Journal of Pharmaceutical Care & Health Systems
Open Access
ISSN: 2376-0419
ISSN: 2376-0419
Research Article - (2021)Volume 8, Issue 5
Background: Acute Kidney Injury (AKI) is a common illness especially among critically ill patients. The incidence is 2-3 cases per 1000. Seventy percent of the cases are found in the Sub-Sahara African. The proportion of drug- induced AKI is about 25%. Hence there is a need to identify the medication related problems in AKI patients which will facilitate identification, prevention and improved patient outcomes.
Objective: To establish the prevalence and determinants of medication related problems in patients with AKI at Kenyatta National Hospital.
Methods: This study was a cross-sectional survey that was conducted among patients with AKI at Kenyatta National Hospital. Consecutive random sampling was used to select 92 participants. Data was collected using researcher administered questionnaire and analyzed using STATA version 15. The level of significance was set at p ≤ 0.05.
Results: The average age of the participants was 51(± 15.96) years. Medication related problems (57, 62%) identified were associated with the severity of AKI (p=0.014) with the most prevalent being over dosage (59, 64.1%, p=0.002) and drug-drug interactions (44, 47.8%, 0.037). Acute decompensated heart failure (25, 27.2%) was more prevalent comorbidity followed by Obstructive uropathy (18, 19.5%). The main independent predictors of AKI severity were alcohol use (p=0.021), drug overdose (p=0.001) and obstructive uropathy (p=0.014).
Conclusion and recommendations: Medication related problems as a precipitating factor of AKI cannot be underscored particularly in the presence of comorbidities. It is therefore recommended that AKI management protocols and policies be developed to address the gaps and involve pharmacists in the bedside medication management.
Obstructive uropathy; AKI; AKI severity; Dosage problems
There is a growing global concern over the rising cases of AKI in recent years affecting both low and high-income countries with an incidence of 2-3 cases per 1000 persons [1,2]. AKI is severe in Sub- Saharan Africa with 70% affected found in critical care settings. This increases the morbidity and mortality to about 84% if the victims are not dialyzed [3]. The disease is characterized by an abrupt deterioration of kidney function. There is rise in serum creatinine, urea, and dysregulation of extracellular volume and electrolyte imbalance. These may occur with or without other organs being damage [4,5]. Risk factors associated with AKI includes a history of hypotension, sepsis and the aged population [6,7].
Medication Related Problems (MRPs) is anything involving drug therapy that interferes or has the potential to interfere with the desired outcome for a patient [8]. They are either clinician or patient related [9]. These problems may arise from patient medication experience or prescription preparation. Nephrotoxic drugs account for about 25% of all the incidences of AKI [10]. With the rising burden of chronic diseases especially in developing countries, it is highly likely that these patients will use multiple drugs [11]. Knowledge gaps still exist among physicians and pharmacists as well as the variation in identifying AKI risk factors, nephrotoxic drugs, and risk assessment [12]. Locally, Kenyatta national hospital admits several community-acquired or hospital-acquired AKI cases. More importantly, the facility lacks data to demonstrate the prevalence of MRPs associated with AKI. This study sought to explore the MRPs in patients with AKI which will inform the facility policy makers on the present burden and give useful recommendations that will improve medication use in the facility.
Study design
This was a cross-sectional study design involving 92 participants diagnosed with AKI selected by consecutive sampling method at Kenyatta National Hospital which is the largest teaching and referral hospital in the Kenya.
Ethical consideration
Ethical approval was obtained from the Kenyatta National Hospital/University of Nairobi Ethics and Research Committee (P147/02/2019) before the study began. Additionally, participants who agreed to participate signed the consent declaration form. Patient data were coded with a unique number.
Sampling and data collection
AKI patients aged 18 years and above were selected from the medical wards of KNH. Potential participants were identified from the files and recruited after admission and having received standard of care. The sample size was determined using Fischer’s formula and corrected using the finite population where a sample size of 92 was obtained. This was based on the study population which had an average of 120 patients per months suffering from AKI. The cases of AKI were defined by rise of creatinine levels by at least 1.5 X (times) from the baseline within 7 days or by 26.5 umol/L within 48 hours. The severity of AKI was defined as mild if creatinine levels is 1.5 to 1.9 X above the baseline levels or 26.5 umol/L while moderate being 2.0-2.9 X and severe above 3.0 X above the baseline. Recruitment was done by simple random sampling method on patients who met the inclusion criteria and gave consent by signing the consent declaration form. Patient demographic information was obtained followed by the clinical data. Thereafter information of medication uptake which included dosage and drug interactions was collected from the patient files. This was done until the desired number was achieved.
