Internal Medicine
Open Access
ISSN: 2165-8048
ISSN: 2165-8048
Research Article - (2021)
Objective: To analyze the results of five years of In Vitro Fertilization (IVF) practice in the medically assisted procreation unit of the gynecology department of the Center Hospitalize du Pays d´Aix.
Materials and methods: This was a retrospective study for descriptive and analytical purposes covering a period of five years from January 1, 2014 to December 31, 2018. It focused on patients treated for In Vitro Fertilization (IVF) in the unit of medically assisted procreation of the gynecology department of the Center Hospitalier du Pays d'Aix.
Result: At the end of this study, the data completion rate was on average 94%. The mean age of the patients was 35 years with extremes of 25 years and 44 years. This was a generally non-smoking (76.7%) and 90.1% non-obese population. Infertility was secondary in 58% of cases. Male causes accounted for 22% of the indications for In Vitro Fertilization (IVF). With regard to female infertility, there is a homogeneous distribution between endometriosis (27%), tubal (21%), cervical (18%), ovulatory (18%) and unexplained (21%) causes. The main prognostic factor turned out to be age.
Conclusion: Infertility is a couple's business, not just a woman. Our study showed that age was the main prognostic factor influencing the outcome of In Vitro Fertilization (IVF) with a decrease in the chances of success with increased age.
Fertilization; Procreation; Infertility; Prognosis
The couple's infertility is a public health problem. In France, the percentage of couples without pregnancy after one year without contraception is between 15 and 25% [1]. The causes of the couple's infertility are numerous and can be caused by either the man and woman or sometimes both [2]. Its management uses the medical and surgical means based on infertility therapy [3,4]. However, in some cases, the use of medical assistance through Artificial Insemination (AI) or In Vitro Fertilization (IVF) and Embryo Transfer (FIVETE) or Intra Cytoplasmic Sperm Injection (ICSI) may be necessary [5]. The Hospital Center of Pays d'Aix is one of the major centers in the practice of medically assisted reproduction. The evaluation of the practice of In Vitro Fertilization (IVF) and embryo transfer over the last 5 years led us to carry out this study with the following hypothesis: The results of IVF are satisfactory at the Pays d'Aix Hospital Center. The objectives were to determine the factors influencing the outcome of IVF in the medically assisted procreation unit of the gynecology department of the Hospital Centre of Pays d'Aix.
This was a cross-sectional study with descriptive and analytical aim with retrospective data collection over a 5-year period from January 1, 2014 to December 31, 2018. All couples treated for infertility and having undergone at least one IVF procedure during the study period were included in the study. The variables studied were: Age, occupation, marital status, duration of infertility, medical-surgical history, physical examination data, stimulation protocol, puncture, number of embryos, number of attempts, IVF outcome, pregnancy with live birth, pregnancy without live birth, procedure failure. The data was entered using Excel 2019 software. Data processing and analysis was done with SPSS 16.0 data management and statistics software.
A total of 1463 files were exploited with 3480 cycles or on average 2.38 file cycles. The distribution of cycles according to the age of the patients is presented in Table 1.
| Age | Cycles | Known results | Percentage (%) |
|---|---|---|---|
| <30 | 354 | 353 | 14 |
| 30-34 | 720 | 717 | 29 |
| 35-37 | 503 | 499 | 20 |
| 38-39 | 310 | 308 | 12 |
| 40-41 | 320 | 319 | 13 |
| ≥ 42 | 294 | 292 | 12 |
| Total | 2501 | 2488 | 100 |
| ≥ 40 | 614 | 611 | 25 |
Table 1: Age distribution of cycles.
The average age of the patients was 35 years with extremes ranging from 25 years to 44 years. All patients were nulliparous. The percentage of primary cycles was 42% compared to 59% for the secondary cycle of infertility. The distribution of cycles according to the etiology of infertility is shown in Table 2, below:
| Etiologies | N | Percentage (%) |
|---|---|---|
| Masculine | 777 | 22 |
| Pure Tubal | 744 | 21 |
| Unexplained | 745 | 21 |
| Endometriosis | 928 | 27 |
| Ovulatory | 621 | 18 |
| Cervical | 621 | 18 |
Table 2: Distribution of cycles according to the etiology of infertility.
Following the stimulation protocols the antagonist was performed in 50%, the long antagonist delay in 17%, the long daily antagonist in 30%, the short in 4% and spontaneous stimulation in 0%. High pregnancy rates per cycle were found in young subjects with 28.8% in subjects fewer than 30 years of age and gradually decreased to 4.4% in subjects over 42 years of age. The same observation was made with regard to the distribution of pregnancies by age and the rate of pregnancy by transfer by age. Indeed, the highest rate of pregnancy by age was observed in subjects under 30 years of age (32.8%) and gradually decreased to 5.3% in subjects over 42 years of age. The agespecific risk of miscarriage was higher in older women. 34% for subjects over 40 years of age compared to 5% for subjects under 5%. The pregnancy rate by gesture was primary in 17% of cases and secondary in 21% cases. Taking into account whether or not smoking, no significant differences were found in the pregnancy rate. This rate was 18% in both smoking and non-smoking subjects. The same is true for the number of pregnancies by transfer (15%) or puncture (29%).
