Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Case Report - (2023)Volume 13, Issue 3
Background: COVID-19 is associated with lots of complications. Pulmonary thromboembolism is a rare complication of pneumonia that is showing a rising trend in the context of COVID-19.
Case presentation: We present the CTPA findings in 3 patients of pulmonary thromboembolism in patients with COVID-19 pneumonia. The patients had varying involvement of pulmonary arteries. We also provide and update on the published literature on COVID pulmonary embolism.
Conclusion: Pulmonary embolism can complicate COVID-19 pneumonia and lead to poorer prognosis. Hence, the correct diagnosis is imperative as prompt antithrombotic therapy can significantly reduce mortality and morbidity. There have been updates on pulmonary embolism in COVID-19 patients and they have been presented in this study.
COVID-19; Pulmonary Thromboembolism; Pneumonia; CT angiography; Case report
CTPA: CT Pulmonary Angiography; RTPCR: Reverse Transcriptase-Polymerase Chain Reaction; GGO: Ground-glass opacities; PE: Pulmonary Embolism; ED: Emergency Department; CRP: C-Reactive Protein; ICU: Intensive Care Unit; DVT: Deep Venous Thrombosis
COVID-19 pneumonia is known to be caused by the SARS-CoV-2 virus. This global pandemic reached every part of the world since the detection of the first human case in the December 2019 [1]. COVID-19 causes primarily respiratory symptoms that can be mild to severe [2]. Severe COVID-19 pneumonia can cause pulmonary thromboembolism [3]. As countries like China are seeing new COVID waves in December 2022 it is likely that there will be an increase in cases of COVID pneumonia with pulmonary thromboembolism too.
Pulmonary Embolism (PE) is a serious complication that can occur in patients with COVID-19. The occurs when a thrombus forms in the deep veins, mostly in the legs, and then travels to the lungs, where it can block blood flow and cause serious damage. PE is a well-known complication of COVID-19, and the risk of developing the condition is increased in patients with the virus. This is because COVID-19 can cause blood clots to form more easily, and the virus can also lead to inflammation in the lungs and other organs, which can make it harder for blood to flow properly. The features of pulmonary embolism include tachycardia, tachypnea, and dyspnea. In some cases, patients may also experience coughing, fever, and sweating. These symptoms may be similar to those of COVID-19, making it difficult to diagnose PE. Diagnosis of PE is typically made through imaging studies such as pulmonary angiography or Ventilation/Perfusion (V/Q) scanning. Treatment of PE includes anticoagulant therapy, thrombolytic therapy, or a vena cava filter. It should be noted that patients with COVID-19 who have underlying conditions such as obesity, diabetes, hypertension, and cardiac disease, are at a high risk of developing PE. It is important to stay vigilant for clinical symptoms and signs of PE in COVID-19 patients, especially those with underlying conditions. Patients with mild pneumonia undergo chest radiographs and noncontrast chest CT. Patient with severe pneumonia or breathlessness out of proportion to lung involvement undergo CT Pulmonary Angiography for suspicion of pulmonary embolism.
We present imaging findings of 3 cases of COVID-19 pneumonia who developed pulmonary embolism. Computed Tomography Pulmonary Angiography (CTPA) was done on these cases using Isovue 370 iodinated contrast. The amount of contrast used in CTPA varied depending on the patient's body weight.
Case 1
A 68-years old male presented having breathing difficulties with fever for 3 days. His respiratory rate was high at 42 breaths per minute, and he had a low blood pressure of 76 mmHg. He was given oxygen through a non-rebreather mask and received fluids and high-flow nasal cannula to stabilize his condition. Laboratory tests revealed an elevated WBC count, high levels of lactate, creatinine, and CRP, as well as abnormal D-dimer and fibrinogen. RTPCR from nasal swab was positive for COVID-19. D-Dimer was elevated. CTPA revealed small filling defect just distal to bifurcation of right pulmonary artery indicating small thrombus as shown in Figure 1a. Multiple Ground-Glass Opacities (GGOs) were also seen in all lobes of both lungs consistent with COVID-19 pneumonia, shown in Figure 1b. The patient was given a dose of Tissue Plasminogen Activator (TPA) which led to a rapid improvement in his condition. He was given heparin and apixaban for anticoagulation treatment and was discharged from the hospital after a week with improvement confirmed during follow-up telehealth visits (Figures 1a and 1b).