Data processing and analysis
Data obtained was fed in a pre-structured Epi-info version database which was exported to excel sheet and copied to Stata version 15 for analysis. Continuous variables were summarized into mean and standard deviation while categorical viable into frequency and percentages. Associations between the dependent variable (severity of AKI) and predictive variables (sociodemographic characteristics, comorbidities, and medication related problems) were determined using bivariate analysis (chi-square and fisher exact). Forward stepwise multiple logistic regression analysis was used to determine the independent predictors of AKI severity. All the data was analyzed against p<0.05 level of significance.
Sociodemographic characteristics
The study had almost equal number of females (47, 51%) and males (45, 49%) males. The mean age was 51 (± 15.96) years and the range were 20 to 81 years (Table 1). Most participants had normal weight (55, 59.8%) followed by overweight. Those who had history of smoking and drinking alcohol were 22(23.9%) and 34(37%) respectively. The sociodemographic characteristics associated with the severity of AKI were gender (p=0.008), smoking (p=0.02) and alcohol intake (p=0.005).
| Variable | AKI severity (serumcreatinine) | p-value | |||
|---|---|---|---|---|---|
| Mild (X1.5) | Moderate (X2) | Severe (X3) | |||
| Gender | Male | 17 | 14 | 14 | 0.008* |
| Female | 25 | 3 | 17 | ||
| Age | <35 | 7 | 3 | 5 | 0.995 |
| 35-60 | 23 | 9 | 16 | ||
| >60 | 14 | 5 | 10 | ||
| BMI | <18.5 | 5 | 2 | 4 | 0.304 |
| 18.6-24.9 | 22 | 11 | 22 | ||
| 25-29.9 | 10 | 2 | 5 | ||
| >30 | 7 | 2 | 0 | ||
| Marital status | Married | 26 | 15 | 41 | 0.439 |
| Single | 5 | 2 | 3 | ||
| Smoking status | Nevers smoked | 38 | 9 | 23 | 0.020* |
| Current smoker | 6 | 8 | 8 | ||
| Alcohol status | Never drunk | 33 | 4 | 21 | 0.005* |
| Currently drinking | 11 | 13 | 10 | ||
Note: AKI: Acute Kidney Injury; * denotes Statistically significant values.
Table 1: Association of sociodemographic characteristics and severity of AKI (p=92).
Comorbidities
The blood pressure was normal in 40(43.5%) participants while low in 25(27.7%) and high in 27(29.3%) (Figure 1). Fifty-four (58.8%) participants had normal heart rate. Forty four (44.8%) respondents had mild and 31(33.7%) had severe AKI cases respectively. Acute decompensated heart failure (25, 27.2%) was the most prevalent. A statistically significant association was observed between the severity of AKI and obstructive uropathy (p<0.001).
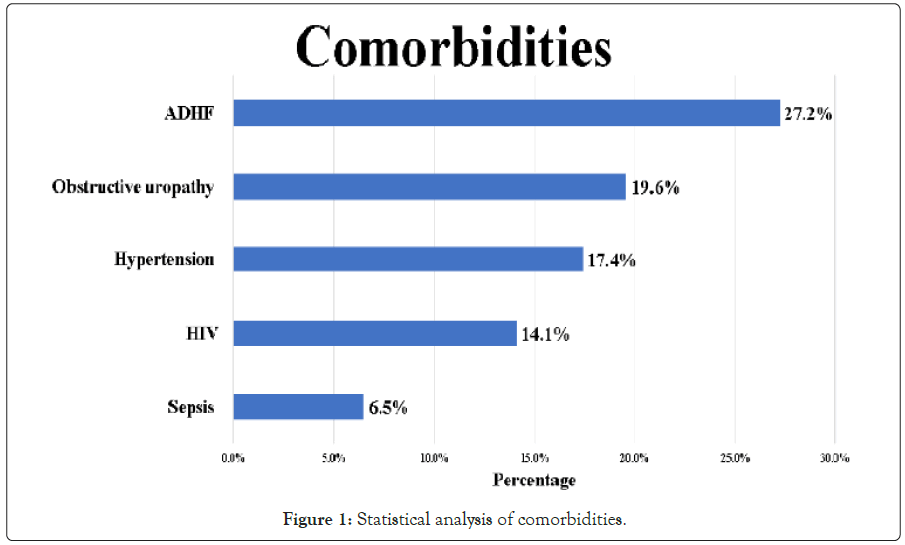
Figure 1: Statistical analysis of comorbidities.
