Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Case Report - (2024)Volume 14, Issue 1
Mediastinal widening on chest radiography is a concerning sign in patients visiting the emergency room. Among young patients, the most common cause of mediastinal widening is that of a tumorous origin. Here we present the case of a 29-year-old woman who presented to the emergency room with a chief complaint of dry cough for 2 months. Chest radiography revealed mediastinal widening and bilateral pleural effusion. Contrast-enhanced computed tomography of the chest revealed a huge heterogeneous anterior mediastinal mass with hilar and subcarinal extension. The patient was admitted to the internal medicine ward and she underwent ultrasound-guided pleurocentesis. Pleural fluid analysis revealed an exudative characteristic; however, pleural fluid bacterial culture and tuberculosis culture were negative. The patient underwent excisional biopsy of the right neck lymph node, and the pathology report revealed diffused large size malignant lymphoid cell infiltration. Immunohistochemical staining revealed CD10-, CD20+++, Bcl-2+++, and ki67+ (>90%), thereby confirming the diagnosis of diffuse large B-cell lymphoma.
Emergency physicians are always aware of great vessel diseases in cases of newly found mediastinal widening. However, mediastinal masses should also be considered in the differential diagnosis. Diffuse large B-cell lymphoma is rarely observed in an emergency setting, especially in cases where patients present to the emergency room with an uncommon presentation of lymphoma. Early detection relies on a high level of clinical suspicion and accurate diagnosis is still based on the pathological morphology and immunophenotyping. However, a general work-up should be performed in the case of newly found mediastinal widening.
Mediastinal widening; Diffuse large B-cell lymphoma; Young woman; Atypical symptoms
Mediastinal widening is a concerning sign on chest radiography in patients visiting the emergency room. Among young patients, the most common cause of mediastinal widening is that of a tumorous origin [1]. Herein, we present the case of a woman who presented with a chief complaint of dry cough for 2 months and first-time mediastinal widening [2]. The final diagnosis was diffuse large B-cell lymphoma and the patient showed no classic “B” symptoms (i.e., fever, weight loss and night sweats).
A 29-year-old woman presented to the emergency room with dry cough for 2 months. She also reported progressive exertional dyspnea and orthopnea; however, there was no fever, night sweats, weight loss, rhinorrhea, sputum production, chest pain, abdominal pain or leg edema [3]. Physical examination revealed decreased breath sounds in the bilateral basal lung fields and the presence of a palpable lymph node in the right neck (Figure 1).
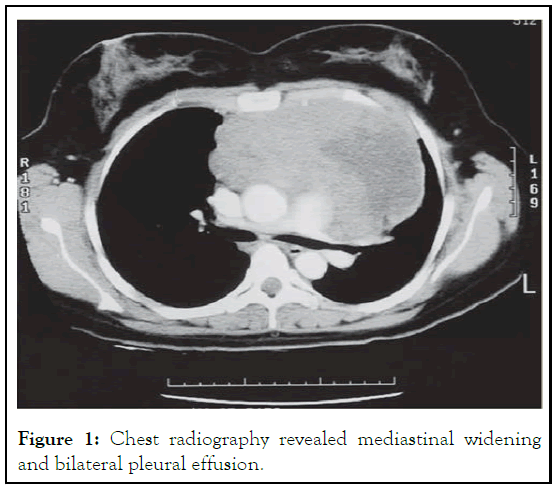
Figure 1: Chest radiography revealed mediastinal widening and bilateral pleural effusion.
The patient’s complete blood count revealed mild leukocytosis (white blood cell count, 10,780 cells/μL) without blast cells. Her biochemistry findings were unremarkable except for elevated lactic dehydrogenase levels of 372 IU/L (Figures 2-4) [4].
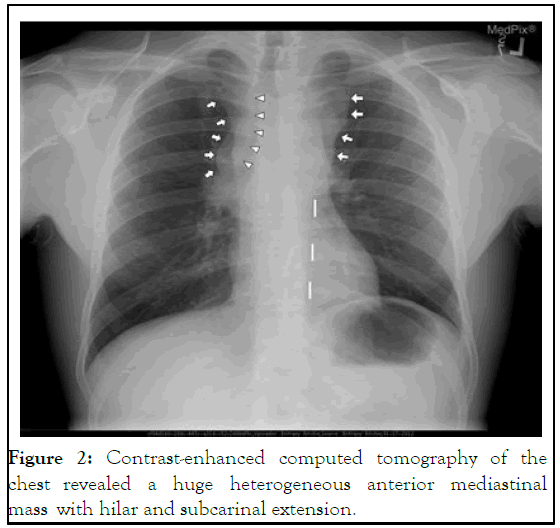
Figure 2: Contrast-enhanced computed tomography of the chest revealed a huge heterogeneous anterior mediastinal mass with hilar and subcarinal extension.
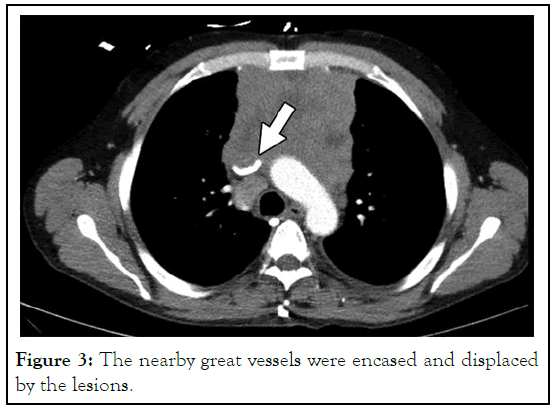
Figure 3: The nearby great vessels were encased and displaced by the lesions.
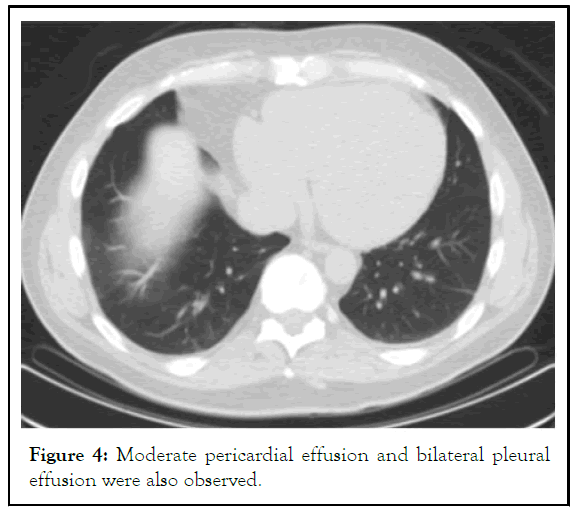
Figure 4: Moderate pericardial effusion and bilateral pleural effusion were also observed.
The patient was admitted to the internal medicine ward and she underwent ultrasound-guided pleurocentesis. Pleural fluid analysis revealed an exudative characteristic; however, pleural fluid bacterial culture and tuberculosis culture were negative. The patient underwent excisional biopsy of the right neck lymph node and the pathology report revealed diffuse large size malignant lymphoid cell infiltration [5]. Immunohistochemical staining revealed CD10-, CD20+++, Bcl-2+++, and ki67+ (>90%), which confirmed the diagnosis of diffuse large B-cell lymphoma. Positron emission tomography revealed Ann Arbor stage IV disease, with pleural, pericardial and bone marrow involvement. The international prognostic index score of this patient was 3. Therefore, she was referred to oncology department and she underwent combined intensive chemotherapy during hospitalization [6].
The m-BACOD regimen, which includes methotrexate, bleomycin, doxorubicin, cyclophosphamide, vincristine and dexamethasone was used. Rituximab, an anti-CD20 monoclonal antibody medicine, was added to the m-BACOD regimen to improve the complete response rate [7]. The patient had an uneventful treatment course during 6 cycles of chemotherapy, without the development of tumor lysis syndrome and follow-up positron emission tomography revealed no obvious fluorodeoxyglucose uptake lesion. She exhibited complete response after our treatment and no recurrence of disease was observed at the 6-month follow-up.
Mediastinal widening is defined as a mediastinal width of more than 6 cm on upright posterioanterior chest radiograph or 8 cm on anteroposterior chest radiograph at the level of the thoracic bulb [8]. When emergency physicians encounter patients with newly found mediastinal widening on chest radiography, they are always aware of the presence of great vessel diseases, such as aortic dissection and aortic stenosis, associated with ascending aorta dilatation. However, the main differential diagnosis of mediastinal widening is the presence of a tumor. The most common tumors that originate from the anterior mediastinum are teratoma, thyroid tumor, thymoma and lymphadenopathy (3T1L).
Diffuse large B-cell lymphoma is the most common subtype of non-Hodgkin lymphoma and has an annual incidence rate of approximately 7 cases per 100,000 individuals per year. Approximately 60% of the patients with diffuse large B-cell lymphoma are <60 years old. Asian patients have a lower incidence rate than caucasians, with a slight male predominance. Patients with diffuse large B-cell lymphoma usually present with rapidly enlarging lymph nodes in the neck, abdomen or mediastinum, similar to the symptoms in our patient. In addition, indirect symptoms resulting from external nodal compression, including cough, dyspnea, dysphagia, horner syndrome and superior vena cava syndrome, may develop. Only 30% of the population has the classic “B” symptoms, i.e., fever, weight loss and night sweats. Although imaging studies, such as computed tomography, can reveal disease severity, early detection primarily relies on a high level of clinical suspicion and accurate diagnosis is based on pathological morphology and immunophenotyping. The patient in our study did not experience chest pain or sharp back pain. Therefore, in such cases, physicians would presume a diagnosis of mediastinal widening with a tumorous origin. However, the patient in our study had atypical symptoms, such as cough, dyspnea and orthopnea, that may be attributable to pericardial effusion and pleural effusion [9].
Currently, the main regimen for diffuse large B-cell lymphoma treatment is the CHOP regimen (cyclophosphamide, doxorubicin, vincristine and prednisone). Shipp MA et al. found that the use of the m-BACOD regimen achieved a response rate of 62% for treating high-grade diffuse large-B cell lymphoma, which is superior to that with the use of the CHOP regimen. However, this single-institution study from Shipp MA, et al. compared their current results with data from previous cooperative-group studies. A few years later, a prospective randomized control trial in the United States concluded that there was no significant difference among the groups in terms of the overall survival, disease-free survival, as well as partial and complete response rates. The particularly good prognosis in treating patients with diffuse large-B cell lymphoma using the m- BACOD regimen may be because of the relatively younger age and lower disease stage [10]. Rituximab plays an important role in improving the complete response rate, disease-free survival, and overall survival when added to the chemotherapy regimens used for diffuse large B-cell lymphoma treatment. Although Bcl-2 overexpression has been associated with poor prognosis in certain subtypes of diffuse large B-cell lymphoma, rituximab prevents treatment failure in patients with Bcl-2 overexpression. However, the benefit of rituximab was less in activated B cell subtypes. Therefore, we choose the m-BACOD regimen plus rituximab in the treatment plan because the patient in our study was young, had a high international prognostic index score, and Bcl-2 overexpression. Eventually, she exhibited complete response after 6 chemotherapy cycles, with no recurrence during follow-up with positron emission tomography after 6 months.
Diffuse large B-cell lymphoma is rarely observed in an emergency setting. Establishment of accurate diagnosis is difficult, especially when patient present to the emergency room with an uncommon presentation of lymphoma. Except great vessel disease, emergency physicians should know that a tumorous origin is the most common cause of mediastinal widening. Moreover, a general work-up should be performed for timely diagnosis and early detection.
We would like to express our special thanks to Dr. Yung Hsiang Hsu, department of pathology in Buddhist Tzu Chi general hospital, for the pathology reports.
The authors certify that the patient has obtained appropriate patient consent form. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initial will not be published and due efforts will be made to conceal her identity and anonymized information.
The case report was made by retrospective chart review.
The authors declare no potential conflicts of interest respect to the research, authorship or publication of this article.
The study procedures were in accordance with ethical standards.
The authors received no financial support for the research, authorship or publication of this article.
All authors strictly adhered to the declaration of Helsinki. Patient's anonymity and confidentiality were preserved.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Liu CC, Wen WC, Niu KY (2024) Rare Presentation of Diffuse Large B-Cell Lymphoma in a Young Woman with a Newly Found Mediastinal Mass. Emergency Med. 14:305.
Received: 20-Aug-2019, Manuscript No. egm-23-1440; Editor assigned: 24-Aug-2019, Pre QC No. egm-23-1440 (PQ); Reviewed: 07-Sep-2019, QC No. egm-23-1440; Revised: 01-Nov-2023, Manuscript No. egm-23-1440 (R); Published: 26-Apr-2024 , DOI: 10.35248/2165-7548.14.305
Copyright: © 2024 Liu CC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : The authors received no financial support for the research, authorship or publication of this article.