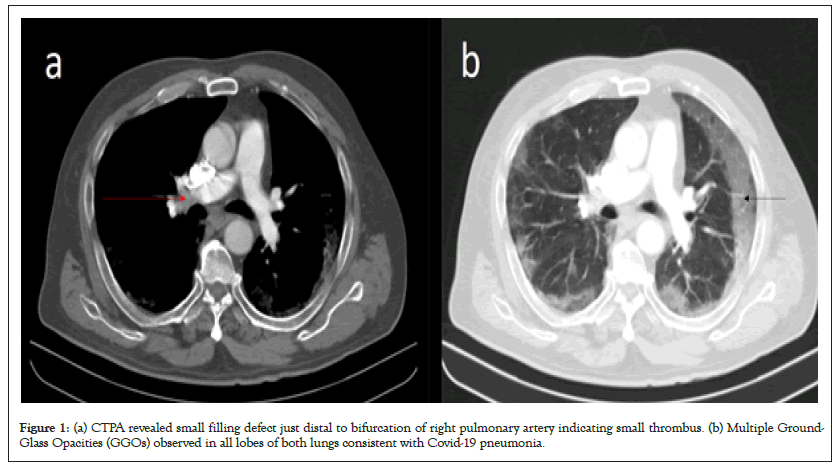
Figure 1: (a) CTPA revealed small filling defect just distal to bifurcation of right pulmonary artery indicating small thrombus. (b) Multiple Ground- Glass Opacities (GGOs) observed in all lobes of both lungs consistent with Covid-19 pneumonia.
Case 2
A 55-years old female having no major past medical issues was admitted to the ICU with severe respiratory distress. She had been experiencing symptoms such as fever, shortness of breath, muscle pain, loss of smell and taste for 12 days, and was positive for COVID-19 through a nasal Polymerase Chain Reaction (PCR) test 8 days ago. At the time of admission, her temperature was high at 102.4 F, heart rate was at 114 beats/minute, she was breathing rapidly at 39 breaths per minute, and had low oxygen saturation levels at 81% on room air. Laboratory tests showed an elevated WBC count with low lymphocyte count, mild liver inflammation, increased creatinine levels, high ferritin, lactate dehydrogenase, C-reactive protein, creatine kinase, D-dimer, procalcitonin, troponin, and B-type Natriuretic Peptide (BNP) levels. She was admitted to the ICU. She was started on tocilizumab, hydroxychloroquine, antibiotics, proning, and received enoxaparin prophylactically. Being taken off the ventilator on the 9th day, she had another episode of hypoxia requiring high flow nasal cannula oxygen. On CTPA, filling defects were seen at bifurcation of right and left pulmonary arteries extending into proximal part of all the lobar arteries, shown in Figure 2a. Patchy flow is seen in distal lobar and segmental branches. Findings indicated bilateral pulmonary partial thrombosis. Interstitial thickening and GGOs were seen in all lobes of both lungs as shown in Figure 2b. She was administered anticoagulation therapy (heparin followed by apixaban) and improved and shifted from the ICU in the following week (Figures 2a and 2b).
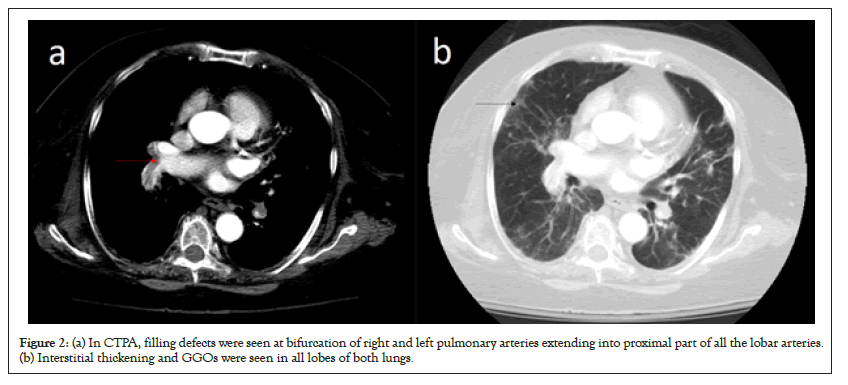
Figure 2: (a) In CTPA, filling defects were seen at bifurcation of right and left pulmonary arteries extending into proximal part of all the lobar arteries. (b) Interstitial thickening and GGOs were seen in all lobes of both lungs.
Case 3
A 44-years old man presented with dyspnea for 4 days and was admitted into the hospital with low oxygen levels. At the time of admission, his heart rate was 112 beats/minute, and oxygen saturation levels were low at 83% on room air. Laboratory tests showed elevated WBC count, high levels of BNP, troponin, CRP, lactate dehydrogenase, D-dimer, ferritin and procalcitonin. RTPCR from nasopharyngeal swab was positive for COVID-19. D-Dimer was elevated. CTPA demonstrated filling defect at bifurcation of right pulmonary artery and extends into its right descending branches indicating pulmonary thrombosis, shown in Figure 3a. GGOs were seen in all lobes of both lungs as shown in Figure 3b. The patient underwent a successful mechanical thrombectomy using FlowTriever, which improved his oxygenation. Nasopharyngeal PCR test returned positive for COVID-19. He was administered antibiotics, hydroxychloroquine, and anticoagulation. Despite these treatments, his condition deteriorated with worsening lung inflammation. The patient finally succumbed to COVID-19 infection and pulmonary thromboembolism (Figures 3a and 3b).