Types of medication prescribed
The most prescribed medication was enoxaparin (43, 46.7%) and paracetamol (43, 46.7%) (Table 2). Ceftriaxone (23, 25%) and augmentin (17, 18.5%) were the preferred antibiotics while carvedilol (19, 20.7%) and enalapril (17, 18.5%) most used among the antihypertensives.
| Medications | Frequency (n) | Per (%) | p-value |
|---|---|---|---|
| Analgesics | |||
| Paracetamol | 43 | 46.7 | 0.329 |
| Tramadol | 14 | 15.2 | 0.799 |
| Morphine | 7 | 7.6 | 0.415 |
| Antibiotics | |||
| Ceftriaxone | 23 | 25 | 0.611 |
| Augmentin | 17 | 18.5 | 0.023* |
| Metronidazole | 11 | 12 | 0.020* |
| Ceftazidime | 7 | 7.6 | 0.269 |
| Gentamicin | 3 | 3.2 | 0.321 |
| Cotrimoxazole | 8 | 8.7 | 0.107 |
| Clarithromycin | 5 | 5.4 | 0.296 |
| Antihypertensives | |||
| Carvedilol | 19 | 20.7 | 0.006* |
| Enalapril | 17 | 18.5 | 0.016* |
| Amlodipine | 11 | 12 | 0.219 |
| Nifedipine | 8 | 8.6 | 0.343 |
| Diuretics | |||
| Furosemide | 29 | 31.5 | 0.079 |
| Spironolactone | 15 | 16.3 | 0.005* |
| Hydralazine | 5 | 5.4 | 0.675 |
| Antiplatelets | |||
| Aspirin | 14 | 15 | 0.001* |
| Clopidogrel | 6 | 6.5 | 0.013* |
| Statins | |||
| Atorvastatin | 19 | 20.7 | 0.003* |
| Anticoagulant | |||
| Enoxaparin | 43 | 46.7 | 0.057 |
| Antifibrinolytics | |||
| Tranexamic acid | 5 | 5.4 | 0.031* |
| Antiemetics | |||
| Metoclopramide | 23 | 25 | 0.007* |
| Ondansetron | 14 | 15.2 | 0.009* |
| Antifungal | |||
| Fluconazole | 3 | 3.2 | 0.793 |
| Amphotericin B | 2 | 2.2 | 0.611 |
Note: * denotes statistically significant values.
Table 2: Association between prescribed medication and AKI Severity (n=92).
Medication related problems
Of all the participants in this study 62 (67.4%) had medication related problems. In this study dosage too high was found to be significantly high hence we choose to analyze it. Of these participants 59 (64.1%) were on medication with dosage too high and the ones that had significant association with AKI severity included enoxaparin (20, 21.7%, p=0.006), metoclopramide (13, 14.1%, p=0.016), augmentin (7, 7.6%, p=0.023) and tranexamic acid (5, 5.4%, p=0.031) (Table 3). Drug-drug interactions were observed in 44(47.8%) participants which were significantly associated with the severity of AKI (p=0.037). The most common interactions were observed between enoxaparin and ceftriaxone (8, 8.6%), aspirin and enalapril (7, 7.6%), aspirin and carvedilol (6, 6.4%) and furosemide and enalapril (4, 4.3%). However, none of these specific interactions were associated with the severity of AKI. Nevertheless, the number of medications with the potential for nephrotoxicity was significantly associated with the presence of interactions (0.003).
| Medications | Frequency (n) | Per (%) | p-value |
|---|---|---|---|
| Enoxaparin | 20 | 21.7 | 0.006* |
| Metoclopramide | 14 | 15.2 | 0.016* |
| Augmentin | 7 | 7.6 | 0.023* |
| Ceftazidime | 6 | 6.5 | 0.152 |
| Aspirin | 6 | 6.5 | 0.629 |
| Morphine | 5 | 5.4 | 0.83 |
| Tranexamic acid | 5 | 5.4 | 0.031* |
| Enalapril | 4 | 4.3 | 0.908 |
| Tramadol | 3 | 3.3 | 0.187 |
| Gentamicin | 3 | 3.3 | 0.214 |
| Clarithromycin | 3 | 3.3 | 0.99 |
| Spironolactone | 3 | 3.3 | 0.553 |
| Fluconazole | 3 | 3.3 | 0.8 |
| Ceftriaxone | 2 | 2.2 | 0.414 |
| Amphotericin B | 2 | 2.2 | 0.925 |
Note: * denotes statistically significant values.
