Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Research Article - (2016) Volume 6, Issue 2
Objective: In Benin, as life expectancy continues to increase, the number of postmenopausal women increases. Menopause is a physiological phenomenon that can be quiet for some+, tumultuous in others. Few studies are devoted to menopause in Africa and Benin in particular. The objective of this study was to describe the profile, clinical symptoms of menopausal women as well as management of postmenopausal symptoms in Cotonou, Benin.
Materials and method: This is an analytical cross-sectional study in Cotonou, the capital city of Benin Republic during the month of August 2014. 2021 women were included in the study out of a female population of 11,669 people aged 40 and older.
Results: 52.7% of the participating women 40 or older were postmenopausal. The mean age at menopause in the sample was 47.5 years, and the largest age group was 50 to 59 years old. Clinically, the most frequent menopausal side effects were hot flashes (58.7%), libido disorders (67%), and joints pain (38.8%). The most frequent associated pathology was hypertension in 37.7% of cases. Factors that limit access to hormonal treatment of menopause in Cotonou include lack of information (66.17%) and financial barriers (19.65%).
Conclusion: Health promotion must address obesity, hypertension and smoking to reduce the negative effects of menopause in Sub Saharan Africa.
Keywords: Menopause; Morbidities; Profile; Clinical symptoms
The number of postmenopausal women in the world in 1990 was estimated at 467 million, 60% in the developing countries and is expected to reach 1.2 billion by 2030 [1]. In metaanalysis of Ghazanfarpour than an estimated one billion women have experienced menopause worldwide [2]. Menopause or period of quiescence of the reproductive system [3] is a natural phenomenon but can be charged many disorders. In Benin, as the case for many Sub-Saharan Africa countries, the number of post-menopausal women is increasing thanks to gradually improving life expectancy. This lifecycle period is quiet for some women tumultuous for others. Unlike European countries, North American and Asian, few studies are devoted to menopause in Africa and Benin in particular. The problematic of menopause often being relegated to second place the concerns of health authorities. Three decades after the first studies on menopause in Cotonou , and facing the increasingly important demand for care of menopausal women, it seemed necessary to realize this study which the objective was to describe the profile, clinical symptoms of menopausal women as well as management of postmenopausal symptoms in Cotonou, Benin
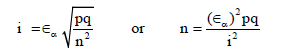
The study took place in Cotonou, the capital city of Benin. It was an analytical cross-sectional study, conducted in August 2014. The sample consisted of women over 40 who are ordinarily resident in Cotonou (at least 9 months per year) and with at least one year of amenorrhea at the time of the study. Women younger than 40 years were not included in this study, as well as women in transit in Cotonou at the time of the survey, as well as those suffering from amenorrhea from other causes other than menopause. The city of Cotonou is divided into 140 areas grouped into districts. We calculated the minimum sample size from the Schwartz formula:
α = Significance threshold
ε = z-score of the normal distribution
For α = 0,05 ε = 1,96
i = margin of error; it varies in medical studies between 2% et 8%. In this study we chose 2% to increase the likelihood of detecting any association.
p = proportion of menopausal women of a given age in the female population of Cotonou.
In a doctoral thesis done on menopause in 2004, the average age of menopause was 49.2 years; with ages between 43 and 56 years. If p = proportion of women 40 years of age, q = complementary probability of p (1-p), the required minimum size for the study was obtained by multiplying the size calculated by the correction of the cluster effect factor (Fc) to minimize bias in the sampling technique. The corrected minimum size (Nc) = n × Fc; Fc = 1.3
For this minimum size we conducted a random sample, multiphase, sampling, and in clusters. The ideal scenario would have been to follow a cohort of women early in the menstrual disturbances until years after cessation of the menarches and observe the chronology of appearance of different manifestations of perimenopause and menopause. It would have taken years and especially important logistics. To remedy this we performed a pseudo cohort significant representation of each age of menopause. To build this cohort we needed to know the size of the female population over 40 years old in 2014. These recent data are not available at the time of the study we estimated the population based on census data from 2002 according to the formula below: Population in 2014 = Population in 2002 (1 + r), where r = average annual growth rate = 4.12% from 2002 to 2014. By projecting the total female population and that of at least 40 years we had estimates of 555,072 and 82,019 respectively. Thus the minimum sample size obtained from the formula is 1356 and a corrected minimum size is 2,712 women.
We considered each areas of the city of Cotonou as a stratum.
The total number of clusters recommended by the World Health Organization (WHO) for this type of sampling is 30. Data were collected by interviewers (medical students and doctors enrolled in specialized studies diploma in gynecology obstetrics) during interviews and during the clinical examination. The clinical examination was limited, given available means and local conditions, to weighing measurement, body mass index (BMI), and blood pressure. Statistical tests used were Khi2 and binary logistic regression. For chi2 values, the probability p is determined; the difference is statistically significant when p <0.05.
