Journal of Thyroid Disorders & Therapy
Open Access
ISSN: 2167-7948
ISSN: 2167-7948
Case Study - (2021)Volume 10, Issue 6
Introduction: The prevalence of metabolic syndrome is increasing worldwide with distinct evidence of high prevalence in southern countries including India. Recent evidence suggests thyroid dysfunction primarily subclinical hypothyroidism has been prevalent in the general population. Studies show both metabolic syndrome and thyroid dysfunctions are independent risk factors for cardiovascular disease. Hence estimating the prevalence of metabolic syndrome and thyroid dysfunction in the study population may help to take preventive measures to decrease the complications of non-communicable diseases.
Aim: To estimate the prevalence of metabolic syndrome and to observe the pattern of hypothyroidism among the north coastal Andhra population.
Materials and methods: A cross sectional study was conducted among 925 patients attending the outpatient department of the GVP Medical College, Visakhapatnam, from the North coastal area. Blood pressure and anthropometric measures were taken. Blood glucose, lipid profile and thyroid profile were measured using fasting blood samples.
Result: Among the 925 subjects screened for metabolic syndrome 356 (38%) had metabolic syndrome. Overt hypothyroidism was found in 4.3%, subclinical hypothyroidism (TSH 5.5-10 mIU/L) was observed in 25.3%, (TSH above 10 mIU/L) in 26.4%, hyperthyroidism and subclinical hyperthyroidism was found in 0.9% and 2.2% respectively.
Conclusion: Our study showed a higher prevalence of metabolic syndrome and subclinical hypothyroidism among the study population. Hence the study suggests assessing the metabolic components and thyroid profile as a routine analysis in the study area. The association of components of metabolic syndrome, dietary pattern and measurement of ant TPO (Thyroid peroxidase) antibodies among the study population has to be studied to protect them from complications of diabetes and thyroid disease.
Metabolic syndrome; Hypothyroidism; Subclinical hypothyroidism; Cardio vascular disease
Metabolic syndrome is a cluster of risk factors characterized by obesity, dyslipidemia, diabetes mellitus and arterial hypertension, prothrombin and proinflammatory conditions [1]. The prevalence of metabolic syndrome is increasing worldwide with a distinct evidence of an increase in southern countries, including India [2]. It has been estimated that understanding the prevalence of metabolic syndrome is essential to predict the future burden of diabetes mellitus and cardiovascular diseases among the Indian population [3].Thyroid disease is an endocrine disorder where the thyroid gland produces excess or low thyroid hormones. Many observational studies suggest there is an increasing prevalence of thyroid dysfunction even with the advent of iodine supplementation and in seafood consuming population [4-6] Literature also reveals that TSH (Thyroid- Stimulating Hormone) level above 10 mIU/L leads to cardiovascular disease [7]. Hence the present study is aimed to estimate the prevalence of metabolic syndrome among the north coastal Andhra population and observe the pattern of thyroid dysfunction among the study population to help in taking preventive measures from the complication of these noncommunicable diseases.
A cross sectional study was conducted from Jan 2018 to Dec 2020 and the study participants were representative from the north coastal region of Visakhapatnam, Andhra Pradesh. The study included 925 patients aged between 20-60 years, attending the outpatient department of the GVP Medical College, Visakhapatnam. Blood pressure and anthropometric measures were taken using standard procedures. Blood glucose, lipid and thyroid profile were measured using fasting blood samples.
Metabolic syndrome was defined using the NCEP ATP III (National Cholesterol Education Program Adult Treatment Panel III) criteria [8]. Patients who fulfilled any three of the following five risk determinants were considered to have metabolic syndrome. (Increased BP≥130/85 mmHg, impaired fasting blood glucose (≥110 mg/dl)/TGL (≥150 mg/dl) or decreased HDL (<40 mg/dl in men, <50 mg/dl) or increased waist circumference (>102 cm in men (>40 inches), >88 cm in women (>35 inches)
Thyroid function was defined based on the TSH levels, as euthyroid (TSH 0.3-5.4 mIU/L), subclinical hypothyroidism (normal/altered T3 (Triiodothyronine), T4 (thyroxine) and TSH 5.5-10.0 mIU/L), overt hypothyroidism (TSH>10 mIU/L), subclinical hyperthyroidism (normal/alteredT3, T4 and TSH <0.3 mIU/L) and hyperthyroidism(TSH <0.3 mIU/L) [9].
Inclusion criteria
Patients with Type 2 Diabetes mellitus, Blood pressure ≥130/85 mm/Hg, Obese subjects (WC->102 cm in men and 88 cm in women)
Exclusion criteria
Patients with type-1 Diabetes mellitus, known metabolic disorders.
Ethical issues
The study was approved by the institutional ethical committee. The participants were informed about the study and informed consent was obtained.
Statistical analysis
Statistical Package for Social Sciences (SPSS) version 16.0 was used for statistical analysis. Results of prevalence were expressed in numbers and percentage.
In the present study (Figure 1) among the 925 study participants screened for metabolic syndrome 356 patients had metabolic syndrome and the prevalence of metabolic syndrome among the study population was found to be 38%. Among the metabolic syndrome subjects 46 (12.9) were males and 310(87.1%) were females.