No significant difference was found in the pregnancy rate per cycle regardless of the patients' body mass index. The finding was the same when taking into account the number of pregnancies by puncture or transfer. The pregnancy rate was significantly higher in the transfer group regardless of the stimulation protocol used compared to the puncture group. However, regardless of the group, the pregnancy percentage for the spontaneous stimulation protocol was zero. Table 3 shows the general influence of WHA on IVF outcome.
| AMH | N=1335 | G | G/c | G/p | G/t | |
|---|---|---|---|---|---|---|
| <0.5 | 151 | 12 | 8% | 11% | 17% | |
| 0.5-1 | 80 | 23 | 13% | 13% | 23% | p=0.15 |
| >1-3 | 515 | 88 | 17% | 14% | 25% | p=0.17 |
| ≥ 3 | 489 | 125 | 26% | 29% | 38% | p=0.00 |
Table 3: General impact of AMH on IVF outcome.
The cancellation rate per cycle according to the AMH is shown in Figure 1.
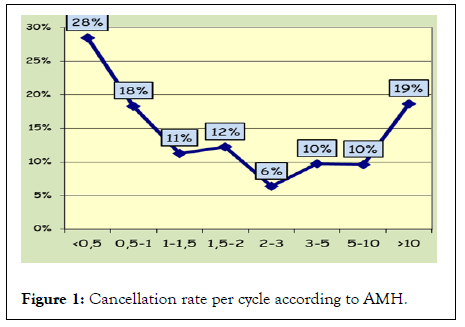
Figure 1: Cancellation rate per cycle according to AMH.
The pregnancy rate per cycle as a function of THE AMH is shown in Figure 2 below.
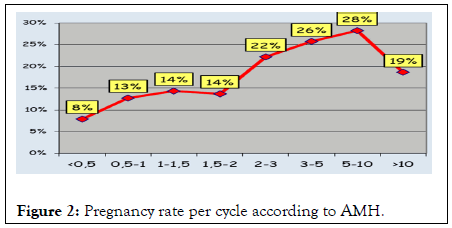
Figure 2: Pregnancy rate per cycle according to AMH.
The impact of the FSH threshold measured at the third day on IVF outcome is presented in Table 4 below:
| FSH A J3 | N=1989 | G | G/c | G/p | G/t | |
|---|---|---|---|---|---|---|
| <3 | 15 | 3 | 20% | 14% | 21% | p=1.00 |
| 3 A 10 | 1747 | 350 | 20% | 16% | 20% | |
| >10 | 227 | 26 | 11% | 13% | 19% | p=0.002 |
Table 4: FSH impact on IVF outcome.
The outcome of IVF following the existence or absence of a uterine abnormality is presented in Table 5.
| N=2663 | GC | G | FCS | |
| Normal Uterus | 2368 | 468 | 388 | 62 |
| 20% | 16% | 13% | ||
| Uterine Abnormality | 295 | 43 | 33 | 9 |
| 15% | 11% | 21% | ||
| p=0.02 | p=0.001 | p=0.163 |
Table 5: IVF outcome following uterine abnormality.
Figure 3, below shows the pregnancy rate by transfer according to endometrial thickness.
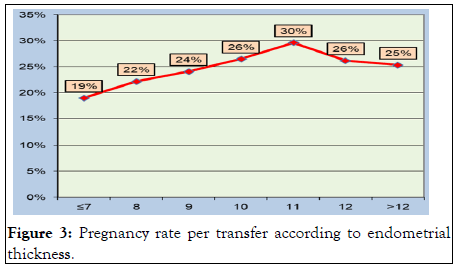
Figure 3: Pregnancy rate per transfer according to endometrial thickness.
The distribution of embryo transfers by day of transfer is shown in Figure 4.
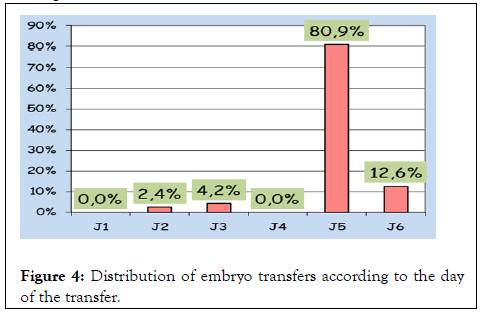
Figure 4: Distribution of embryo transfers according to the day of the transfer.
The rate of progressive pregnancy following the day of embryo transfer is shown in Figure 5.