Table 3: The association between “dosage too high” and AKI severity (n=92).
Predictors of AKI severity
Logistic regression analysis model was used to identify the predictors of severity of AKI. The AKI severity was transformed into a binary data by collapsing the moderate and severe severity one which was compared against mild AKI. Those with history of drinking alcohol were 4.3 (95% CI (1.24-14.86), p=0.021) times more likely to have moderate to severe AKI than those with mild AKI, having controlled for BMI, dosage problems and obstructive uropathy (Table 4). Furthermore, participants on prescriptions with dosage problems had 10.2(95% CI (2.63-39.16), p=0.001) times the odds of developing more moderate to severe AKI compared to those who did not after controlling for BMI, alcohol use and obstructive uropathy. Obstructive uropathy was the only condition that was included in the model which indicated 23.6 (95% CI (1.92-350.72), p=0.014) times likely to suffer from moderate to severe AKI compared to those who do not after controlling for BMI, alcohol use and dosage problems.
| Variables | Bivariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| COR (95% CI) | p-value | AOR (95% CI) | p-value | |
| BMI | 0.36(0.14-0.94) | 0.037* | 0.32(0.08-1.17) | 0.084 |
| Alcohol use | 2.76(1.14-6.60) | 0.025* | 4.29(1.24-14.86) | 0.021* |
| Dosage too high | 5.1(2.04-13.26) | 0.001* | 10.15(2.63-39.16) | 0.001* |
| Obstructive uropathy | 23.58(2.98-186.68) | 0.003* | 25.92(1.92-350.72) | 0.014* |
Abbreviations: COR: Crude Odds Ratio; AOR: Adjusted Odds Ratio; CI: Confidence Interval; BMI: Body Mass Index, *: p<0.05.
Table 4: Predictors of AKI severity (n=92).
Most of the participants with AKI were aged between 35 to 60 years with an average of 51 (± 15.96) years. Similar findings were observed where the middle aged population was most affected [13]. In developed countries there is of the disease increased risk above 65 years of age [14]. Smoking was found to be associated with more severe AKI, which is consistent with a study done in Finland [15]. Furthermore, smoking aggravates AKI severity in the presence of other comorbidities especially infectious diseases. Participants who were taking alcohol were at a higher risk of developing severe AKI compared to those who did not by 4.3 times. Similar findings were observed in patients with alcoholic liver hepatitis in Spain, which negatively impacted the patients’ short-term survival due to acute kidney injury [16]. Even though alcohol use disorders causing AKI has not been fully been understood, mechanisms that involves oxygen radicals formation from CYP 2E1 that causes oxidative stress [17].
Acute Decompensated Heart Failure (ADHF) was the most common comorbidity followed by obstructive uropathy, hypertension, HIV and sepsis. However, a different pattern was observed in Sudan that showed sepsis, volume depletion, obstructive uropathy, heart failure, acute glomerulonephritis, and severe malaria were the common causes of AKI [18]. ADHF which was the leading cause of AKI among the comorbidities has the potential of causing low blood pressure, thus leading to AKI [19]. Notably, obstructive uropathy was 25.9 (p=0.014) times more likely to cause severe AKI [20].
The medication related problems associated with the severity of AKI was polypharmacy which has been observed to be linearly associated with medication related problems [21]. Participants who had dosage issues were 10.2 times likely to have a more severe AKI compared to those who did not. This suggests the importance of dosage adjustment in patients who are prone to developing AKI and those who already have AKI.
Paracetamol was the preferred analgesic which concurs with the National Kidney Foundation recommendations [22]. The use of opioids which included tramadol and morphine was used in pain management but was not associated with the severity of AKI. In fact, opioid use has been associated with the accumulation of the parent drug and its metabolites in patients with acute kidney injury since they are primarily excreted by the kidneys [23]. However, fentanyl does not significantly accumulate in the body hence recommended in patients with renal insufficiency [24].
