Internal Medicine
Open Access
ISSN: 2165-8048
ISSN: 2165-8048
Research Article - (2022)Volume 12, Issue 1
Background: The coronavirus disease 2019 (COVID-19) has been a pandemic and has affected mortality worldwide. The Cox Proportional Hazard (CPH) model is becoming more popular in time to event data analysis. When there are unobserved/unmeasured individual's factors, then the results of the CPH may not be reliable. So, this study aimed to determine the association between frailty and survival time in hospitalized COVID-19 patients.
Methods: This was a Single-center observational study conducted at one of the hospitals in Iran. So that, hospitalized patients with confirmed COVID-19 were included. Epidemiological, clinical, laboratory and outcome data on admission were extracted from electronic medical records. After selecting the most important prognostic risk factors on survival, CPH and gamma-frailty Cox models were used to identify the unadjusted and adjusted effects of the risk factors.
Results: 360 patients with COVID-19 enrolled in the study. The median age was 74 years were men and 42·3% were women, the mortality rate was 17% The results of the CPH model showed that, hypertension, sex, age and smoking status increase the mortality hazard of death due to the covid-19 (P<0.05). Furthermore, the frailty model showed that there is at least a latent factor in the model (P=0.005). Age and platelet count were negatively associated with the length of stay, while red blood cell count was positively associated with the length of stay of patients.
Conclusions: Both the frailty and CPH model indicate that in addition to age, the frailty factor is a useful predictor of survival in patients with COVID-19 and disease outcomes were better predicted by considering frailty than either age or comorbidity.
Survival model; Frailty; Cox model; COVID-19
Coronavirus disease 2019 (COVID-19), has become one of the most health challenges that rapidly affected mortality worldwide [1]. COVID-19 is usually asymptomatic. These patients often improve without specialized medical care. Besides, a considerable proportion of these cases intensify their disease and acute severe respiratory failure [2]. These COVID-19 patients usually need hospitalization, intensive care unit admission, and in most cases require intubation [3].
The time-to-event analysis is a series of statistical analyzing the methods in which, the outcome variable is time until an event occurs. The event can be death, recovery, recurrent or disease incidence, and survival time is often defined in days, weeks,months, or years. A key feature in survival analysis is that not everyone will necessarily experience the event of interest within the specified time of the study, so some individuals are censored [4,5]. The key concept in survival analysis is the hazard function that describes the instantaneous risk of the event for an individual who has not already experienced the event. Subjects may differ due to the hazards. For example, in terms of hazards; patients with the more severe disease tend to die earlier and have a higher hazard than less severe ones. Such hazard can be included in survival models as Cox’s proportional hazards model [6,7].
It is possible to account for all relevant covariates in the model scarcely. These variables account for observed heterogeneity, and the unaccounted part is considered unobserved heterogeneity.
The effects of unobserved heterogeneity are referred to as frailty. The frailty is an unobserved individual random effect that acts multiplicatively on the hazard. The estimated variance is a preventative of this unobserved heterogeneity [8,9].
Frailty models can be used to explain the effects of the selection of healthier subjects over time, and also to explain deviations from the proportional hazards model. In shared frailty models, it can be used to model dependence of survival times in clustered data or recurrent events. Here the frailty term is shared among individuals in the same cluster [10].
Studies of the clinical and epidemiologic characteristics of COVID-19 have been conducted in many countries. With increasing clinical experience, more detailed information has been discovered concerning COVID-19. As one of the first conducted studies, Huang et al revealed clinical manifestations of these patients and observed that Intensive Care Unit (ICU) patients had higher plasma levels of cytokines compared with non-ICU ones [4]. Another study reported that the disease most probably affected older male’s parameters of severity and comorbidities. Also, other studies compared clinical non-severe patients. As result, ICU patients were significantly older and more likely to have some comorbidities [11,12]. These studies were single-center with univariate analysis without consideration of the influence of heterogeneity and unobserved or confounding factors because of their small sample sizes [13]. So, accounting for this factor and clarifying the independent highrisk factors with considering the frailty by fitting a multivariate Cox frailty model to analysis and establishing an accurate prediction of COVID-19 has become desirable [14]. Therefore, in this study, we used the cox frailty hazard model to provide a highly accurate risk-estimation model. Moreover, a comparison of survival data across gender and age groups was done. To probably unmeasured factors affecting survival time among hospitalized covid-19 patients in Birjand, this study aimed to fit cox frailty model to account for the unobserved factors affecting their survival time.
