Journal of Depression and Anxiety
Open Access
ISSN: 2167-1044
ISSN: 2167-1044
Research Article - (2020)Volume 9, Issue 4
Introduction: Diabetes is a known cause of, disability, morbidity, premature death and increased health-system costs. Previous research has shown that there is high prevalence of depression in patients with type 2 diabetes as compared to people without diabetes but there is a lack of data for Pakistan.
Objective: To determine the presence of depressive and anxiety symptoms in adults with type 2 diabetes and without diabetes.
Methods: A questionnaire-based descriptive cross-sectional study was carried out at AIMS Sugar Hospital, Hayatabad, Peshawar, Pakistan, 2018-2019. We used Patient Health Questionnaire (PHQ-9) and General Anxiety Disorder (GAD-7) scale for data collection, on a consecutive sample of patients.
Results: A total of 1157 subjects were interviewed face to face, to fill PHQ-9 and GAD-7 questionnaires in Pashto (locally spoken language). More than three quarters (77%) of the study population had known type 2 diabetes and 23% (264) were healthy individuals. Of the 1157 subjects, 893 (55%) were males and 264 (45%) were females. The mean (S.D.) age of study participants was 46.2 ± 14.1years (range 25-74 years). Both, PHQ- 9 and GAD-7 score, showed high prevalence of mild (34% vs. 12%, moderate (17% vs. 5%) and moderately severe/severe (8% vs. 5%) depression, symptoms and mild (25% vs. 13%), moderate (19% vs. 6%) and severe (8.6% vs. 4.5%) anxiety symptoms in diabetes group as compared to control group. We found that females in diabetes group were more likely to have depressive symptoms as compared to male patients (p<0.01, Pearson Chi Square test). Increasing age (>50 years of age) was not associated with depressive and anxiety symptoms as compared to younger age (<50 years of age) in both control and diabetes group (P=0.3181and P=0.431, respectively,). Similarly, we did not find any statistical association between duration of diabetes and severity of depressive and anxiety symptoms (P=0.561).
Conclusion: High prevalence of depressive and anxiety symptoms were reported by patient with diabetes and female gender was more affected than males. The psychosocial wellbeing of patient with diabetes should be taken into consideration during their consultation and need regular monitoring of depressive illness and anxiety disorder in primary healthcare settings in Pakistan.
Depression; Anxiety; Type-2 diabetes
Diabetes is a known cause of premature death, disability, morbidity, and increased health-system costs [1]. Currently type 2 diabetes is on rise due to aging population, sedentary life style and obesity. Around 400 million people worldwide having diabetes and this number is expected to rise up to 592 million by 2035 [2]. Patients with chronic medical conditions such as diabetes are 2-4 times more likely to have depression as compared to those with no diabetes [3,4]. Research studies have shown that up to 40% patients with diabetes have depression [5,6]. Both diabetes and depression represent 8th and 4th cause of disability adjusted life years, worldwide, respectively [7]. Depression is a leading cause of disability and a major contributor to the overall global burden of disease worldwide. Around 300 million people of all ages are affected with depression [8]. Depression can affect lives adversely with poor functionality at work, school and within the family as well as at worst can lead to suicide. Around 800,000 people die due to suicide every year and is the leading cause of death in 15- 29- years old. Depression is also a large burden on most economies [9] and leads to increased mortality [10,11]. Depression is a recurrent disorder with many risk factors. Such risk factors include comorbidities with other chronic conditions [12], other mental illnesses [8], positive family history of depression and mental illness, childhood adverse events [13], past history and treatment of depression, lack of physical activity, female gender, younger adults, smoking and unhealthy eating habits [13].
Research studies have claimed that diabetes precedes the risk of developing depression because of psychological trauma of the diagnosis of diabetes and its associated burdens, for example hyperglycemia/ hypoglycemia and its related complications and treatment, causing significant challenges for clinical practice [14,15]. However, this notion was challenged by a longitudinal studies results, that depression can be a risk factor for diabetes [14,16] and that diabetes may be modestly associated with depression [15]. Similarly incidence of diabetes were reported in patients with depression by a number of systematic reviews and meta-analyses [17-21] oppose to diabetes as a risk factor for depression [19,22- 25]. Recent studies have reported a bidirectional relationship of diabetes and depression as comorbidities existing simultaneously [26-29].