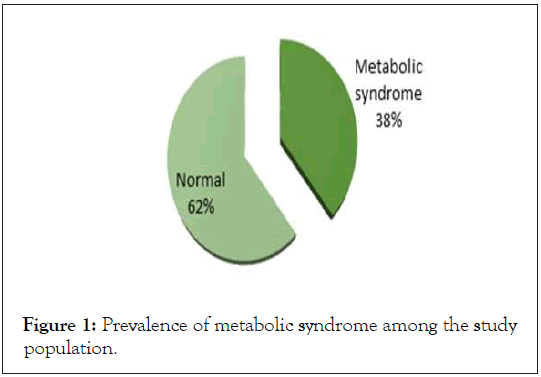
Figure 1: Prevalence of metabolic syndrome among the study population.
The reports of a systemic review revealed that 12%–37% of the Asian population and 12%–26% of the European population suffer from metabolic syndrome [10]. In a study by Gupta et al. in 2004, the prevalence of the metabolic syndrome in the Indian population was found to be 31.6%, (22.9% in men and 39.9% in women [11]. A systemic review and meta-analysis done in 2020 reported the prevalence of metabolic syndrome in different parts of India as follows. North India -30%, central India-27%, eastern India -33%, southern India -30% and north east India -35%[12].
Studies in rural and urban population of Andhra Pradesh showed the prevalence of metabolic syndrome as 25% to 32%, respectively [13-14]. Another study in urban elderly people of Tirupati, Andhra Pradesh showed the prevalence of metabolic syndrome to be 34.58 [15].
Our report is in agreement with other studies that there is increasing prevalence of metabolic syndrome among the population of north coastal Andhra region. The high prevalence observed may be due to the increasing urbanization which leads to changes in life style and food habits or may be due to genetic factors. It has been well reported that patients with metabolic syndrome have an increased risk of cardiovascular morbidity and mortality [16]. Hence the study suggests a routine screening of metabolic components in the study area to prevent them from complications of metabolic syndrome.
Figure 2 shows the pattern of thyroid function among the study population. In the present study the prevalence of subclinical hypothyroidism (normal/altered T3 and T4 with a TSH level between 5.5 -10.0 mIU/L.) was found to be 25.3%. Among the study population overt hypothyroidism was found in 4.3%, hyperthyroidism was found in 0.9% and 2.2% had subclinical hyperthyroidism. Our results also showed that 26.4% of the study participants had a normal/altered T3 and T4 with a TSH value above 10.0 mIU/L.
Figure 2: Pattern of thyroid dysfunction among the study population.
Prevalence of thyroid disorders varies among gender, age and different ethnic populations. Bagcchi, reported a higher prevalence of hypothyroidism in India (11%) when compared with UK (2%) and USA (4-6%).(4) A study involving 25,862 participants attending a state health fair (Colorado Thyroid Disease Prevalence study),showed 9.5% of the participants had an elevated TSH level and 2.2% had a low TSH level [17].A cross sectional multicentric epidemiological study involving 5376 participants conducted in eight major cities of India reported the prevalence of thyroid dysfunction as hypothyroidism 10.95%, subclinical hypothyroidism 8.02%, hyperthyroidism 0.67%, and 21.85% tested positive for antiTPO antibodies [18]. A prevalence study conducted among 8179 participants attending a tertiary care hospital in northern Kerala, reported the overall thyroid dysfunction as 15.73% and among this the highest being subclinical hypothyroidism (7.15%) followed by overt hypothyroidism (4.2%), hyperthyroidism (2.77%) and subclinical hyperthyroidism (1.6%) [19]. A study Cochin on 986 adults showed the prevalence of hypothyroidism as 3.9% and subclinical hypothyroidism as 9.4% [6]. The reports of a retrospective study in 2018 in patients attending King George hospital from north coastal region of Andhra Pradesh showed 43.7% had thyroid dysfunction [20]. A study in east Godavari of Andhra Pradesh showed a higher prevalence of subclinical hypothyroidism 36.5% and hypothyroidism was observed in 12.73%.
The results of our study showed that a major proportion of the study participants are in a state of subclinical hypothyroidism (TSH 5.5-10 mIU/L–25.3% and TSH above 10 mIU/L-26.4%) that may go into full blown hypothyroidism within a few years. It has been shown that subclinical hypothyroidism with TSH concentration more than 10 mIU/L has been associated with increased risk for coronary artery disease. A meta-analysis study that included 2500 participants showed an increased risk of coronary artery disease and mortality in those with high TSH levels particularly above 10 mIU/L. Literature review reveals that with the advent of iodine supplementation across the world, autoimmune thyroid disease has become the most common cause of hypothyroidism [18]. The limitation of our study is anti TPO antibodies in the study population was not measured. Hence, future studies should focus on the measurement of thyroid antibodies along with thyroid hormone tests to know the actual status of thyroid dysfunction among the study population and the study subjects has to be followed up to understand the development of overt hypothyroidism and other complications.
Our study showed a higher prevalence of metabolic syndrome and subclinical hypothyroidism among the study population. Hence there is a need to assess the metabolic components and thyroid profile as a routine analysis in the study area. The association of components of metabolic syndrome and dietary pattern among the study population has to be studied to protect them from complications of diabetes and associated diseases. Future studies should focus on measuring anti TPO antibodies which may throw light in finding the cause for the increasing prevalence of subclinical hypothyroidism.
Citation: Krishna B, Dhas PK, Bettina J, Krishna NR (2021) Prevalence of Metabolic Syndrome and the Pattern of Thyroid Dysfunction among North Coastal Andhra Population. Thyroid Disorders Ther 10:264.
Received: 04-Nov-2021 Accepted: 18-Nov-2021 Published: 25-Nov-2021
Copyright: © 2021 Krishna B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.