Internal Medicine
Open Access
ISSN: 2165-8048
ISSN: 2165-8048
Research Article - (2021)
Objective: To determine the prevalence of E.coli causing Urinary Tract Infection (UTI) in JMCH during one year 2020-2021. To determine the resistance and sensitive drugs acting on E.coli.
Background: Most frequently, Urinary Tract Infection (UTI) infection is caused by E.coli, requiring urgent medical attention. Normally E.coli lives abundantly in rectum but when this bacterium comes in urethra it can cause UTI’s.
Methods: The retrospective study included 538 patients of which 261 were males and 275 females were admitted to Jinnah Medical College Hospital, Karachi between February 2, 2020-January 20, 2021. The ages, gender, presence of E.coli along with sensitivity and resistance against drugs were recorded and analyzed using SPSS version 16.
Results: Of the 538 patients, 261 (48.5%) were males and 275 (51.1 %) were females. The age range was from 1-100 years with mean age between 40.07 years and mean SD ± 20.105. The female to male ratio was 0.95. Of the 538 patients, 102 were infected with E.coli. The most sensitive antibiotics against E.coli was Imipenem (87 patients), Fosphomycin (80 patients) nitroflurantoin (59 patients), Tazobactam (56 patients). The most resistant antibiotic against E.coli were amoxacillin+clavulinic Acid (83 patients), Septran (75 patients), Cefuroxime (72 patients), Ceftriaxone (59 patients). Prevalence of E.Coli during 1 year was 18.9%.
Conclusion: E.coli infection is high in females in the study region. E.coli is most sensitive to Imipenem and most resistant to amoxacillin+clavulinic Acid. UTI can be prevented by good personal hygiene and drinking plenty of water. UTI’s are easy to treat if proper diagnosis is made.
Antibiotics; E.coli; Resistance; Sensitivity; Urinary Tract Infections.
Urinary Tract Infection (UTI) is a condition in which bacteria grow in the urinary tract and it is the most common bacterial infection. These bacteria can gain access to the urinary tract through the skin, from sexual transmission and from birth control devices. If kidneys and ureters are involved it is known as upper urinary tract infection [1]. Escherichia coli is a gram-negative, rod-shaped bacterium that is commonly found in the lower intestine of warm-blooded organisms (endotherms). Anti-Microbial Resistance (AMR) is resistance of a microorganism to an antimicrobial medicine to which it was previously sensitive.
Many of the widely used antibiotics were resistant to the E. coli isolates, including amoxicillin, gentamicin, cotrimoxazole, augmentin, ciprofloxacin, norfloxacin, streptomycin, and nalidixic acid. All 50 E. coli isolates tested were resistant to penicillin and erythromycin (100%); 49 (98%) were resistant to nalidixic acid, 47 (94%) to cephalexin, 43 (86%) to amoxicillin, 42 (84%) to ampicillin, 37 (74%) to ciprofloxacin, 32 (64%) to tetracycline, 27 (54%) to cefixime, and 18 (36%) to gentamicin. Fosfomycin is an oral antibiotic that exhibits wide antimicrobial efficacy against Multi-Drug Resistant (MDR) bacteria, including E.coli that produces Extended Spectrum Beta-Lactamases (ESBL). Misuse and overuse of antibiotics, as well as poor infection prevention and control, all contribute to antibiotic resistance. At all levels of society, measures can be made to decrease the impact and spread of resistance.
Classic symptoms of UTI’s include painful micturation, increased frequency of urination, backache, bleeding from urethral tube, fever and smelly urine. Most common urinary tract infections are also caused by, but less commonly by, Staphylococcus, Klebsiella, Proteus and Pseudomonas. Women have a greater chance of having UTI’s because urethra is close to anus and it is shorter [2,3]. E.colilives abundantly in the rectum but when this bacterium comes in the urethra it can cause Urinary Tract Infection (UTI).
