 2 paired measurements at phase 2 could be analysed.
The non-invasive SpHb concentrations were recorded upon admission (Phase 1) and for repeat readings (Phase 2) in 24 patients (100%), but the device it aborted during one or more measurement in 8 patients (33.3%) due to tremor and shivering.
For Phase 1 measurements, the mean SpHb was 13.2 ± 2.7 g/dL, while the mean LabHb was 12.7 ± 3.0 g/dL (p=0.708). For Phase 2 measurements, the mean SpHb was 12.7 ± 3.4 g/dL, while the mean LabHb was 13.4 ± 1.8 g/dL (p=0.205).
Paired comparison of SpHb and LabHb measurements revealed a mean real error of -0.2 ± 1.6 g/dL (median -0.4, range -2.3 to 5.2) and a mean absolute error of 1.2 ± 1.3 g/dL (median 0.7, range 0.1 to 0.5). In relative terms, the mean absolute error was 9% ± 14% (median 5%, range 1% to 59%).
Because of some extreme values observed in our data, we also performed a sign test for related samples of SpHb and LabHb measurements for Phase 1 and Phase 2. The analysis verified the results obtained by paired t test with no statistical significant difference between measurements in both phases (p= 0.18 and p=0.50, respectively)
Bland- Altman analysis showed good agreement between the two measurements. The mean difference (i.e., bias) between methods was 0.2 with lower limit at -2.73 and upper limit at 3.13. Only one point fell outside of the upper limit (Figure 1).
Finally, post-hoc power analysis for both phases indicated that the achieved level of power was relatively small (0.06 and 0.18, respectively) suggesting that the sample size of the present study (N= 24) may have played a limiting role in the statistical significance of the comparisons conducted.
The achieved power to detect a clinically significant difference of 10 or more points in Hb between the two measurement methods was 97.2%.
We aimed to evaluate the accuracy and reliability of non-invasive SpHb readings from the portable Pronto-7 Pulse CO-Oximeter, compared to synchronous LabHb measurements in emergency department patients. The results from this small cohort demonstrate that, although Bland-Altman analysis showed a good agreement between the two methods, non-invasive SpHb measurements deviate from the ‘gold standard’ LabHb, by an average of 1.2 g/dL (10%), but that due to the small number of study population the bias may be up to 5.2 g/dL (59%). Furthermore, the device functioned correctly in only 16 of 24 patients (66.6%), which do not provide sufficient reliability for routine use in the emergency department.
The accuracy and reliability of the portable Pronto-7 Pulse COOximeter was reported in numerous studies conducted in the operating room [10-21] and in the intensive care unit [4,5,22-25] with predominantly satisfactory performance. In a study done in bleeding trauma patients the agreement was moderate [bias (LOA) of -0.6 (-3.0; +1.9)] g/dl [26], where the limit of agreement is defined as the mean difference + twice the standard deviation of the differences [27]. In the subgroup analysis, the pooled mean difference and SD were 0.4 + 1.3 g/dL (-2.2 to +3.0 g/dL) in 13 studies conducted in the peri-operative setting and -0.5 ± 1.6 g/dL (-3.63 to +2.62 g/dL) in 13 studies conducted in the intensive care unit setting. The authors concluded that the results showed that the mean difference between the methods and the SD of non-invasive laboratory values were small. But, due to the wide limits of agreement, physicians should be cautious when making clinical decisions [8]. Moreover, sensitivity and specifity of non-invasive haemoglobin measurement varies in different studies ranging at the critical threshold of 8 g/dl from 16.9 to 91% and 40 to 94.6% respectively [28,29], suggesting that non-invasive SpHb technology should be used with caution.
The studies that evaluated the performance of the Pronto-7 Pulse CO-Oximeter in the emergency department, however, reported high bias and poor reliability [30-32]. Gayat et al. and Gayat et al. [31,32] reported that in the clinical usefulness of the device in the emergency department was debatable and that “SpHb is systematically biased and too unreliable to guide transfusion decisions”, while Galvagno et al. [30] simply concluded that “SpHb did not enhance predictions of needs for transfusion.
Non-invasive haemoglobin measurements not only depend on haemoglobin concentrations, but may be influenced by peripheral perfusion, hypothermia, cardiac output, shock – and drug-induced vasoconstriction, high bilirubin concentrations and severe anaemia – which could play a role in the emergency room [5,33,34]. Recent studies have in fact shown that the correlation between SpHb and LHb is reduced in patients with significant haemorrhage or at risk of haemorrhage [4,25,35]. In contrast, other studies have found that significant intraoperative haemorrhage or controlled hypotensive anaesthesia have no major effect on SpHb [36,37]. Further work is needed to clarify the possible role of these factors. Moreover, known variables that affect the accuracy of the pulse CO-oximetry include movement and sensor position, while the device calculates haemoglobin values. This may require repeated measurements and may reduce the reliability of the device in the emergency department, where often patients are anxious, agitated and intoxicated. Since the device uses signal extraction technology another limitation especially for the emergency department is the presence of tar, soot and nail polish on the fingers of the patients.
The SpHb technology has the potential to support processes in the ED and to help to optimise the treatment of ED patients. Firstly, it could be used as a triage tool to detect patients with anaemia. Secondly, it might expedite the detection of critical illness and thus improve patient safety. Thirdly, it could enhance patient satisfaction by avoiding invasive Hb testing and thus reduce costs.
For the emergency department itself, non-invasive haemoglobin measurements can improve workflow management. If diagnosis, treatment and discharge are accelerated, costs will be reduced. At the IEDLI conference, it was proven that showed that the inclusion of technologies in the ED can decrease the patient’s time in hospital by 10% [37]. If we have 50,000 patient visits per year, this corresponds to an additional capacity of 2,000 patients. In addition to decreasing laboratory costs with the non-invasive Hb measurement, an ED with 50,000 patient visits per year and a patient-to-nurse ratio of 4:1 can save up to 5,000 care hours, as well as the corresponding personnel costs.
This study has numerous limitations, notably its very small cohort size and lack of inter-observer testing. Because the non-invasive device was not formally approved for use in the emergency department, it was not possible to assign more than one trained observer for one week to perform the SpHb measurements. The preset exclusion criteria were also strict to eliminate cases in which non-invasive measurements would be difficult or flawed. No patient experienced significant haemorrhage or haemodynamic instability. In addition, as the vast majority of the patients had Hb levels > 8 g/dL, we did not investigate the accuracy of the method in the low range (< 8 g/dL). SpHb values may be less accurate in severely anaemic patients.
The results of the present study suggest that non-invasive SpHb measurements deviate from the ‘gold standard’ LabHb by an average of 1.2 g/dL (10%), but that outliers could be up to 5.2 g/dL (59%), which could lead to conflicting clinical decisions. Furthermore, the device functioned correctly in only 16 of 24 patients (66.6%), which should be reviewed in the light of difficult emergency department settings.
The authors declare that there is no conflict of interest. Our unit has been equipped by the manufacturer with two Masimo Radical 7® devices for evaluation. No financial support was received. The manufacturer was not granted any intellectual properties related to the data nor did the manufacturer have any right to influence the selection, evaluation, or discussion of the data.