Study design
A retrospective, single-center observational study was performed among COVID-19 patients at the general hospital in Birjand, Southeast Iran. We examined a systematic random sampling from admissions patients with COVID-19 from 1 March 2020 to 15 November 2020. All hospitalized patients admitted and diagnosed with COVID-19 were included. Inclusion diagnostic criteria were positive real-time Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR) or a clinical diagnosis made by the radiological responsible clinician based on signs, symptoms, or radiology consistent with COVID-19.
The only exclusion criteria were incomplete hospital records during data analysis that were retained from the study. We applied recorded hospital data of COVID-19 patients for analysis. A checklist form was used for data collection. A data protection policy was followed to record data securely for statistical analysis. Demographic variables such as age and sex were included. Selected variables for analysis were based on prognostic indicators used including a history of coronary artery disease, diabetes, and hypertension; smoking status; and blood biomarkers in recent COVID-19 studies. Clinical, laboratory and radiographic parameters were extracted from electronic health records.
Outcomes
The basic outcome was time to death, indeed (time from hospital admission to death in day. Patients, who were still alive in the hospital at the end of follow-up, were censored for survival analysis. For patients that died, the date of death was considered for survival analysis. In other words, time from hospital admission to mortality).
Mortality
All-cause mortality was obtained from electronic hospital records. The follow-up period was the time between admission and death, discharge, or end of the study. For those patients who died in the hospital, we retrieved the cause of death as COVID-19 deaths versus non-COVID-19 deaths. Hospitalization was defined as stay in a hospital for at least one day, so outpatients were not included. Due to time is in discrete days, at time zero, survival is 100%.
Ethics approval
All procedures in this study were approved by the Ethical Committee of Birjand University of Medical Sciences, reference number: IR.BUMS.REC.1399.185
Statistical analysis
Before doing the analysis, the dataset was cleaned and the accuracy of the data was checked in partnership with the medical record office. To analyze whether the included variables and comorbidities were predictive of in-hospital mortality we performed the Cox hazard model. We first tested these variables individually in univariate Cox models adjusted for age and sex. Those predictors that were significant in the univariate models were further entered in multivariate models, again adjusting for age and sex. Since some important factors were not recorded in the data, probably, it was a great heterogeneity between patients. So a cox frailty model is utilized to account for unobserved variables. The frailty factor is an unobserved multiplicative effect on the hazard function that in this study we considered gamma distribution for frailty component in the model.
Variables, such as age, sex, and smoking status grouped into were included. Obesity was grouped using categories derived from the WHO classification of BMI. The comorbidities including asthma, chronic heart disease, diabetes, chronic neurological diseases, common autoimmune diseases, cancer, and a diagnosis of hypertension were also considered. The specified outcome: Time to mortality was analyzed with the Cox frailty hazard model, containing a random effect to account for variation occurring between patients and adjusted for the aboveselected variables. Both crude and adjusted HRs was estimated along with 95% confidence intervals. Each analysis was reported with a Kaplan-Meier survival plot. Both crude Odds Ratio (OR) and adjusted OR were presented with associated 95% CIs.
Sample characteristics
From 20 May 2020 to 20 September 2020, we screened a total of 360 patients from a general hospital after the exclusion of patients with no clinical record or missingness in diagnosis record aged 21 years and older who were diagnosed with COVID-19. So, complete data were available for (95·4%) of included patients, imputation technique was used for missing status and all outcomes were completed for all patients.