Depression is also associated with hyperglycemia (higher glycated haemoglobin, HbA1c; [30,31]), increased morbidity & complications [32,33], mortality and healthcare costs [3,34]. Such association may be linked with sub-optimal self-care [35], noncompliance to medication, [36], and poor health-related quality of life [37]. Appropriate diagnosis and treatment of depression in diabetes can improve quality of life, better glycemic control and wellbeing with improve social interaction of patients in general with family, friends and careers [38,39].
AIMS Sugar hospital presented our ‘diabetes circle of care’ and complications data in IDF [40], which highlighted high (77%) reporting of depressive and anxiety symptoms in our out-patient population (male and female together, and 88% in female as compared to 22% in male). Therefore, current study was designed to collect data specifically on depressive and anxiety symptoms in our diabetes patients as compared to people with no diabetes or other comorbidities.
A questionnaire-based descriptive cross sectional study was carried out at AIMS Sugar Hospital, Hayatabad, Peshawar, Pakistan between 1st November 2018 to 31st January 2019. Study subjects were recruited from our diabetes out-patient department (as diabetes group) and their relatives (as control group), as a consecutive sample, to participate in the study. Adults (age ≥25 years) with known type 2 diabetes were included in the study group and the control group was consisted of adults (age ≥25 years) with no known history of diabetes. Ethical approval was taken from AIMS ethics committee. Written consent forms was signed by all participants.
We used PHQ-9 and GAD-7 for data collection through face to face interview with study subjects during their visit to the hospital. Statistical analysis were carried out using SPSS-21.
The Patient Health Questionnaire-9 (PHQ-9) is a short self-report screening tool used more commonly in the primary healthcare settings, to screen people with major depression as well as assess the severity of depressive symptoms. It has a high internal consistency (Chronbach's alpha 0.86 and 0. 88) and high testretest reliability (Chronbach's alpha 0.84 and 0.95; [41,42]). A total score of 0-4 represents minimal or no depression, 5-9 represents mild symptoms of depression with minimal intervention and no medication required. Scores of 10- 14 represent moderate depressive symptoms, and they may benefit psychological interventions such as brief counselling, cognitive behavioral therapy (CBT) or interpersonal psychotherapy/ However scores of 15-19 represent severe depression symptoms which needs treatment along with or without psychological interventions. Scores above 20 shows severe depression that needs urgent referral to mental health services and treatment.
Major depression was calculated if any 5 or more than 5 items were cited as “at least more than half the days” (2) plus either 1a or 1b was positive as “at least more than half the days” (2) on the PHQ-9 questionnaire. While minor depression was calculated if 1b, 1c or 1d was cited as “at least more than half the days” (2) plus either 1a or 1b was positive as “at least more than half the days” (2). The General Anxiety Disorder-7 (GAD-7) is a 7 item based self- administered screening tool, used to measure the severity of generalized anxiety disorders, and also a reliable screening tool for panic, social anxiety and post-traumatic stress disorder [43]. The GAD-7 has good internal consistency (Chronbach's alpha 0.89- 0.92), good convergent validity [42] and sensitivity of 83–89% [44].
GAD-7 has seven items, each item ask the individual to rate his/her symptoms over the past 2 weeks (GAD-7 questionnaire). Subjects’ response can be one of these, not at all (0), several days (1), more than half the days (2) and nearly every day (3). Scores between 0-4 indicate minimal or no anxiety, 5-9 indicate mild anxiety, 10-14 indicate moderate anxiety (needs further evaluation) and scores 15 and above are indicative of severe anxiety and treatment needs to be initiated if patent is not taking anxiety medication.