E.coli can either be single drug resistant or they can be multi drug resistant. The standard regiment for Urinary Tract Infection (UTI) treatment is Trimethoprim-Sulfamethoxazole (TMP-SMX), but lately quinolone has been prescribed to treat UTI’s Sometimes a combination of amoxicillin-clavunate (Augmentin) is administered for drug-resistant infections [4]. One mechanism by which E.colibecome resistant are “genetic sequence of events that lead to multi drug resistant phenotypes of Gram-negative bacteria” [5]. Extended-spectrum beta lactamases an enzyme that is produced by multi drug resistant E.colimay be another reason why certain anti-microbial drugs do not work. Another cause may be due to concomitant infection with other bacteria or virus. Indiscriminate use of antibiotics is may be another cause of resistance in different E.colistrains [6].
We retrospectively analyzed 538 patients of age 1-100 years that were admitted to Jinnah Medical College Hospital, Karachi between February 2, 2020 and January 20, 2021. Our source of data was from JMCH laboratory consisting of Urine D.R. (culture reports) which mentioned the age, gender, and sensitivity and resistance to different bacteria. The inclusion criteria were laboratory reports that came positive with E.coli. Statistical analysis was performed using SPSS version 16.0 [7].
The urine culture reports were stratified based upon the growth of bacteria. E.coli had the greatest prevalence, followed by Enterococcus and Staphylococcus (Figure 1). Majority of the urine culture reports showed growth of no organism. Prevalence of bacteria causing UTIs was calculated. All the urine culture reports of E.coliwere reanalyzed and sensitivity and specificity of each antibiotic was recorded. In cases where lab report did not mention any particular antibiotic, we recorded it under category of missing data. Antibiotics that were mentioned on the urine culture reports included imipenem, septran, ceftazidine, ceftriaxone, norfloxacin, ciprofloxacin, ofloxacin, enrofloxacin, levofloxacin, tobramycin, tazobactam, gentamicin, maxifloxacin, fosfomyhcin, amoxicillin+clavulanic acid, cefuroxime, cefixime, cefotaxime and cefeperzone. We analyzed and recorded the results of sensitivity or resistance for each of the antibiotics mentioned above.
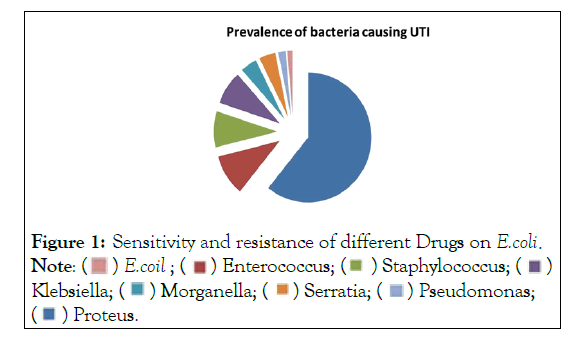
Figure 1: Sensitivity and resistance of different Drugs on Ecoli. 

Of the 538, 261 (48.5%) were males and 275 (51.1 %) were females. The age rage was from 1-102 years with mean age between 40.07 years and mean SD ± 20.105. The female to male ratio was 0.95. Prevalence of E.coli during 1 year was 18.9 % (Figure 1). The most sensitive antibiotics against E.coli were Imipenem (87 patients), Fosphomycin (80 patients) nitroflurantoin (59 patients) and Tazobactam (56 patients). The most resistant antibiotic against E.coliwere amoxacillin+clavulinic Acid (83 patients), Septran (75 patients), Cefuroxime (72 patients) and Ceftriaxone (59 patients) (Table 1).