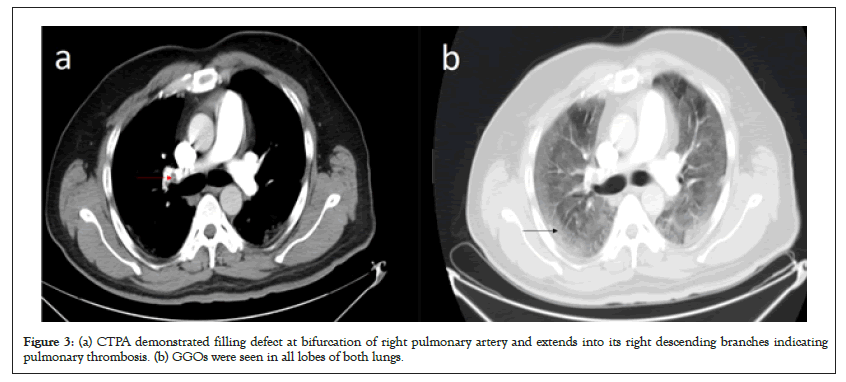
Figure 3: (a) CTPA demonstrated filling defect at bifurcation of right pulmonary artery and extends into its right descending branches indicating pulmonary thrombosis. (b) GGOs were seen in all lobes of both lungs.
Relationship between pulmonary embolism and disease severity
Yassin and colleagues [3] studied the connection between the occurrence of Pulmonary Embolism (PE) and the severity of COVID-19, as determined by lab results or CT scan scores. They included 96 patients with COVID-19 who were suspected of having PE and found that 40 of them tested positive, making up 41.7% of the patients. The study found that features such as worsening tachypnea, reduced oxygen levels, dyspnea, and coughing up blood were statistically significant indicators of PE, however, no significant difference was noticed regarding age or gender and the incidence of PE. The study also looked at the relationship between lab markers such as D-dimer, ferritin, CRP, white blood cell count, neutrophils, and lymphocytes and the incidence of PE, but found no significant correlation. However, subjects with positive PE had higher CRP and D-dimer compared to those having negative PE. Additionally, the study found that the progression of the disease was highly significant with the incidence of PE, suggesting that close monitoring of critically ill patients is crucial for early diagnosis and treatment.
Acute phase characteristics and long-term complications of pulmonary embolism in COVID-19 compared to non-COVID-19 patients
Franco-Moreno et al. [4] looked at the relationship between PE and the severity of COVID-19. Their study found that there were differences between PE characteristics in COVID and patients without COVID-19. COVID-19 patients did not have the classical risk factors for PE and had more markers of systemic inflammation. Radiologically, COVID-19 patients had a distal thrombi location and a lesser incidence of deep vein thrombosis. The study also found that mortality in hospitals was lower in COVID-19 patients, largely due to a higher prevalence of end-stage cancer causing death in non-COVID-19 subjects. The study also demonstrated that the risk of recurrent Venous Thromboembolism (VTE) in patients with COVID-19 was less, suggesting that stopping anticoagulant therapy after three months may be appropriate. Additionally, the incidence of Chronic Thromboembolic Pulmonary Hypertension (CTEPH) was lower in COVID-19 patients due to the distal topography of pulmonary embolism.
COVID-19 and Pulmonary Embolism Outcomes among Hospitalized Patients
Nasrullah A et al. [5] study is the largest one assessing the outcomes of patients with COVID-19 with and without PE. It consists of 1.6 million patients having COVID-19 pneumonia that were hospitalized. The study found that COVID-19 patients with PE had increased mortality in-hospital, cardiogenic shock, and need for mechanical circulatory support in comparison to those without PE. They also required a higher amount of vasopressors and ventilation and had a longer hospital stay and higher hospitalization costs. Male sex and old age were found to cause a higher rate of mortality in both COVID-19 patients with or without PE, however, there was no relation of mortality with income, insurance, or race. The study also found that the rate of PE in patients with COVID-19 was 2.8%, which is less than reported in previous literature. The study notes that the difference in mortality could be explained by many factors including selection bias, sample size, and different virus strains.