A total of 1157 subjects were interviewed face to face, to fill PHQ-9 and GAD-7 questionnaires and were included in the study. Seventy seven percent (893), study population was patient with known type 2 diabetes (diabetes group) and 23% (264) were healthy individuals (control group). Of the 1157 subjects, 523 (45%) were females and 634 (55%) were males. Average age (S.D.) for the study population was 46.2 (±14.1) ranged from 25-74 years. Patients with diabetes were comparatively older (50.1 ± 11.7) than healthy individuals in the control group (31.7±11.3) (Table 1).
| Variables | Depression (PHQ-9) | Anxiety (GAD-8) | |
|---|---|---|---|
| Group | Diabetes Group | 551/893 (61.7%) | 475/893 (53.2%) |
| Control group | 58/264 (21.9%) | 61/264 (23.1 %) | |
| Gender | Males | 190/551 (34.5%) | 110/475 (23.2 %) |
| Females | 361/551 (65.5%) | 365/475 (76.8 %) | |
| Age | <50 years | 303/551 (55%) | 271/475 (57%) |
| =50 years | 248/551 (45%) | 204/475 (43%) | |
| Duration of diabetes | <1 year | 215/551 (39%) | 171/475 (36%) |
| 1-10 years | 176/551 (32%) | 162/475 (34%) | |
| >10 years | 160/551 (29%) | 142/475 (30%) | |
Table 1: Characteristics of study population and distribution of depression and anxiety symptoms.
Depression was reported by 52.6% (609) of the total study population (point prevalence) as compared to 47.4% (548) of study subjects reported no symptoms of depression on PHQ-9 scale. Major depression was noted in 274 (23.7%) as oppose to minor depression in 335 (28.9%) study subjects.
Between-group analyses have shown that statistically high number of patients (551/893, 61.7%) in the diabetes group reported symptoms of depression as compared to the control group (58/264, 21.9%, respectively, P 0.001, Pearson Chi Square test (Figure 1).
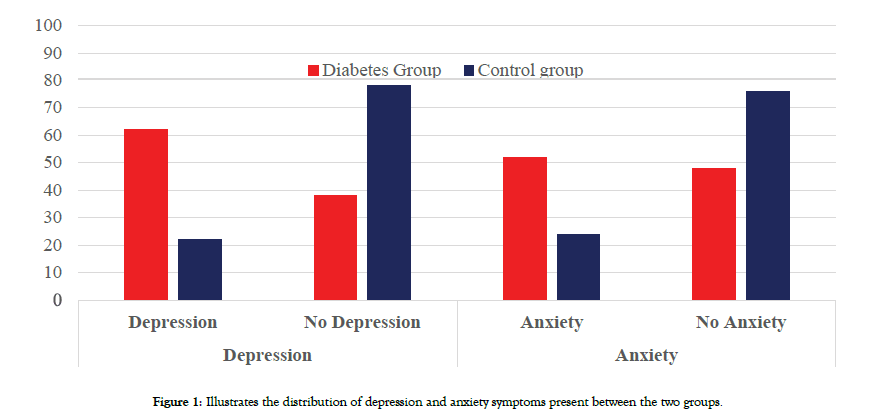
Figure 1: Illustrates the distribution of depression and anxiety symptoms present between the two groups.
Similarly, according to GAD-7 scale, 46.5% of our study population (539/1157) reported anxiety as compared to 53.5% (618/1157) with no anxiety. Among subjects reported anxiety, majority of the subjects’ indicated mild anxiety symptoms (257/539, 48%), as compared to severe anxiety symptoms in 17% (89/539) and 35% (193/539) had shown moderate anxiety symptoms.
Between-group comparison have shown that anxiety was reported significantly among the diabetes group (475/893, 52%) as compared to the control group (64/264, 24%, P 0.001, Pearson Chai Square test, Figure 1).
Within-group analysis have shown that Female gender (361/551, 65.5%) was significantly associated with depression as compared to males (190/551, 34.5%) in diabetes group (P< 0.01, Pearson Chi Square test). However female gender was not associated with depression in our control group (29/58, 50% vs. 29/58, 50%; Figure 2). Figure 3 illustrates the distribution of depressive and anxiety symptoms in a flow chart, between the two groups according to the gender.