The median age was 42 years (minimum 23, maximum 97 years), minimum follow-up time was 2 days and the maximum follow-up time was 46 days and 52.4% were men. The overall mean (sd) of the patient's survival time was 16.4 (1.3) days. The median survival time for dead patients was 8 days. 313 patients were discharged. The median length of hospital stay for those patients was 10 days.
The hospital mortality rate in the patients with COVID-19 was 17%. The mortality rate was higher among the patients with COVID-19, and they were older, frailer, and had higher prevalence of comorbidities, such as diabetes and hypertension, compared with the other patients. Most patients admitted to the hospital are middle-aged and 75% being 58 years or less. A large variation was observed for clinical variables, with most ranging very abnormally.
We reported the results of non-frailty and frailty models respectively. As findings shows, in models, age groups, gender, and comorbidity are related to the hazard rate significantly. The result of the frailty cox model shows that the hazard of mortality due to COVID-19 in male sex with an age bigger than 60 years is about 3.2 times compared to the men with an age less than 60 years (P=0.023). Moreover, it can be seen that comorbidity increase the death hazard (P=0.002). A negative coefficient for age categories indicated that these patients had worse prognoses, compared to 18-39 years one. However, these findings were not significant statistically. For those aged ≥ 80 years old, coronary artery disease and hypertension were also associated with mortality. No difference in the radiological and clinical diagnosis of COVID-19 was observed by sex (results were not shown).
The unadjusted and adjusted survival analysis between demographic, clinical variables, and frailty with time from hospital admission to discharge or death, among patients. Variables such as age and gender were associated significantly (P<0.001). Hence, older age and male sex increased the risk of mortality. In contrast, previous admissions were not associated with mortality.
Sex, place of residence, did not differ significantly between survivors and non-survivors cases. However, compared to survivors of COVID-19, non-survivors were significantly older. Baseline hemoglobin, white blood cell, platelet, or 25- hydroxyvitamin D levels were not significantly different.
Duration of hospitalization tended to be shorter in those who died (P>0.05).
Most non-survivor patients were admitted to the ICU. So that, the hazard ratio for mortality was significantly higher in patients requiring ICU admission (P<0.0001) (Figures 1 and 2).
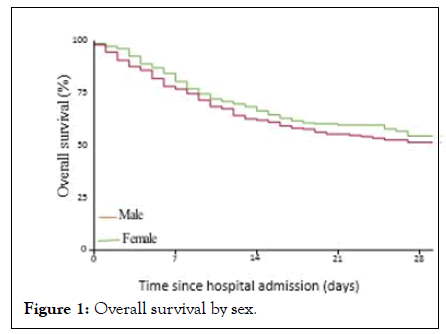
Figure 1: Overall survival by sex.
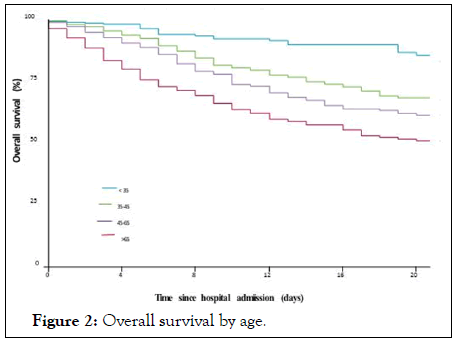
Figure 2: Overall survival by age.
This study was designed to provide evidence on the effect of frailty in hospitalized COVID-19 patients. We confirmed that age and male sex were associated with an increased risk of mortality. Generally, we conducted this study to examine the association between frailty and severe disease. We found that frailty has an effective factor for survival time among COVID-19 patients. This finding suggests the optimum treatment strategy in advance for older COVID-19 patients. Since the epidemic of COVID-19, much literature has reported that older age was correlated with ARDS after being infected [15].
