
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Case Report - (2023)Volume 13, Issue 3
Baclofen, a derivative of the neurotransmitter γ-aminobutyric acid, is widely used to treat adjuvant pain and skeletal muscle spasms. Common side effects of baclofen can cause dizziness, drowsiness, or weakness, in addition to serious central nervous system problems such as loss of brain stem reflex, comatose mentality, myoclonic jerk, and seizures. Several cases have reported that baclofen intoxication is provoked by high overdose ingestion in a short period. We report two cases of serial EEG changes in low-dose baclofen intoxication that showed burst and suppression patterns and eventually returned to normal EEG in correlation with clinical improvement.
Baclofen; Burst and suppression; Drug intoxication; Dizziness; Drowsiness
Baclofen is a chemical derivative of the neurotransmitter γ-Aminobutyric Acid (GABA), which acts as a central nervous system depressant, GABA agonist, and muscle relaxant. It is a lipophilic drug that easily crosses the blood-brain barrier and acts as a presynaptic inhibitor by activating the GABA-B receptor. Baclofen is usually used to relieve spastic movement disorders, cramping, or tightness caused by cerebral palsy, spinal cord injury, motor neuron disease, or multiple sclerosis [1]. Although many patients have no adverse drug reactions, some may have general weakness, dizziness, delirium, bradycardia, sedation, and even a comatose mentality with loss of brainstem reflex. Serious side effects such as generalized tonic-clonic seizure and non-convulsive status epilepticus can also occur, especially when ingested with a high overdose within a short period. Several showed comatose mentality, and Generalized Tonic-Clonic (GTC) seizures reached beyond the therapeutic level by baclofen uptake in a short time. We report two cases of abrupt altered mentality accompanied by specific electroencephalography changes who took low-dose baclofen for several months [2].
Case 1: A 77-year-old woman visited the emergency room because of a loss of consciousness. On admission, she had been harvesting parsley water at work. After working for 5 h, she suddenly fell with an altered mentality while experiencing nausea, vomiting, and dizziness. The patient had been taking antihypertensive and diabetic medications for approximately 15 years, and baclofen 10 mg, eperisone 100 mg (50 mg twice a day), pregabalin 25 mg, acetaminophen 162.5 mg, tramadol hydrochloride 18.75 mg, and aceclofenac 100 mg for muscle pain for 3 months before the visit. Her vital signs were as follows: Blood pressure, 200/90 mmHg; heart rate, 70 beats/min; respiratory rate, 20 beats/min; and body temperature, 36.8°C. The neurological evaluation indicated that the patient was in a stupor and showed a withdrawal pattern under pain. The pupil light, corneal, and oculocephalic reflexes revealed normal responses without pathologic reflexes. Blood sodium concentration was 134 mmol/L, blood glucose was 245 mg/dL, and glycated Hemoglobin (HbA1C) was 5.6%. The creatinine in the blood was 1.53 mg/dL, and the Glomerular Filtration Rate (eGFR) was 32.8 ml/min. The results of the other electrolyte and blood tests were normal, and there were no specific findings in the urine test. The only abnormalities in the computed tomography angiography and perfusion were stenosis of the left vertebral artery and the left posterior cerebral artery. Additional Magnetic Resonance Imaging (MRI), including Diffusion Weighted Imaging (DWI), did not reveal any changes or signs of contrast medium enhancement [3]. In the cerebrospinal fluid study, only the protein increased to 49.4 mg/dL, and no other inflammatory findings were observed. Her drug screen tests on 230 drugs, 260 pesticides, and other natural poisons were performed and found a positive toxic level for baclofen (3.5 mcg/mL, normal range: 0.08-0.60). EEG was performed three hours after admission and showed high amplitude of 3 Hz-4 Hz epileptiform burst and attenuation patterns. On the second day of hospitalization, the consciousness level deteriorated further to a semi-coma state, and the patient did not show any eye response to pain stimulation. Neither upper extremity responded to external stimuli, nor only the lower extremities showed mild flexion responses. EEG was conducted to reveal a burst and suppression pattern throughout the background. The patient discontinued all medications, and the patient’s progress was monitored under hydration and supportive management. On the seventh day after discontinuing baclofen, her consciousness improved to an alert state and she showed proper orientation toward people and places. The muscle strength of both upper and lower extremities was MRC grade 4. Follow-up EEG revealed that the burst and suppression found in the previous EEG had disappeared, and the patient’s condition improved to increased background activity with an overall alpha rhythm of 8 Hz-9 Hz (Figure 1) [4].
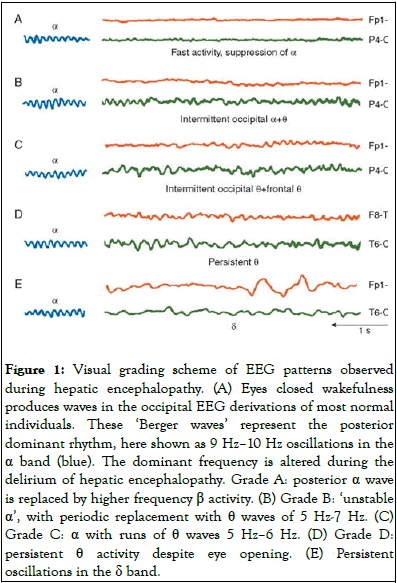
Figure 1: Visual grading scheme of EEG patterns observed during hepatic encephalopathy. (A) Eyes closed wakefulness produces waves in the occipital EEG derivations of most normal individuals. These ‘Berger waves’ represent the posterior dominant rhythm, here shown as 9 Hz–10 Hz oscillations in the α band (blue). The dominant frequency is altered during the delirium of hepatic encephalopathy. Grade A: posterior α wave is replaced by higher frequency β activity. (B) Grade B: ‘unstable α’, with periodic replacement with θ waves of 5 Hz-7 Hz. (C) Grade C: α with runs of θ waves 5 Hz–6 Hz. (D) Grade D: persistent θ activity despite eye opening. (E) Persistent oscillations in the δ band.
Case 2: A 40-year-old woman visited the emergency room with generalized tonic-clonic seizures and mental deterioration. Since she had a chronic headache, she took baclofen 10 mg, afloqualone 10 mg, dexibuprofen 400 mg twice a day and amitriptyline 5 mg once a day without a specific medical history. She talked to her husband over the phone 15 h before admission and complained of a severe headache. However, she could engage in normal conversations [5]. When her caregiver came home ten hours before her admission to see that she was lying in bed, the caregiver thought she was sleeping and did not wake her up. Three hours before her admission, the caregiver discovered that the patient had a sudden onset of seizures and dyspnea and took her to the emergency room. At the time of admission, blood pressure was 105/55 mmHg, pulse rate was 80 beats/min, respiration rate was 20 breaths/min, and body temperature was 37.1°C. Two GTC seizures occurred immediately after admission, and each seizure persisted for approximately 10 seconds. On neurological examination, her consciousness level was a coma, and she did not respond to light reflex, corneal reflex, and oculocephalic reflex; she did not show eye response, verbal response, or motor response to external pain stimuli, and did not have pathologic reflexes, such as Babinski sign and ankle clonus. The results of the diagnosis basic blood test, chemistry examination, and blood gas examination showed that CK and lactate increased to 549 U/L and 5.4 mmol/L, respectively, while eGFR, and including electrolyte 91.1 ml/min and creatinine were 0.81 mg/dL, which were normal. The patient’s blood glucose level was 127 mg/dL. The computed tomography, angiography, and perfusion results were normal, and MRI did not show any abnormalities. In the CSF study, ICP was elevated to 256 mm H2O, but white blood cells and red blood cells were not detected, and protein (43.7 mg/dL) and glucose (64 mg/dL) were within the normal range [6].
This study conducted a poison test on 230 drugs, 260 pesticides, and other natural poisons regarding the possibility of drug intoxication by requesting it from the poisoning analysis lab. The blood drug concentration test results showed that baclofen was 5.747 mcg/mL (normal range: 0.08-0.6). Hydration and supportive management were administered to the patient as initial treatment, and progress was monitored. On the first day of admission, she was in a coma state with no response to light reflex, corneal reflex, oculocephalic reflex, and noxious stimuli. EEG was conducted to check the patient's brain function. A 1 Hz-2 Hz burst and suppression pattern was confirmed. On the 4th day of admission, the level of consciousness was restored to a drowsy state, the patient showed a normal response to the brainstem reflex, and the muscle strength of the patient recovered to MRC grade 4. The patient responded appropriately to questions related to the time, place, and person. As the patient's level of consciousness improved, a follow-up EEG was performed on the 4th day of admission to confirm that the patient showed a normal response with an overall beta rhythm of 14 Hz-15 Hz. The patient’s condition improved and she was discharged on the 8th day of admission [7].
Orally administered baclofen is rapidly absorbed in the gastrointestinal tract, and its serum concentration reaches its highest level between 45 minutes and 2.5 hours with a half-life of 3.5 hours. Acute baclofen intoxication can occur when taking 200 mg or more within a short period [8]. Various side effects, including mental deterioration, seizures, hypopnea, hypotension, hypothermia, and hypotension, have been reported. As drug elimination consists of approximately 15% metabolized by the liver and 85% excreted through the kidneys, patients with renal dysfunction might have more toxic adverse effects. Previous case studies on baclofen intoxication reported that taking a large amount of baclofen over a short period could cause acute intoxication symptoms, such as mental deterioration and seizures, and patients on dialysis showed acute intoxication even with a low dose of baclofen. In this case study, both patients were administered a relatively low dose of baclofen (10 mg twice daily) at admission. Even though the baclofen dosage was low, and the patients’ initial symptoms were headaches, their neurological symptoms deteriorated to a coma state within several hours [9]. Both patients recovered their mental status within seven days because the causative medication was withdrawn. Three cases of low-dose baclofen intoxication have been reported previously, and they were taking the drug in a range of 10 mg-40 mg and showed acute altered mentality within seven days. All of them had kidney problems, including one patient diagnosed with CKD after left nephrectomy for cancer and two patients with end-stage renal disease receiving hemodialysis three times per week. Unlike the three previous cases, our patients required more than 2.5 months for sudden altered mentality with low-dose baclofen (20 mg). It is unclear what mechanism caused patients’ mentality, even with low-dose baclofen, for a long period. In the first case, it was estimated that baclofen was beyond the toxic level, and old age with newly diagnosed CKD might have contributed to the deteriorated mentality. The second patient was taking afloqualone in addition to baclofen, and both of which are known as gaba receptor agonists. There has been a case of seizure in a 3-year-old girl who received an overdose of afloqualone. Although the second patient was younger than the first patient and had no specific underlying diseases, the two medications taken for a long period might have led to seizures and confusion. The first patient took three more days to recover alert mentality than the second patient, which may be due to the advanced age and newly found kidney disease. According to the blood test results on admission, the first patient was diagnosed with CKD 3b [10].
We had the opportunity to perform serial EEG to evaluate comatose mentality because there was a time interval to receive the drug screen results. Both patients in this case study showed a B-S EEG pattern. The first patient underwent EEG three times. EEG on the first and second days showed a burst and suppression pattern (B-S pattern) when she was in a stuporous state. On the seventh day of admission, the background rhythm recovered without a B-S pattern, and her neurological symptoms also improved with alert mentality. The second patient also showed a B-S pattern of EEG on the day of admission, which was normal after 3 days with clinical improvement. Known causes of a B-S pattern in EEG include space-occupying lesions, toxic metabolic factors, infection, brain trauma, stroke, coma due to hypoxic brain damage, general anesthesia, halogenated ethers, barbiturates, propofol, etomidate, NMDA receptor antagonists during gabaergic anesthesia, ohtahara syndrome, epilepsy syndromes such as early myoclonus encephalopathy, and hypothermia. A suggested mechanism of a B-S pattern in EEG was that baclofen binds to both postsynaptic and presynaptic inhibitory interneurons to inactivate them, which could excite the neuronal balance and cause a seizure. Patients with a B-S pattern show different prognoses depending on the cause. It is known that when it is medically induced in patients, the prognosis of a B-S pattern is good, while when it is due to a critical illness or hypoxic brain damage, it is poor. The favorable outcomes of our patients can be explained by previous literature. When the first EEG was taken in two patients, we correlated the B-S EEG pattern with their stuporous mental status. After stopping baclofen, the B-S pattern disappeared, and the background was restored in the EEG over time. Although a low dose of baclofen was administered for several months, we confirmed the possibility of acute intoxication with a low dose of baclofen and a clear correlation between EEG findings and the patients’ clinical condition [11].
This case highlights to diagnose critical illnesses caused by baclofen by examining detailed neurological symptoms and medical history. When baclofen was administered for a long time, even at a low dose, the patient could reach an acute comatose state and show a B-S pattern on EEG. Comatose patients with a B-S pattern on EEG without a clear medical history should consider not only a critical illness condition such as cardiac arrest or hypoxic brain damage but also drug intoxication.
Written informed consent was obtained from the patient for publication of this case report and the accompanying images.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
All data and material supporting our findings are contained within the manuscript.
Hyun Goo Kang is as a member of the editorial board (associate editor) of this journal.
The present study was supported by grants from the Clinical Medicine Research Institute at Jeonbuk national university hospital (2022).
Research design: H.J.K., B.S.S. and H.U.R; Data collection and analysis: H.J.K., H.G.K. and H.U.R; Computational studies and manuscript writing, H.J.K., H.G.K., B.S.S. and H.U.R. All authors have read and approved the final manuscript.
None
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ryu HU, Kim HJ, Kang HG, Shin BS (2023) Serial EEG changes in low-Dose Baclofen Intoxication. J Clin Toxicol. 13:536.
Received: 12-Jan-2023, Manuscript No. JCT-23-21381; Editor assigned: 16-Jan-2023, Pre QC No. JCT-23-21381 (PQ); Reviewed: 30-Jan-2023, QC No. JCT-23-21381; Revised: 30-Mar-2023, Manuscript No. JCT-23-21381 (R); Published: 06-Apr-2023 , DOI: 10.35248/2161-0495.23.13.536
Copyright: © 2023 Ryu HU, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.