
Cell & Developmental Biology
Open Access
ISSN: 2168-9296

ISSN: 2168-9296
Research Article - (2021)Volume 10, Issue 4
This study was carried out to determine the prevalence and antibiotics resistance of Staphylococcus aureus among HIV/AIDS patients on highly active antiretroviral therapy in Ekiti State, Nigeria. A total of 200 blood samples were collected from Federal teaching Hospital, Ido-Ekiti and University Teaching Hospital Ado-Ekiti. The blood samples were examined for bacteria using cultural and biochemical characteristics. Antibiogram was carried out by disc diffusion method. CD4+ T-cell count was done using flow cytometry method. The Socio-demographic data of the patients were obtained through questionnaire. A total of 26 Staphylococcus aureus were isolated from HIV/AIDS patients with overall prevalence rate of 13.0% which is statistically significant (p value 0.02). Results showed that female subjects 15(7.5%) with HIV/AIDS were more susceptible to S. aureus associated bacteraemia than males 11(5.5%). Age group 41-50 years were the most infected with S. aureus with median age of 35 years (p value 0.607, X2= 0.26, df=1) which is not statistically significant. The CD4+ T-cell of the HIV/AIDS patients with S. aureus were within the range of 20 to 400 cells/µl. However, low CD4-T cell and multiple previous hospital admission were the identified risk factors with 100% and 88.5% occurrence rate respectively. The bacterial isolates were tested for resistance to eight antibiotics commonly prescribed in hospitals. The resistance to the antibiotics ranged between 42.3% to 80.8% with ciprofloxacin having less resistance. This study strongly suggests that the isolation of the S. aureus from HIV/AIDS patients might be because it takes advantage of the weaken immune system provided by deficiency in β-cell and dysfunctional macrophage in HIV/AIDS patients
HIV/AIDS; Staphylococcus aureus; HAART; CD4+ T-cell.
Human Immunodeficiency Virus (HIV) is characterized by a serious disorder of the immune system in which the protective defences against infection cannot function leaving the individual vulnerable to severe infections and conditions [1]. The resulted opportunistic infections cause unfavourable outcome and increase the morbidity and mortality in both children and adults. There is a high prevalence of HIV infection among patients admitted to hospitals as well as a high prevalence of AIDS patients as a result of opportunistic infections related to their HIV status or advanced AIDS [2]. A major risk factor for bacterial colonization is immunosuppression subsequently making HIV infected individuals ideal candidates for bacterial infections [3]. Colonization contributes significantly to the development of nosocomial infections in HIV positive patients [4]. Colonization is the first step of microbial infection. It is the establishment of the pathogen at the suitable portal of entry for example, host tissues that are in contact with the external environment. Sites of entry include the conjunctiva, the digestive tract, the respiratory tract and the urogenital tract [5]. Organisms such as Staphylococcus aureus have been found to have high rates of nasal colonization in HIV infected patients and can disseminate to blood where it causes bactereamia [6]. Bacteraemia are among the most severe of hospital-acquired infections and have been shown to cause significant mortality and prolonged hospital-stays in patients with HIV [7]. Since the beginning of AIDS epidemic, the bacteraemia has become a frequent secondary infection. This is because of the depilated immune system. The advent of HAART has reduced these secondary infections; but despite this, the HIV infected patients are still face with varying secondary infection including Staphylococcus aureus bactereamia.
Staphylococcus aureus is the most commonly isolated human bacterial pathogen [8] and is the leading cause of gram positive bacterial infections [9]. It has clinical range from minor skin infections to severe life threatening infections including bactereamia [10]. Staphylococcus aureus has emerged as a significant opportunistic pathogen among HIV and AIDS patients in both nosocomial and community settings and recent studies have shown greater frequency and morbidity of this organism among HIV positive individuals [11]. Symptoms of abdominal illness such as nausea, vomiting and loss of appetite were also associated with bloodstream infections caused by this pathogen [12]. Globally, Staphylococcus aureus is the second most common pathogen that is responsible for causing Blood Stream Infections (BSI) [13] and in European countries, it is the leading cause of nosocomial bloodstream infections [14]. S. aureus is also the most common pathogen isolated from all Bloodstream infections (BSI) [15]. Staphylococcus aureus has a preference for the anterior nares, with this colonization’s prevalence varying, depending on the population studied [16]. It has a mean of 37.2% in the general population, and a rate of up to 35.5% in the nasal sites of patients with Human Immunodeficiency Virus (HIV) [17]. Nevertheless, antibiotic therapy is fundamental to illness control in this group of patients because of their impaired immunity. Unfortunately, the incidence of bacterial resistance to antibiotics is high and therefore posing a major challenge to the management of these patients.
In this study, the prevalence and antibiotic resistance of S. aureus bloodstream isolates were determined in other to provide an updated data and influence the treatment decision by the health workers.