Anticoagulation is crucial in preventing deep venous thrombosis in hospitalized patients, particularly in patients with AKI [25]. About half of the participants were on enoxaparin which was similar to a previous study [26]. In some cases (20, 21.7%), the dose was not adjusted for the renal clearance below 30 ml/min. Since enoxaparin is excreted via the urine the patients may be therefore exposed to toxic levels leading to bleeding [27,28]. That being the case, the usefulness of enoxaparin in patients with AKI should be explored further since the effectiveness of the dosage used in the prevention of DVT is still in question [27,28].
Empiric antibiotics use in patients with sepsis is always warranted in advanced resuscitation therapy under the concept of “hit hard and hit fast” which is the cornerstone of management to improving survival [29,30]. Augmentin was the only drug associated with the severity of AKI (p=0.023). Owing to Augmentin being a beta- lactam which is hydrophilic and the elimination depends on the renal clearance as the unchanged product [31]. In as much as the standard dose is used in the initial prescriptions and the dose hardly adjusted based on the creatinine clearance consequently exposing the patients to higher doses which may cause acute interstitial nephritis [32].
The use of antiemetics is paramount in managing nausea and vomiting in uremic patients. The use of metoclopramide requires dosage adjustment based on creatinine clearance since its elimination depends on renal function. In this study, some of the participants were on a higher dosage of metoclopramide (14, 15.2%) and was associated with the severity of AKI (p=0.016). Extrapyramidal side effects which are common with metoclopramide occur in 0.2% of the patients which was not manifested in this study since the observation was done within a short time after administration [33,34]. Additionally, numbness, tingling sensation and dizziness occurred in participants who were on inappropriately prescribed metoclopramide which are commonly observed side effects [35].
Tranexamic acid is an antifibrinolytic used in the management of bleeding episodes that had a higher dosage in 5 (5.4%) participants and was associated with the severity of AKI (p=0.031). These participants also experienced headache, nausea, malaise, and abdominal pain. These findings were consistent with a review of frequently reported adverse events which include fatigue, musculoskeletal pain, arthralgia and myalgia [36].
Antihypertensive medication may reduce blood pressure to the extent of reducing renal perfusion thus precipitating AKI. Association with Low blood pressure and severity of AKI was observed in patients on carvedilol (p=0.006) and enalapril (p=0.016) but not with the amlodipine (0.219) and nifedipine (0.343). Moreover, these findings are consistent with a new-user cohort study that showed an associated 12% higher relative risk of AKI on ACEi/ARB antihypertensive medication and especially those with other conditions that predispose the patients to have low blood pressure [37,38]. Additionally, beta-blockers are known to reduce renal function, particularly the non-selective agents that reduce renal plasma flow and effective glomerular filtration [39]. A recent review on the use of RAAS inhibitors showed no benefit in stopping the medication, in patients with a renal decline, but also suggested the need for renal dose adjustment in case worsening kidney function up to 30% [40]. Among the diuretics used, an association was observed in the use of spironolactone (p=0.005) and the severity of AKI. Additionally, inappropriately prescribed spironolactone was associated with a high heart rate (p=0.032) which is an indicator of hypotension. Diuretics are neither effective in the prevention of AKI nor shorten the duration of AKI when used in volume management [41].
The presence of drug-drug interactions was associated with the number of drugs prescribed (p<0.001) and severity of AKI (p=0.042). Polypharmacy, especially in the elderly population, lead to a prolonged hospital stay and increased mortality [42]. Additionally, the aging populations are vulnerable due to multiple organ dysfunction, hence the need for more medication in their prescriptions. The most commonly involved medications in drug-drug interactions from this study were enoxaparin, enalapril, furosemide, clarithromycin, aspirin and carvedilol consistent with the study done by Juarez-Cedillo, et al. [43]. Enoxaparin and ceftriaxone interactions, ceftriaxone increases the anticoagulant effect of enoxaparin by decreasing prothrombin activity and therefore close monitoring of bleeding tendencies or antithrombotic alternatives be considered. Interactions were seen between furosemide and enalapril and were not significantly associated with AKI as observed in a different study though close observation is advised [44].