Mortality in our population was 17·2%, which is in line with current mortality estimates for COVID-19 globally. A study recently showed a mortality rate of 26% in a large UK study [16]. These data also show that frailty helps to predict the hazard of death in COVID-19 patients, similar to in other diseases.
Here, we fitted the CPH and frailty Cox models to estimate the adjusted hazard of COVID-19 hospitalized patients. Our results showed that a higher age group has a direct effect on the hazard of death. These results are consistent with another study [17]. The present study was performed during three months of followup. The significant variables in the CPH model including comorbidity, sex, smoking status, and age groups. In the current study, the gamma-frailty Cox model was fitted to the COVID-19 patients. The findings represent that the increased mortality associated with increased C-reactive protein levels and prevalence of comorbidities (hypertension, diabetes) are also in line with other estimates, suggesting that our data are comparable with other populations [18,19]. It is unfortunate that because of the constraints of the pandemic, we were unable to rapidly collect more clinical data. We purposely focused only on the main variables in the study to get fast reporting of the frailty effect. Additionally, as COVID-19 data become more available rapidly, it was being shown that comorbidities have increasing importance, so these additional data would have added value to the manuscript but were not available at the time of data collection.
However, we carefully prepared this study, but it felt some limitations. First, hormonal factors have not been considered as important factors on the hazard. Second, there are missing observations in some of the recorded factors. It is possible that inaccuracies may have occurred during data collection; although, our research team is experienced in collecting data. Another limitation of this study is that only admitted hospital patients were included. This criterion will have excluded other patients that were died in emergency departments or discharged, and also cases who did not present to secondary care. Therefore, these results are only generalizable to an inpatient population. The current study aimed to assess the effect of frailty on death hazard in patients of all ages with COVID-19 showed that considering frailty in the model increases the hazard of mortality, even after accounting for variables such as age and other known comorbidities linked to COVID-19.
The findings show the importance of frailty assessment, rather than age, in combination with other measures in the context of COVID-19.
These findings also show that frailty can help to predict the hazard of death in COVID-19 patients accurately [10,19].our major purpose was to provide evidence to help clinicians about the proper allocation of health-care resources in the COVID-19 pandemic. Increasing age has been associated with COVID-19 mortality previously. Our study expresses a relationship between frailty and mortality in older patients. This finding is in line with previous studies, showing an association between frailty and non-COVID mortality as well as among older hospitalized adults.
As the results of the frailty model were shown, it can be concluded that accounting for latent variables including genetic factors and environmental, can increase the efficacy of the predictive analysis. Also, using a more advanced statistical model that considers the role of latent variables can lead to reducing the hazard of mortality which highlights the screening role. Frailty is associated with COVID-19 mortality in older hospitalized patients. Increasing age, male sex, and comorbidities are also associated with increased death hazard. Although, we feel that it can be useful, in conjunction with other prognostic markers regarding clinical management decisions.
Ethics approval and consent to participate
All procedures in this study were approved by the ethics board committee of Birjand University of Medical Sciences, reference number: IR.BUMS.REC.1399.185 and consent to participate is not applicable
Not applicable
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
MZ and FO designed the experiments. FO collected data and performed the statistical analyses and wrote the results section. FO interpreted the results. FO wrote the initial manuscript. MZ critically reviewed and modified the manuscript. Both authors approved the final manuscript.
We would like to thank all the students for their participation.
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
Citation: Battino E (2022) Survival Analysis of COVID-19 Patients using Cox Frailty Model. Intern Med. 12:358.
Received: 03-Jan-2022, Manuscript No. IME-21-358; Editor assigned: 05-Jan-2022, Pre QC No. IME-21-358 (PQ); Reviewed: 19-Jan-2022, QC No. IME-21-358; Revised: 24-Jan-2022, Manuscript No. IME-21-358 (R); Published: 31-Jan-2022 , DOI: 10.35248/2165-8048.22.12.358
Copyright: © 2022 Battino E. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.