Study area
The study areas for this work were Federal Teaching Hospital, Ido Ekiti and Ekiti State University Teaching Hospital, Ado Ekiti located in Ekiti North senatorial district and Ekiti Central Senatorial District of Ekiti State respectively.
Study subjects and sample size
A total of 200 HIV/AIDS patients were collected between September, 2015 and February, 2016 were selected and investigated for Staphylococcus aureus blood stream infection. Patients who are on HAART and with clinical history of severe illness and fever were selected for this study. Fever has been defined as individual whose axillary temperature is >_ 37.5o C. Two hundred blood were collected from HIV negative patients with sporadic cases seeking medical attention in the above named hospital and this served as control population. Ethical consideration, questionnaire and informed consent The ethical clearance for this research was given by Federal Teaching Hospital ethical committee after due processes. Before the collection of the sample, information regarding the study was explained to the subjects. Oral and written consent for participation in the study were obtained. Questionnaire to obtain the demographic characteristics and other relevant information to the study as well as an informed consent were administered to the participant.
Determination of the CD4+
CD4+ values of the patients used for this study were obtained from the HIV Laboratory of the Federal Teaching Hospital through the help of Medical Laboratory Scientist. The method used for this estimation is DP Flow Cytometry. The kit included monoclonal antibodies of CD45PerCP. About 50 μl of whole blood is pipetted into tubes containing 10 μl of monoclonal antibodies, vortexed and incubated for 15 minutes at room temperature; 450 μl of FACS Lysing solution is added and incubated for 15 minutes. Four colour analysis was performed to obtain the percentage of lymphocytes subsets. The absolute CD4 + T-cell count was computed by multiplying CD4 percentage by ALC/100 and expressed in cells/μl. The ALCs were obtained on haematology analyser sysmex XE-2100.
Collection, handling transport and processing of specimens
About 5 ml of venous blood was drawn aseptically by cleaning the skin using 70% alcohol from each patient and placed into Brain Heart Infusion (BHI). A minimum blood to broth ratio of 1 in 10 was maintained [18]. All blood specimens were collected by the laboratory technician. The blood culture broth was incubated at 37oC for 7 days and was subcultured onto Mannitol salt agar. This medium is recommended for the isolation of S. aureus from clinical samples [19,20]. Blood culture with no bacterial growth after sub cultured were reported as negative.
Identification of staphylococcus aureus
The growth of Staphylococcus aureus was detected by their characteristics appearance on Mannitol salt agar (Golden yellow). The colonies was Gram Stained and confirmed by biochemical reactions (Catalase and coagulase ). The isolates were be kept frozen at -70oC until when ready for use for antimicrobial susceptibility and phenotypic characterizations (serotyping) on nutrient agar slant.
Antimicrobial susceptibility testing
Disk diffusion testing
Antibiogram was performed for all Staphylococcus aureus isolates using the disk diffusion method and the results were interpreted using the criteria of the Clinical Laboratory Standard interpretation (CLSI). The drugs for disk diffusion testing were obtained from reputable company. Their codes and concentration (in μg) were as follow: Aminoglycosides: Gentamycin (GM) (10). Cephems: Ceftriaxone (CRO) (30), Ceftazidime (CAZ) (30), Fluroquinolones: Ciprofloxacin (CPX) (10), Ofloxacin (OFL) (5), Folate pathway inhibitor: Cotrimoxazole (COT) (1.25+23.75). Penicillin: Ampicillin (AMP) (10).
It shows the overall prevalence of Staphylococcus aureus among HIV/AIDS patients on HAART. It revealed that out 200 HIV/ AIDS patients, 26 (13.0%) had Staphylococccus aureus in their blood while 174 (87.0%) did not have Staphylococcus aureus in blood culture with p value 0.02 which is statistically significant.
Prevalence of Staphylococcus aureus among HIV/AIDS patients in relation to study location is shown in Table 2. There are two locations used for this study. Out of 100 HIV/AIDS patients from Ido, 14 (14.0%) had Staphylococcus aureus in their blood while out of 100 HIV/AIDS patients from Ado, 12 (12.0%) had Staphylococcus aureus in their blood. This is not statistically significant p value 0.674 ( X2= 0.18, df= 1).
It shows the prevalence of Staphylococcus aureus among HIV/ AIDS patients in relation to Demographic data. It revealed that age group 21-30, 31-40, 41-50, and 51-60 years had 2(1.0%), 8(4.0%), 12(6.0%) and 4(2.0%) prevalence rate respectively.
The prevalence of S. aureus in relation to the sex revealed that female had the highest prevalence of S. aureus with prevalence rate of 15(7.5%) compare to their male counterpart with prevalence rate of 11(5.5%). This is not statistically significant (P value 0.607).