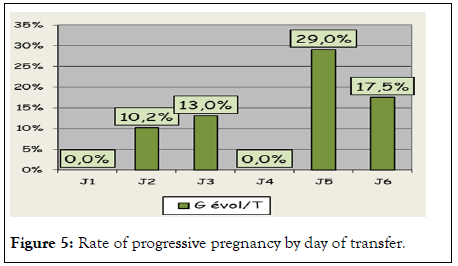
Figure 5: Rate of progressive pregnancy by day of transfer.
The fate of pregnancies after IVF is presented in Table 6.
| G | AACHT | G E | GA | GEU | IMG | |
|---|---|---|---|---|---|---|
| fresh e | 87 | 0 | 1 | 64 | 9 | 13 |
| 0.0% | 1.1% | 73.6% | 10.3% | 14.9% | ||
| frozen e | 138 | 109 | 0 | 21 | 6 | 2 |
| 79.0% | 0.0% | 15.2% | 4.3% | 1.4% | ||
| total | 677 | 570 | 1 | 85 | 15 | |
| 84.2% | 0.1% | 12.6% | 2.2% |
Table 6: Becoming pregnancies after IVF.
The majority of women in our study were over the age of 30. This is the age where fertility decreases and hopes of spontaneous pregnancy dwindle. The use of In Vitro Fertilization (IVF) is therefore essential [6]. In our study, most of the patients were non-smokers. This augurs a priori a good prognosis because the decrease in natural fertility is dose-dependent since it decreases sharply beyond 10 to 15 cigarettes per day and duration-dependent (even more beyond five years of active smoking [7,8]. There is an increase in the time to conception in case of active and passive smoking, as well as a decrease in ovarian reserve [9], but smoking-related variations were not statistically significant in our study. This could be related to the small sample size. In our study, only 9.9% of patients were obese or underweight. This is a factor that a priori augurs a good prognosis. Obesity increases the risk of infertility and menstrual disorders, especially if it is android obesity [10,11]. In 58% of the cases in our study, it was a secondary infertility with a female etiology found in 78% of cases. A male cause was found in 22% of cases or one in five couples. This is to say once again that a parental project is a couple's story. These data are similar to those in the literature which estimate the rate of male infertility between 20 and 40%. With regard to female infertility, there is a homogeneous distribution between endometriosis (27%), tubal (21%), cervical (18%), ovulatory (18%) and unexplained (21%) causes; with a small prevalence for endometriosis [12].
It has been found in the literature a gradual decrease in fecund ability from the age of 30, then quickly after 35 years to become almost zero at age 45. These data were observed in natural fertility, donor sperm insemination and In Vitro Fertilization (IVF) [13,14]. These data are similar to those revealed by our study. We have seen a general decline in pregnancy rates based on age.
The mechanisms involved involve a decrease in oocyte quantity [15,16]. Thus, in our study we note a gradual fall of the antimullerian hormone with the progression of age. The anti mullerian hormone is indeed a good reflection of the ovarian reserve. Its decline reflects a decrease in the chances of pregnancy. Other mechanisms are also implicated such as an increase in the rate of aneuploidy, a longer duration of exposure to environmental factors and infections, and a greater frequency of genital pathologies [17]. Obesity in our study did not significantly influence the outcome of In Vitro Fertilization (IVF).
The ovarian reserve was evaluated in our study by the determination of the level of AMH and FSH on Day 3. It made it possible to report a decrease in the chances of success with a decrease in the ovarian reserve. Indeed, an increase in FSH or a decrease in AMH has been associated with a decrease in pregnancy rates. In the literature it is accepted that a decrease in ovarian reserve is associated with a poor response to stimulation [18].
The appearance of the uterus influenced in this study the outcome of In Vitro Fertilization (IVF), including the condition of the endometrium at the time of transfer. All transfers were performed in our study on an endometrium at least 7 mm thick. There is usually an increase in the chances of pregnancy with the increase in the thickness of the endometrium. Endometrial thickness therefore influences embryo implantation [19,20].
The literature reports that an endometrial thickness of less than 7 mm significantly reduces embryo implantation. In addition, embryo implantation seems all the weaker as the endometrium is hyperechoic. Our study showed that age was the main prognostic factor influencing the outcome of In Vitro Fertilization (IVF) with a decrease in the chances of success with increasing age. To this is added the ovarian reserve, the thickness of the endometrium and the transfer of the embryo on the 5th day.
Citation: Tognifode MV, Aboubakar M, Coovi FMB, Hounkponou NFM, Lokossou S, Dangbemey P, et al. (2021) Study of the Factors Influencing the Outcome of In Vitro Fecondation (IVF) at the Pays D'aix Hospital Centre. Intern Med. S9:002.
Received: 08-Dec-2021 Accepted: 22-Dec-2021 Published: 29-Dec-2021
Copyright: © 2021 Tognifode MV, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : no