Journal of Thyroid Disorders & Therapy
Open Access
ISSN: 2167-7948
ISSN: 2167-7948
Case Report - (2020)Volume 9, Issue 1
Graves’ disease is an autoimmune disease of the thyroid gland which results from production of thyroid stimulating immunoglobulins-TSI. These thyroid stimulating immunoglobulins bind to the thyroid stimulating hormone-TSH. This leads to overproduction of thyroid hormones, necessitating excessive functions of these hormones in the body. The commonest presentation is features of hyperthyroidism, occasionally with extra thyroidal features. Graves’ disease is rare in children and adolescents, greater numbers are seen in adults, between fifth and sixth decades of life. We report a case of 19-year-old girl who presented with anterior neck swelling of two years, associated with features of hyperthyroidism and ophthalmopathy which were present at onset. Prior to presentation had received anti thyroid treatments with drugs and radioiodine ablation one year ago and refractory to above treatment. Investigations showed raised thyroxine, tri-iodothyronine, reduced thyroid stimulating hormone and markedly raised thyroid antibody. Thyroid ultrasound showed enlargement of both lobes and isthmus with lobulated outlines, echotexture and heterogenous fibrous bands. She was treated by endoscopic total thyroidectomy (Bilateral axillary and breast approach) without postoperative complication and had since remained euthyroid with good cosmetic outcome. She is currently on outpatient follow up. Graves’ disease in teen age with ophtalmopathy is rare, and refractory with medical and RAI therapy. This can be well managed endoscopically in expert hands.
Graves’ disease ophthalmopathy; Teen age; Endoscopic thyroidectomy
Graves’ disease is an autoimmune disease of the thyroid gland which results from production of thyroid stimulating immunoglobulins-TSI [1]. These thyroid stimulating immunoglobulins bind to the thyroid stimulating hormone-TSH [1]. This leads to overproduction of thyroid hormones, necessitating excessive functions of these hormones in the body. The commonest presentation is features of hyperthyroidism, occasionally with extra thyroidal features [2]. Graves’ disease is rare in children and adolescents, greater numbers are seen in adults, between fifth and sixth decades of life [1,2].
A 19-year-old girl presented with anterior neck swelling of two years. Swelling was not painful, associated with features of hyperthyroidism (heat intolerance, weight loss despite good appetite, tremor and excessive sweating) and eye protrusion from onset. There was no history suggestive of hypothyroidism (weight gain, menorrhagia) and no associated obstructed symptoms. Prior to onset of her symptoms there was no history of neck irradiation, mother had hypothyroidism. Since onset, there was no cough, bone pain and jaundice. For the above complaints, she had received anti thyroid treatments with tablet neomercazole and radioiodine ablation one year ago and refractory to the above treatment (Figures 1-4).
Figure 1: Physical examination.
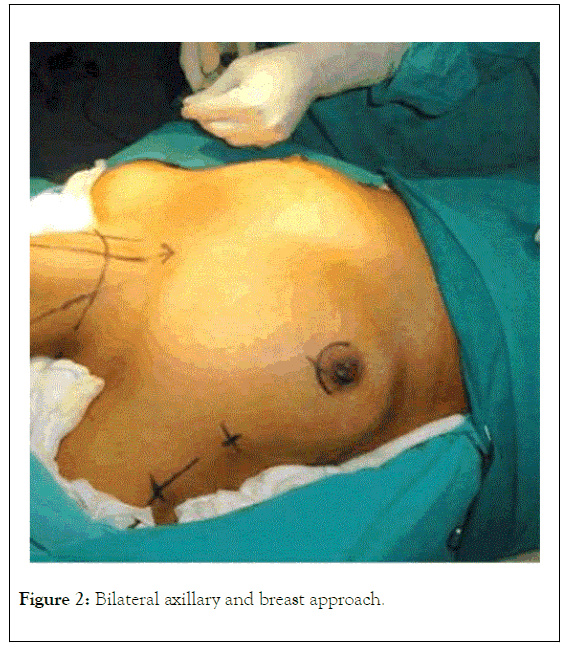
Figure 2: Bilateral axillary and breast approach.
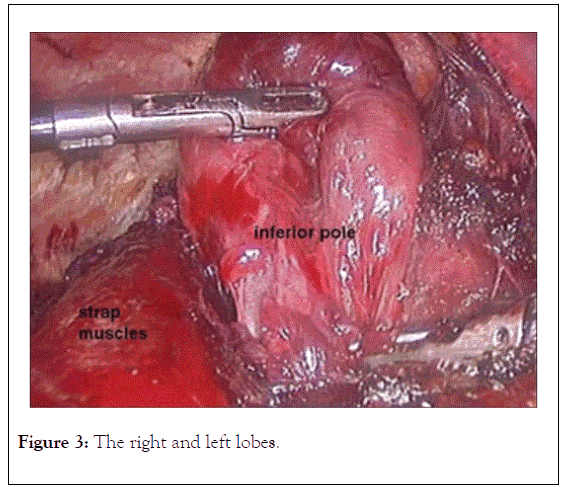
Figure 3: The right and left lobes.
Figure 4: Histopathology findings.
Examination findings were blood pressure of 120/80 mmHg; pulse rate-92/min, sleeping pulse- 90/min, exophthalmos 29 mm and 28 mm. There was a globular mass in front of the neck, measured 4 × 4 cm moved upward with deglutition, defined borders, nodular surface, firm; trachea was mildly deviated to the right, bilateral carotids felt and no cervical lymphadenopathy.
Investigations showed raised thyroxine 320.7 pmol/L triiodothyronine >10, reduced thyroid stimulating hormone 0.01 miu/l and markedly raised thyroid antibody >40IU/L. Thyroid ultrasound showed enlargement of both lobes and isthmus with lobulated outlines, echotexture and heterogenous fibrous bands. She was treated by endoscopic total thyroidectomy (Bilateral axillary and breast approach.
Left lobe measured 6.5 × 3.5 × 3 cm. Outer surface was lobulated and cut surface showed multiple colloid filled nodules, largest nodule measuring 1 × 0.5 cm+pyramidal lobe measuring 3 × 0.5 cm.
Right lobe measured 6 × 3.5 × 3 cm, while attached isthmus measured 1 × 0.5 cm. Outer surface was lobulated and irregular and cut surface showed multiple colloid filled nodules, largest nodule measuring 0.5 × 0.5 cm.
On histopathology, the sections from right lobe, left lobe and isthmus show multiple nodules composed of variable sized thyroid follicles lined by flattened cells displaying bland chromatin and moderate amount of cytoplasm. Focal area of hyperplastic change seen. At few foci hemosiderin laden cystic macrophages are also seen. Normal thyroid parenchyma is also seen in intervening areas between nodules. The section from pyramidal lobe shows unremarkable thyroid parenchyma. There is no evidence of malignancy.
Graves’ disease is an autoimmune disorder that can present with both thyroidal and extra thyroidal features [2]. The genetics of Graves ’ disease is complex, more likely multifactorial [3]. Thyroid ophthalmopathy is one of the extrathyroidal features, which is an autoimmune disorder of the orbit and periorbital tissues seen with thyroid disease. The prevalence varies, Abraham R et al., reported 0.1-0.3% in India [4]. The diagnosis of Graves’ disease is clinical and this is confirmed by the raised anti thyroid antibody.
When Graves ’ disease occurs in adolescents, it should be considered a specific entity, different from Graves’ disease of adult onset. They are more refractory to medical treatment and require long-term protocol for remission [5].
The treatment options are the use of antithyroid drugs, radioactive iodine ablation and surgery. The treatment choice may differ from country to country but generally very few patients with uncomplicated Graves ’ disease are treated with surgery. The principle would involve control of symptoms, maintain euthyroid state, and minimize morbidity [4,6].
Graves’ ophthalmopathy is often resistant to or even aggravated by medical treatment and radioiodine ablation with unpredicted relapse rates [7].
The indication for surgery in Graves’ disease patients include very large glands, refractory to radioiodine, noncompliance to medications and presence of suspicious nodule [8,9]. Other indications include coexisting primary hyperparathyroidism, contraindication to antithyroid drugs and radioiodine and Graves ’ disease in pregnancy [9,10]. Definitive treatment is recommended in children and those with severe Graves’ ophthalmopathy [8]. Such patients can benefit from surgical treatment (total thyroidectomy) in the form of open or endoscopic thyroidectomy aimed at ablative strategy [11].
Surgery for Graves’ disease is usually performed after adequate medical control of symptoms of hyperthyroidism [9]. Total thyroidectomy is increasingly being used in the treatment of benign thyroid diseases including Graves ’ disease with a predictable outcome and lack of disease recurrence making it more advantageous [7].
Lowery and Kerin reported that there is increasing evidence that total thyroidectomy may have a beneficial effect in improving eye signs and symptoms in Graves’ ophthalmopathy [7].
Importantly, cosmesis is of utmost priority when toxicity and malignancy have been ruled out in any goiter. Zhang et al., in their work noted that endoscopic thyroidectomy provided a better cosmetic satisfaction, and less blood loss when compared with open thyroidectomy. They also stated, that endoscopic thyroidectomy is safe and feasible for patients with Graves ’ disease [12].
Surgery for Graves ’ disease is associated with complications which ranges from bleeding, recurrent laryngeal nerve palsy, hypocalcaemia and thyroid storm, the risk of these complications are higher in poorly controlled disease and low in centers with high volume of thyroidectomies [9,13]. Thus, recommendation for referral is necessary to those centers to minimize such risks.
In conclusion surgical treatment is underutilized in the treatment of Grave’s disease. Graves’ disease in teen age with ophtalmopathy is rare. When they occur, they are usually refractory with medical and RAI therapy. This can be well managed endoscopically in expert hands.
Citation: Chand G, Sunday-Nweke NA, Dhanda M (2020) Refractory Graves’ Disease with Ophthalmopathy in a 19-year Old Girl Managed Endoscopically: A Case Report. Thyroid Disorders Ther. 9:234. DOI: 10.35248/2167-7948.20.09.234
Received: 31-Jan-2020 Accepted: 21-Feb-2020 Published: 28-Feb-2020 , DOI: 10.35248/2167-7948.20.09.234
Copyright: © 2020 Chand G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.