| Name of drug | Missing data | Sensitive | Resistance | Intermediate |
|---|---|---|---|---|
| Imipenem | 10 | 87 | 3 | 2 |
| Septran | 17 | 7 | 75 | 3 |
| Ceftazidime | 25 | 31 | 45 | 1 |
| Ceftriaxone | 11 | 31 | 45 | 1 |
| Norfloxacin | 3 | 17 | 80 | 2 |
| Nitrofurantoin | 2 | 59 | 30 | 11 |
| Ciprofloxacin | 9 | 19 | 71 | 3 |
| Ofloxacin | 56 | 21 | 24 | 1 |
| Enrofloxacin | 57 | 10 | 34 | 1 |
| Levofloxacin | 53 | 11 | 36 | 2 |
| Tobramycin | 51 | 14 | 28 | 9 |
| Tazobactam | 15 | 56 | 22 | 9 |
| Gentamicin | 43 | 18 | 37 | 4 |
| Moxifloxacin | 53 | 12 | 37 | 0 |
| Fosfomycin | 3 | 80 | 16 | 4 |
| Amoxicillin+clavulanic acid | 2 | 10 | 83 | 8 |
| Cefuroxime | 5 | 18 | 72 | 8 |
| Cefixime | 45 | 24 | 34 | 0 |
| Cefotaxime | 66 | 22 | 14 | 0 |
| Cefoperzone | 60 | 16 | 14 | 0 |
Table 1: Sensitivity and resistance of different Drugs on E.coli.
While our research was under progress new drugs were included and some drugs were removed that were included in our list. This could have compromised the efficacy of the result. The missing data from some reports could have been another reason for misconstrue results [8].
In our study E.coliwas positive in 102 patients out of 166 positive for Urinary Tract Infection (UTI) at 61.44%. E.coliwas detected at 80% in other retrospective studies [9]. This means that the demographic setting for our study reflects the same demographic trends internationally according to other studies. It also signifies that, though our study was situated in a tertiary care hospital, the results depicted and matched with recent studies which took place in other countries some of which were conducted for 10 extensive years.
Correct diagnosis and prompt treatment of Urinary Tract Infection (UTI) is vital in reducing morbidity. Unnecessary treatment in cases of asymptomatic bacteriuria is associated with increased risk of subsequent symptomatic UTIs, except in certain circumstances. Oral antibiotics are recommended treatment option in cases of simple uncomplicated cystitis. In cases of complicated UTIs, antibiotics usage should always be guided by urine culture in order to avoid any development of resistant strains. In cases of complicated UTIs, hospitalization is often required and treatment for 7-14 days is generally recommended [10].
Increased usage of antibiotics has led to formation of increased resistant strains of bacteria which has led to development of novel therapeutic options for the treatment of UTIs. Newer therapeutic agents aim to target pili/fimbria and block bacterial adhesion [11]. These classes of medication are called pilicides. Usage of new vaccination has been studied in mice and cynomolgus monkeys. The vaccination resulted in 99% reduction in mucosal colonization and 75% reduction in both inflammation and mucosal colonization [12].
In our study we discovered that E.coliwas most resistant (81.3% patients) against amoxacillin+clavulanic acid. In other studies, E.coliwas more sensitive against amoxacillin+clavulanic acid (41.6% patients). This may be due to cover prescription of the drug or easy availability which could have led to increased immunity of E.coli against this drug and may have led to development of new resistant strains of E.coli. Increasing the threat of random error due to patient recruitment in a laboratory setting, overall E. coli resistance rates in Dakar seemed to be significantly high, with the confirmation of the emergence of multidrug-resistant strains. Total management of antimicrobial various drugs in pharmacies and among vendors, reinforcement of therapeutic guidelines and infection control strategies, dissemination of information about antibiotic use and drug resistance, and continued support of large antimicrobial susceptibility studies are now all possible strategies.
Most of the UTI’s caused by E.coliwhich was most prevalent could have been prevented by careful monitoring of drug prescription along with undertaking proper hygienic measures. Heath education programmes regarding UTI’s should be encouraged. This would improve the quality of life among population in general and females in particular. Our study is the first to present data from a developing country on the risk factors for urinary tract infection caused by E.coli strains resistant to widely used antibiotics.
Citation: Razi S, Younas Z (2021) Prevalence of Antibiotic Resistant E.coliCausing Urinary Tract Infection in Jinnah Medical College Hospital. Intern Med. S8 :003.
Received: 02-Sep-2021 Accepted: 09-Sep-2021 Published: 30-Sep-2021 , DOI: 10.35248/2165-8048.21.s8.003
Copyright: © 2021 Razi S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : Antibiotic-Resistant