Risk of thromboembolic events in non-hospitalized COVID-19 patients
The study by Massoud and colleagues [6] indicates that COVID-19 increases the chances of DVT in non-hospitalized patients. Furthermore, the study suggests that patients with COVID-19 who are not hospitalized have a significant risk of pulmonary embolism in comparison to the control group without COVID, even at mild or asymptomatic infection levels. COVID-19 increases the chances of Myocardial Infarction (MI) in non-hospitalized patients. The chances of MI and stroke is significant in the first 7 days of COVID-19 infection, however, drop to insignificance within two weeks following the infection. This could be due to the prothrombotic and pro-inflammatory condition in the acute phase, leading patients to thromboembolism during both the infection phase and recovery phases. Factors such as vascular inflammation, hypoxia and endothelial dysfunction may also contribute to this increased risk.
Prediction of pulmonary embolism in patients with SARSCoV- 2 infection
Franco-Moreno et al. [7] found a high incidence of PE among patients with COVID-19, with 25.54% of patients in their study diagnosed with PE. This is consistent with other studies on critically or severely ill patients, but higher than the general population. All subjects in the study were on anticoagulation, raising questions about the development of PE despite prophylaxis. Factors independently associated with PE were found to be tachypnea and the absence of infiltrates on chest radiographs and increased D-dimer levels. However, the study found no clear risk factors for PE among patients with COVID-19 and no effective tools to predict PE in emergency department patients.
Prognostic association between d-dimer thresholds and 30-day pulmonary embolism diagnosis among emergency department patients with suspected SARS-CoV-2 infection
In a study published in 2023 by Lin et al. [8] of 10,837 patients, 3.7% of subjects were found to have PE at 30 days. A D-Dimer threshold of 500 ng/mL had a sensitivity of 97.8% and a specificity of 40.9%. An age-adjusted D-dimer threshold had a sensitivity of 96.0% and a specificity of 48.5%. D-dimer testing was less accurate for predicting PE in patients who were positive for COVID-19 infection. Overall, the standard and age-adjusted D-dimer thresholds were similarly effective for predicting PE in the Emergency Department (ED) patients with suspected COVID-19 infection as in non-COVID ED patients.
Assessment of pulmonary embolism related to active SARSCoV- 2 infection in pregnant women
Moreno-Ballesteros et al. [9] found that pregnant patients must be anticoagulated at the minimum suspicion of PE. As they have a greater risk of bleeding and the need for its monitoring, so it is crucial to rule out early the presence of thrombotic phenomena. Although in the pregnant patient diagnosed with PE the D-dimer value was practically double that of the rest, this value continues to be a highly variable parameter and unspecific. Also, the effect of PE also turns out to be more serious for the fetus as it causes fetal distress due to low oxygenation. One patient had to undergo a cesarean section due to fetal distress following PE. Additionally, it should be noted that this patient presented a peripheral distribution sub segmental pattern of perfusion defects on scintigraphy, as described by other authors in patients diagnosed with Pulmonary Thromboembolism (PTE) during COVID19 infection. Considering the non-specific nature of the clinical features and the D-dimer values in the COVID-19 context in pregnancy, perfusion scintigraphy lung plays a fundamental role in the diagnosis of PE, due to its higher sensitivity and lower radiation than CT.
The cases presented above highlight the different ways in which COVID-19 and PE can present. Studies have shown that COVID-19 patients have an unusually higher risk of thromboembolism [10]. Research has also found a connection between the severity of COVID-19 and clot turnover, with patients who have higher levels of markers having a poorer prognosis. Additionally, studies suggest that for patients with severe COVID-19 disease, prophylactic anticoagulation may reduce mortality. The exact mechanisms behind the clotting problems related to COVID-19 are not fully understood, but it is believed that the virus infects vascular endothelial cells, causing damage and platelet activation. It is unclear to what extent COVID-19 increases the chances of thrombosis compared to other causes. In conclusion, it is important to maintain a high suspicion for thromboembolic disease in patients with COVID-19, especially those with unexplained hypoxemia, critical illness, or rapid deterioration. More research is required to understand the importance of empiric or preemptive therapeutic anticoagulation in treating COVID-19 patients.
Not applicable.
Not applicable.
Not applicable.
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
The authors declare that they have no competing interests.
No funding was obtained for this study.
SSB analyzed and interpreted the data. SSB was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Not applicable.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Biswas S (2023) Pulmonary Thromboembolism in COVID-19 Pneumonia: A Case Series and Update. Emergency Med. 13:294.
Received: 16-Aug-2023, Manuscript No. EGM-23-26117; Editor assigned: 18-Aug-2023, Pre QC No. EGM-23-26117 (PQ); Reviewed: 04-Sep-2023, QC No. EGM-23-26117; Revised: 11-Sep-2023, Manuscript No. EGM-23-26117 (R); Published: 18-Sep-2023 , DOI: 10.4172/2165-7548.23.13.294
Copyright: © 2023 Biswas S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.