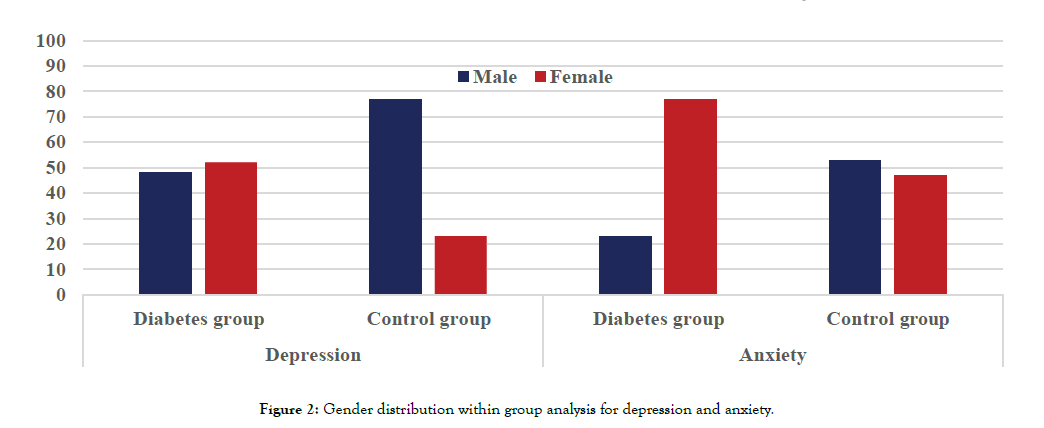
Figure 2: Gender distribution within group analysis for depression and anxiety.
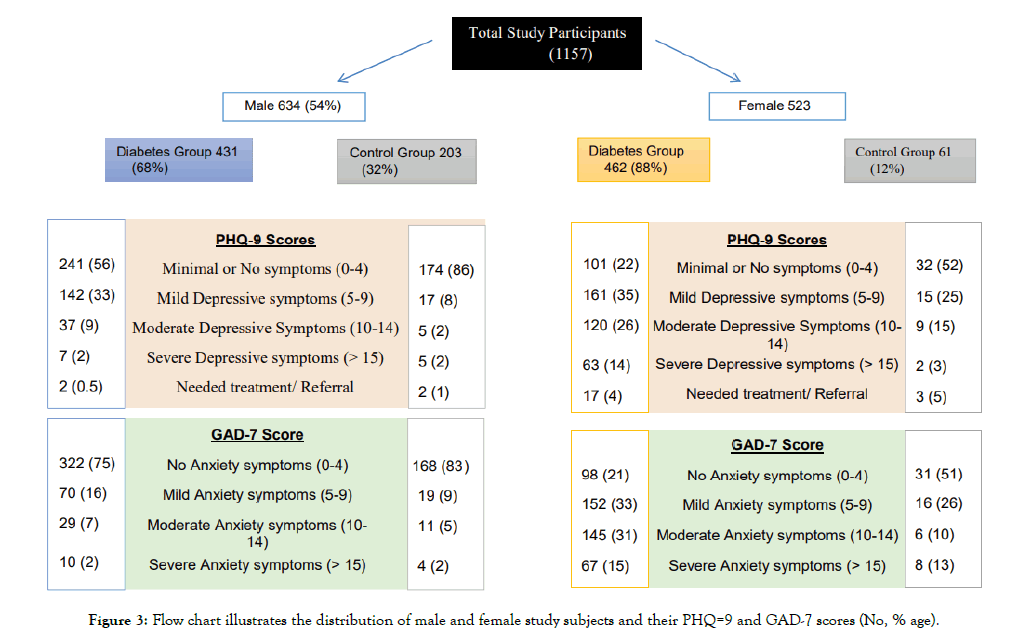
Figure 3: Flow chart illustrates the distribution of male and female study subjects and their PHQ=9 and GAD-7 scores (No, % age).
Within-group analysis of the diabetes group demonstrated that statistically significant number of female patients with diabetes reported symptoms of anxiety (364/475, 77%) as opposed to male patients in the same group (109/475, 22.8%, P 0.001, Pearson Chi Square test). On the other hand, in the control group anxiety symptoms were reported equally by male and female subjects (30/64, 47% and 34/64, 52%, respectively.