Limits and Constraints: There was no hormonal assay to confirm or menopause, and no diagnostic test for osteoporosis. In other studies, menopausal hormone assays such as FSH and estradiol were assessed and we could not perform these tests because of limitations of means in our context.
Profile of postmenopausal women in cotonou
2,716 postmenopausal women were identified in a total female population sample of 15,943 people of all ages representing the sampled population from which 5155 were at least 40 years. Thus, the proportion of postmenopausal women in this study was 52.7% of women over 40 years, and 16.8% of the total female population sampled.
The mean age of postmenopausal women was 59.30 years, ranging from 42 years to 100 years (Figure 1). Women 50 to 59 were the most numerous with a frequency of 37.8%. Most menopausal women were not educated (57.4%) similar to the high female illiteracy in the general population. In terms of occupation, small business represents 44.4%. Almost half of menopausal women were married or living in union (47.7%). Age at menarche was provided by 98.3% of women. The mean age at menarche was 16.8 years (CI: 14.6 to 19) with a minimum at 10 years and the maximum at 25 years.
The length of the menstrual cycle varied between 25 and 35 days in 99.6% of cases. The normal duration of the menses varies from 4 to 7 days, and was found in 77.40% of cases. The age at first pregnancy, recorded from 2520 postmenopausal women was on average 22.20 years ± 3.70 years. The lowest age was 12 years and the highest 48 years. Similarly, the mean age at last pregnancy, recorded from 2513 postmenopausal women provided was 36 ± 5.9 years. In summary, the profile of women in our sample is similar to the profile of women over 40 in the latest census in Benin (RGPH 2002).
In bivariate analysis, age at menarche less than 15 years increases by 50% the likelihood of menopause before the age of 47.5 years (Table 1). Similarly, history of hypertension, multi-parity, age at first pregnancy between 17 and 25 years, and history of uterine fibroma were associated with increased likelihood of menopause at early younger ages.
| Factors | Odds Ratios (OR) | Confidence Intervals (CI) |
p-value |
| First menses before age 15 | 1,5 | 1,2 – 2,0 | < 0,05 |
| Family history of hypertension (HBP) |
2,5 | 2,0 – 2,8 | < 0,05 |
| Multi parity | 2,2 | 1,6 – 2,9 | < 0,05 |
| First pregnancy between age 17-25 | 1,4 | 1,0 – 1,7 | < 0,05 |
| History of uterinefibroma | 1,6 | 1 – 2,5 | < 0,05 |
Table 1: Factors associated to onset of menopause among postmenopausal women and her dependent variables, logistic regression analysis from in Cotonou, Benin, in 2014.
Contraception use history
85.35% of the postmenopausal women have not practiced modern contraception during their reproductive years. This is not surprising given the very low modern contraceptive prevalence rates over decades in the country. The duration of modern contraceptive use during the reproductive life reported by 47 postmenopausal women was between 1 and 3 years. In terms of methods, the oral contraception was the most used in 40.2% of cases. The duration of reproductive health life (elapsed time from age at menarche to age at menopause), was documented in 2364 women. In 79.23% of the respondents (2716) the duration of reproductive health life was between 25 and 35 years. At the time of the survey, the mean duration of menopause (time between when menopause occurred and the date of the survey) was 11.82 years.
Clinical symptoms and morbidities in postmenopausal women
Table 2 summarizes the clinical symptoms of postmenopausal women in Cotonou, Benin. The most common manifestations of menopause are hot flashes the 58.7%, sweating (50.9%), irritability (51.2%), and memory loss (64.3%).
| Signs and symptoms | Number | Percentage (%) N= 2716 |
|---|---|---|
| Vasomotor troubles | ||
| - Hot flushes | 1595 | 58,7 |
| - Hyper sweating | 1383 | 50,9 |
| - Paresthesia | 1913 | 70,4 |
| - Headeaches | 1910 | 70,3 |
| - Lipothymia | 730 | 36,1 |
| - Heart palpitations | 1014 | 37,3 |
| Psychic troubles | ||
| - Physical Asthenia | 2061 | 75,9 |
| - Insomnia | 1412 | 52,0 |
| - Memory loss | 1747 | 64,3 |
| - Irritability/Nervosness | 1390 | 51,2 |
| - Jealousy events | 389 | 14,3 |
| - Autoritarism | 341 | 12,6 |
| - Psychic Asthenia | 1193 | 43,9 |
| General Involution | ||
| - Wrinkles on the face | 1779 | 65,5 |
| - Wrinkles outside the face | 1921 | 70,7 |
| - Fragile hair texture | 1723 | 63,4 |
| - Breast atrophy | 725 | 26,7 |
| - Loss of libido | 2071 | 76,3 |
| - Frigidity | 887 | 32,7 |
Table 2: Distribution of symptoms among postmenopausal women in 2014, Cotonou, Benin.