The triple whammy phenomenon that is known to cause renal failure was observed in one patient who was on enalapril, furosemide, and aspirin. This phenomenon produces significant nephrotoxicity that may go unrecognized particularly among the aged [45,46]. As an antiplatelet, aspirin is necessary for cardiovascular protection. The inappropriate use of aspirin observed was not associated with the severity of AKI since the dosage was below the amount that may cause renal insufficiency [47]. Concurrent use aspirin and enalapril were not associated with the severity of AKI contrary to some previous studies but there may be increased mortality [48,49]. However, these conflicting findings occur at the center of the theorized effect between the two drugs. Aspirin has been shown to attenuate the beneficial effects of ACEi by reducing prostaglandin synthesis hence altering systemic vasodilation and renal perfusion [50]. Additionally, the combination of beta-blockers and aspirin requires close monitoring since aspirin blunts the effects of carvedilol through pharmacological antagonism, affecting the remodeling process, thus altering the left ventricular ejection fraction benefits but the significance of this effect is still unknown which is consistent with this study since there was no association with AKI severity [51].
The patients who were on clarithromycin-based regimen and dosage not appropriately adjusted for had low blood pressure while the ones on azithromycin had normal blood pressure. Co- prescription of clarithromycin and calcium channel blockers has been shown to have a higher risk of hospitalization, hypotension and greater all-cause mortality compared to those on azithromycin [44,52]. Additionally, macrolides are known to inhibit cytochrome P450 3A4 enzymes that take part in the metabolism of calcium channel blockers. Clarithromycin is a strong enzyme inhibitor while Azithromycin is a weak inhibitor of the enzyme hence the observed effects [53].
Since the prevalence of MRP in AKI was high in KNH, the following considerations should be factored in by the clinicians preparing prescriptions. First, the patient’s comorbidities that predispose the patient to getting AKI such as pelvic malignancies should be taken into consideration. Conditions that have tendencies to cause hypotension particularly acute decompensated heart failure and sepsis should be factored into when dosing the medications [54]. Secondly, the clinicians should look out for the drugs that are renally cleared to reduce the risk of high dose exposure to the patient through dose adjustment. This includes painkillers (opioids), anticoagulants (enoxaparin), antibiotics (penicillins) and antiemetics (metoclopramide). Drug interactions should also be watched out for particularly in patients on multiple medications for hypertension using angiotensin converting enzymes inhibitors (enalapril), diuretics (furosemide), painkiller medications (NSAIDS: Nonsteroidal Anti-Inflammatory Drugs) and antibiotics (clarithromycin). These should also be looked into in terms of enzyme inducers and enzyme inhibitors. These considerations based on the study findings would be vital in improving patients’ outcomes.
The prevalence of medication related problems was 67% with the most common types of medication related problems in patients with AKI being over-dosage due to high dose and short frequency administration as well as drug interactions. The presence of comorbidities that predispose patients to low blood pressure in the presence of medication related problems was implicated in severe AKI. The main determinants of AKI identified were obstructive uropathy, high medication dosage and alcohol intake. Among the medications associated due to inappropriate prescriptions were augmentin, metoclopramide, enoxaparin, and tranexamic acid. They were mostly implicated in the severity of AKI and hence closer monitoring of the respective patients. It is recommended that pharmacists be part of the patient care team to help in identification and resolution of the MRPs. Since the management of AKI is still a challenge, it is further recommended that a prospective study be done to investigate the morbidity and mortality outcomes, hospital stay as well as a cost impact on patients with AKI with the associated medication related problems.
To all the faculty members of the school of pharmacy University of Nairobi and patients at Kenyatta National Hospital medical wards for the immeasurable support during the study.
Authors declare no conflict of interest
This work was supported by the Kenyatta National Hospital Research and Programs under Grant number KNH/R&P/23H/97/11.
Obala Neto conceptualized the idea, wrote the concept, collected and analyzed the data and drafted the manuscript. Peter Karimi assisted with proposal development, data analysis, and interpretation as well as writing the manuscript. Francis and Peter Karimi reviewed the proposal, data analysis and revised the manuscript. All authors approved the final manuscript for publication.
Citation: Neto OL, Ndemo FA, Karimi PN (2021) Prevalence and Determinants of Medication Related Problems in Acute Kidney Injury Patients at Tertiary Teaching and Referral Hospital in Kenya. J Pharma Care Health Sys. 8:235.
Received: 11-Jun-2021 Accepted: 25-Aug-2021 Published: 02-Jul-2021 , DOI: 10.35248/2376-0419.21.8.235
Copyright: © 2021 Neto OL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.