Within-group analysis showed that increasing age (>50 years of age) was not statistically associated with high depressive and anxiety symptoms as compared to younger age (<50 years of age) in diabetes group (P=0.3181 and P=0.431, respectively, Pearson Chi Square test).
Similarly, within-group analysis indicated, no statistical association between the duration of diabetes and presence of depressive and anxiety symptoms (P=0.561, P=0.514, respectively, Pearson Chi Square test).
Major study findings
Our studies have shown higher proportion of depressed and anxious adults in the diabetes gas compared to the control group (without diabetes). Also we found that female gender is associated with high proportion of depressive and anxiety symptoms in both groups. Duration of diabetes has no effect on psychological symptoms in our study population. Therefore, psychological symptoms screening should be considered in the treatment of patients with diabetes, since it can effect on treatment process and outcome as well as the quality of life.
Comparison of finding with previous research
Previous research have shown similar results, that patients with diabetes have high prevalence of depression 14.7% (CI 6.6-22.8) as compared to patients without diabetes 4.9 (CI 3.7-6.1, [45]). Also higher prevalence of depression was reported in female 5.4% (95% CI: 4.2-6.6) as compared to male patients [45]. Similarly, Khan et al. [46] have shown high prevalence of depression (60%, 84 out of 140 patients in type 2 diabetes). In comparison to Naseem et al. [45] findings, our diabetes group have shown higher prevalence of depressive symptoms; more than 60% as compared to 23% in the control group which are in consistent with Khan et al. [46] findings, irrespective of different screening tools were used for depression screening.
Furthermore female gender was found more vulnerable to psychological symptoms as compared to male by different studies [46,47]. Our study findings are in agreement with Khan et al. [46], showing that more than 65% of our female patients with diabetes reported depressive symptoms as compared to 34.5% males’ patients with diabetes, whereas Khan et al. [46] study found 68% of females as compared to 31% males patients with diabetes has depression. Such high occurrence of depression in female gender could be associated with their social role such as passivity and dependence and comparatively high emotional expression behavior in women as compared to men [46,47]. Irrespective of the definite etiology of depressed mood in women, it adversely affects their lives, physically, emotionally and socially in the society.
Our results have shown no statistically significant association between the duration of diabetes and depressive/ anxiety symptoms in our adult diabetes population. However, research have shown that generally immediately after the new diagnosis of diabetes there is an increase in depressive symptoms which gradually reduce over period of time for few years and then reoccurrence of psychological symptoms are associated with longer duration of disease, like a J-shape curve [48] found that odds of depression is high in patients with diabetes when duration of diabetes was less than 10 years and more than 30 years, while there was no significant associated when duration of diabetes was 10-30 years in their study. Similarly, Arshad et al [49] have shown that 40% of their study population was depressed with shorter duration of diabetes, using PHQ-9 questionnaire, indicative of increase depression in early diabetes. The relationship of various chronic medical conditions and symptom of depression, and found no significant increase in depressive symptoms after initial diagnosis, however their research have shown that there was a gradual increase in psychological symptoms over period of time, in accordance with Darwish et al. [48] J-shaped curve model. In addition to above, Hood et al [50], reported a peak in depressive symptoms at baseline (initial diagnosis), with a gradual decline over next few years, and an increase in psychological symptoms with longer duration of diabetes in their study, suggestive of J shape-curve model of depressive symptoms in diabetes. Although such an increase of depressive symptoms with initial diabetes diagnosis is not fully investigated but such psychological symptoms might be related to distress caused by the new diagnosis and its lifelong treatment routine, blood testing’s along with diet and exercise regimens [51]. Also, incidence of depressive symptoms were reported with initiation of anti-diabetes oral medication in the first year and after adjustment to medication routines with no diabetes related complications in the following few years, there were improvement in symptoms [52-54].