In terms of transition into menopause, 31.78% of respondents reported a sharp transition from the reproductive years to menopause without irregularities of the cycle whilst for the remaining majority (68.22%), menopause had settled in gradually through a period of menstrual disorders.
The Body Mass Index (BMI) was assessed in 2,713 postmenopausal women. The BMI was below 18.5 in 3.3% of cases (underweight women), normal between 18.5 and 24 9 in 29.1% of cases (normal weight women) and in 31.3% of cases in our sample the postmenopausal women were overweight. 36.3% of the women were obese with a BMI over 30.
There were also sexual disorders associated with menopause in our sample. Among the 2716 postmenopausal women, there were 348 no response for decreased in libido after menopause and 1174 no response for question on frigidity. Among postmenopausal women who complained of decreased libido, married and widows were in similar proportions, 45.8% and 43.8% of cases respectively. These percentages are significantly lower than the 53.9% of married women who reported no reduced libido. Among postmenopausal women who complained about frigidity widows were 50% of the cases.
Hypertension was the most common family medical history in 41.3% of cases. The family history of diabetes was observed in 16.08% of the cases. The most frequent observed morbidity in our sample was hypertension (37.7%). The frequencies of osteoporosis, depression and urinary incontinence and among postmenopausal women in our study were 15.68%, 56.1% and 5.81% respectively. Two rare conditions were also documented: breast cancer (0.33%) and endometrial cancer (0.14%). Using the blood pressure and pulse we estimated the cardiovascular risk of the postmenopausal women. We could not use the tables published by the European Society of Cardiology which include cholesterol level. We estimated the cardiovascular risk factor instead by calculating the pulsed pressure (PP).
The results obtained are the following: In patients with hypertension, normal PP (no risk) was observed in 263 out of 617 cases (42.62%) and high PP (high risk) was observed in 354 of 617 cases (57.37%). In patients with normal blood pressure, normal PP (no risk) was observed in 836 out of 1404 cases (59.54%), and high PP (risk) was observed in 568 out of 1404 cases (40.45%). We thus observed a high cardiovascular risk among postmenopausal women with high blood pressure.
Treatment of menopause symptoms
On the treatment level, 17.9% of postmenopausal women have consulted a health worker. Only 22.6% of respondents were informed of the existence of a menopause treatment. The proportion of women on hormonal treatment for menopause was 4.42%. Factors that limit access to hormonal treatment of menopause in Cotonou include lack of information (66.17%) and financial barriers (19.65%).
The profile of women in our sample is similar to the profile of the woman at age 40 in Benin (RGPH 2012) and the proportion of postmenopausal women was 17.4% in the female population of Cotonou. This is significantly lower to proportions of among women over 40 years in other settings where life expectancy is significantly greater. As examples, in Turkey a retrospective analysis on 136,985 women received in 24 medical centers, noted a prevalence of 72% for natural menopause, 23.9% for surgical menopause and 3.8% for early menopause [4]. In France it is estimated the number of postmenopausal women was 10 million in 2004 [5], which corresponds to 13.7% of France population at the time.
The average age of menopause in Cotonou fits within the range of the observed average age at menopause globally is between 45 and 55 years although in line with the conclusions of an expert WHO panel which indicate the average age of menopause in developing countries is slightly lower than that of developed countries [1,6]. Although women's life expectancy at birth (different in different countries) is improving in Benin, the life expectancy for women 50 and older is not significantly different across countries worldwide.
Among the authors who have studied the menopause, apart from smoking, disagreements exist about the factors that may influence the age at menopause. Menopause is known to occur earlier in postmenopausal women who smoke than those who do not smoke. This difference also exists within the same smokers among heavy smokers and those who smoke less [1]. There has not been a study of the effect of smoking on menopause in our context and this may be linked to the very low smoking prevalence particularly among women. However smoking is increasing among adolescents in Sub Saharan Africa. Active-ever smokers reached menopause 21.7 months earlier than the mean of 49.4 years for never-smokers not exposed to SHS, and women exposed to the highest level of SHS reached menopause 13.0 months earlier [7]. Factors influencing age at menopause in our series before age 50 include age at menarche before age 15, family history of hypertension, multi-parity, age at first pregnancy between 17 and 25 years and existence of uterine fibroma (Table 1). We did not explore in a multivariate analysis the variance explained by each factor as this was not the purpose of this study.
Regarding clinical symptomatology and morbidities, hot flashes were the most common symptom of menopause (58.7%) in our series compared to a frequency ranging from 70 and 80% found by various authors around the world. Our frequency is significantly lower than the 80% reported in Dutch population, significantly higher than 0% reported by Maya women, 12 to 22% reported by Hong Kong women, 17% reported by of Japanese women, and 5.7 to 37.7% reported by women in Thailand. These results along with the generally high frequency reported in North America (45% to 75%) indicate it may be possible that cultural norms, education, climate or other factors play in observed prevalence of hot flashes in postmenopausal women across the world [8] . In fact, some authors have reported the influence of ambient temperature on the frequency of hot flashes, a cool temperature reduces flashes while a high temperature exacerbates. We could not confirm this in our study (Table 2).
Although 56.1% of menopausal women in our study had depression, some authors mention that there is little evidence that suggests women become depressed during menopause. In the study of Osinowo [9], menopausal women Nigerians living in Ibadan had better psychological health than women in Nigerian perimenopause. In one meta-analysis concerning 67714 women showed that the duration of reproductive period influences the psychological troubles of menopausal. Menopause at age 40 or more years compared with premature menopause was associated with a 50% decreased risk for depression [10].
Weight gain and obesity were assessed in our study using BMI. This was different from most studies in which obesity was measured by waist circumference which is more directly correlated to the insulin resistance regardless of age, gender or BMI [11], and waist circumference is also the most important predictor anthropometric parameter cardio vascular and metabolic disease after BMI. Of 27 selected variables, the factors significantly related to ≥ 3% weight gain were weight change in the past 2 years, age at menopause, dietary fiber, fat, alcohol intake, and smoking [12].
Epidemiological data on weight gain at onset of menopause are not frequent, although anecdotally many women complain of weight gain during this lifecycle period [13]. Between 42 and 50 it is noted a mean weight gain of 0.8 kg/year in women. However there is considerable individual variation in the intensity of this weight gain, as 20% of women take 4.5 kg or more in 3 years, while only 3% lose weight. Predictors of weight gain are essentially race (black women gain more weight than white) and decreased physical activity [13]. A reduction of this android obesity is known to reduce the risk of several morbidities including breast and genital cancers, cardiovascular risk among women.
Regarding genital disorders, dyspareunia was the most commonly reported side effect (10.5% of cases) followed by vulvo-vaginal pruritus in 9.42% of cases. The frequency and especially the date of onset of these symptoms are highly variable across the literature, depending on a residual estrogenic impregnation of sexual life of women. For the majority of women interviewed in our study there was no statistically significant difference in levels of libido or frigidity during menopause irrespective of marital status.
Osteoporosis and fractures that often follow represent a major public health problem. The frequency of osteoporotic fracture is rising in many countries. Reasons for this relate in part to the increased longevity of the population, which is occurring both in the developed and underdeveloped world [14].
In our study, because of lack of diagnostics technics, we used pathological bone fractures other than those caused by neoplastic metastasis and joint pains as clinical suspicion for osteoporosis. The overall frequency is low in our study (15.68%) and reflects also the low predictive positive value of such clinical symptoms as diagnostic tools for osteoporosis. In other studies, 10-20% of osteoporosis in postmenopausal women are reported to be linked to a secondary cause [15,16], which implies the need to confirm and eliminate a possible secondary cause before considering therapeutic management of any osteoporosis [17]. Because of the high cost of his care, treatment of these osteoporotic fractures remains prohibitive in developing countries such as Benin. Prevention is the best solution in these countries. It is based on the eviction of risk factors such as smoking, excessive alcohol consumption, a balanced diet rich in calcium and vitamin D and the promotion of regular physical activity should be in all postmenopausal women, fall prevention.
The prevalence of hypertension in postmenopausal women in the study was 37.7%, lower than the average 56.87% prevalence of hypertension among adults of both sexes reported in a study in 2002 in the coastal departments (Capital city of Cotonou and Atlantic province), and similar to the 38.8% prevalence reported in two of the northern and more rural departments (Borgou and Alibori). This difference in the Capital city of Cotonou and surroundings may be related to the nutrition and lifestyle of the city, including stress.
Finally, although the proportion of postmenopausal women on hormonal replacement treatment (HRT) is very low in our survey, the use of HRT is increasing over the last 10 years from a proportion of women in this treatment was 0.54% in 2004 However, access to hormonal treatment of menopause remains limited due to lack of information and financial barriers. Often prescribed to mitigate the effects of menopause, the hormonal treatment of menopause experienced a drastic reduction of its requirements in the world following a publication in 2002, the first results of the US study, Women's Health Initiative (WHI ). This study found indeed more risks than benefits in hormonal menopause treatment over the long term. The WHI study (Women's Health Initiative ) and MWS (Milllion Women Study ) have helped draw the attention of prescribers and women on these "alternative" treatments [18,19].
With the increase in life expectancy in Benin and in the world, more and more women are reaching age of menopause and living many years after menopause. Health promotion must address obesity, hypertension and smoking to reduce the negative effects of menopause in women.