Our within-group analysis showed that increasing age (>50 years) in diabetes group was not significantly associated with depressive/ anxiety symptoms. Previous studies have shown that increasing age in patients with diabetes is associated with less psychological symptoms as compared to younger age, however the relationship between age and risk of depression in diabetes is multifactorial [53,55]. Berge et al. [56] conducted a population based cross sectional survey and found that patients with diabetes in their forties are twice depressed relative to patients with no diabetes in the same age group. Also they found that patients with diabetes who are on oral anti-diabetes medication are three to five times more depress and using anti-depressants, respectively. Association between diabetes and depression with respect to age is complex and other factors such as physical inactivity, diabetes complications, HbA1c and glucose control, BMI (body mass index), low educational level and socioeconomic class would contribute negatively. Also relatively low risk of psychological symptoms in older patients with diabetes as compared to younger patients could be related to better coping mechanism and experience of managing their disease with time (duration of diabetes).
Study tool used for psychological assessment
Screening for psychological symptoms in diabetes is recommended by many clinical guidelines [57,58]. A range of questionnaires is available to asses’ depressive symptoms. Research have shown that the Beck Depression Inventory (BDI), the Patient Health Questionnaire-9 (PHQ-9), Center of Epidemiological Studies- Depression Scale (CES-D) and the Hospital Anxiety and Depression Scale-Depression (HADS-D) are frequently used tools for depression identification in patients with diabetes at primary care level [29,59,60].
Questionnaires effectiveness for depressive symptoms identification are usually assed by reliability, validity, and responsiveness [29]. A reliable questionnaire will have minimum measurement error, while validity is the ability to measure the intended construct, and a good responsive questionnaire shows sensitivity to any changes in the construct [61]. In addition to above, it is crucial questionnaire has to give clinically meaningful outcomes, interpretability [61]. PHQ-9 and GAD-7 scales were found to be valid and reliable tools to screen, rate and monitor outcomes of depressive illness and anxiety disorder in primary healthcare settings in Pakistan.
Our study limitation is possible selection bias, as we included every consecutive patient who consented to participate in the study with or without their relative (as a control) from our out patients department. Therefore our groups (diabetes and control) were not equally distributed, due to less participation rate by the relatives (22.8%).
Previous studies have demonstrated that patients with severe psychological symptoms are less likely to participate in surveys [61] and high prevalence of depression was noted in non-participants relative to participating patients [62]. However, the above case is more likely to underestimate the prevalence of depressive/ anxiety symptoms rather than reducing the validity measure between the diseases (diabetes and psychological symptoms, [62]).
Finally, in our study, we did not assess the confounding factors for psychological symptoms which can affect patients with diabetes negatively such as their treatment history (oral treatment vs. Insulin injections), HbA1c level, presence of diabetes related complications, socioeconomic history and educational level.
We excluded all those participants, who were on anti-depressants currently or have used treatment for psychological symptoms in the past, as it can reduces the specificity of our measure of psychological symptoms (depression and anxiety). But we did not collect data for other existing medical conditions like asthma, heart disease or gastrointestinal disorders, both in diabetes and control group.
The bidirectional relationship between diabetes and depression is not very clear but the two chronic conditions occurring together can create difficulty in managing both conditions and their associated long term effects such as stroke, dementia and mortality. Identification of psychological symptoms in patients with diabetes, in primary care settings, is important and also appropriate treatment with establish pathways for referral are mandatory to avoid further worsening of both conditions by primary care physicians. From public health perspective, it is important to initiate preventive strategies, at primary care level, to reduce the prevalence and impact of depression comorbid to diabetes.
Citation: Hasan A, Zia S, Amanullah Y, Nisa F, Maracy M, Hasan Z (2020) Prevalence of Depressive and Anxiety Symptoms in Adults with Type 2 Diabetes, Peshawar, KPK, Pakistan. J Depress Anxiety. 9:369. doi: 10.35248/2167-1044.20.9.369
Received: 24-Jun-2020 Accepted: 28-Aug-2020 Published: 05-Sep-2020 , DOI: 10.35248/2167-1044.20.9.369
Copyright: © 2020 Hasan A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.