Prevalence in relation to the marital status showed that married HIV/AIDS patients had the highest prevalence of 14(7.0%), followed by Engaged with prevalence rate of 7(3.5%), while Single HIV/AIDS patients had prevalence rate of 5(2.0%).
The prevalence in relation to occupation showed that Civil servant, Farmer and Business had the prevalence rate of 11(5.5%), 5(2.5%) and 10(5.0%) respectively.
The prevalence in relations educational status showed that tertiary education had the highest number of prevalence rate of 12(6.0%), while HIV/AIDS patients with primary and secondary education had the prevalence rate of 6(3.0%) and 8(4.0%) respectively.
It showed the risk factors of HIV/AIDS patients with Staphylococcus aureus. It showed that all the HIV/AIDS patients with Staphylococcus aureus had low CD4 +T cells of ≤400 cell/μl, while 88.5% of the patient had been admitted in the hospital previously, 26.9% identified with smoking while 23.1% had previous history of surgical operation.
It showed the CD4+ T cells count of HIV/AIDS patients with Staphylococcus aureus in the blood. It showed that 13(6.5%) of the patients had CD4 T cells of 201-300 cell/μl while 8(4.0%) of the HIV/AIDS patients with S. aureus had CD4+T cells of 101-200 cells/μl while 4(2.0%) had the CD4+T cells of 20-100 cells/μl while 1(0.5%) had CD4+T cell of 301-400 cells/μl.
| CD4+cells (µ/ml)% | No Examined | No positive |
|---|---|---|
| 20-100 | 10 | 4(2.0) |
| 101-200 | 48 | 8(4.0) |
| 201-300 | 62 | 13(6.5) |
| 301-400 | 50 | 1(0.5) |
| 401-500 | 18 | 0(0.0) |
| 501-600 | 5 | 0(0.0) |
| 601-700 | 4 | 0(0.0) |
| 701-800 | 3 | 0(0.0) |
| Total | 200 | 26(13.0) |
Table 4: The CD4+ T cells count of HIV/AIDS patient with Staphylococcus aureus in the blood.
It shows the antibiotics resistance pattern of Staphylococcus aureus from HIV/AIDS patients. It showed that ciprofloxacin had the least resistance rate of 42.3%, followed by ofloxaxin with 50.0% resistance rate while Ceftazidime, Cefuroxime, Gentamicin, Cefixime, Augmentin and Nitrofuratoin had 73.1%, 65.4%, 80.8%, 65.4%, 76.9% and 65.4% resistance rate respectively.
Acquired Immune Deficiency Syndrome (AIDS) is characterized by a serious disorder of the immune system in which the protective defenses against infection cannot function leaving the individual vulnerable to severe infections and conditions. This results in opportunistic infections causing an unfavourable outcome. Nevertheless, the introduction of HAART has greatly reduced opportunistic bacterial infection in HIV/AIDS patients. The lifesaving role of antiretroviral therapy has improved and prolonged the survival outcome but some dilemmas around chronic HIV infections persist. In this study, the prevalence of Staphylococcus aureus among HIV/AIDS patients on HAART in Ekiti State was 26(13.0%) (Table 1) and it is statistically significant (p value 0.02, X2=68.65, df= 2). Who reported that S. aureus bactereamia have accounted for approximately 10%- 41% of infection in HIV/AIDS patients with increase mortality rate up to 67%. Also reported that bloodstream infections are a major cause of illness in patients infected with HIV. A high percentage of bloodstream infections, ranging from 10% to 63% were observed in hospitalised HIV infected individuals presenting with fever in a number of studies conducted in Sub-Saharan Africa. S. aureus is responsible for many infections but it may also occur as a commensal. The infections can spread through contact with pus from an infected wound, skin-to-skin contact with an infected person by producing hyaluronidase that destroys tissues, and contact with objects such as towels, sheets, clothing, or athletic equipment used by an infected person. However, in HIV/AIDS patients, they may be more predisposed to bloodstream infections due to Staphylococcus aureus base on several conditions such as defective cell-mediated immunity, altered B-cell function with a consequent lack of serum opsonins against some encapsulated bacteria and qualitative and quantitative deficits of neutrophils leading to an increase in the susceptibility of the patient to bacterial and fungal infections. Staphylococcus aureus has emerged as a significant opportunistic pathogen among HIV and AIDS patients in both nosocomial and community settings and recent studies have shown greater frequency and morbidity of this organism among HIV positive individuals. Globally, Staphylococcus aureus is the second most common pathogen that is responsible for causing bloodstream infections and in European countries, it is the leading cause of nosocomial bloodstream infections.
| Frequency | Percentage (%) | p-value | x2 | df |
|---|---|---|---|---|
| Positive | 26 (13.0) | 68.65 | 0.02 | 2 |
| Negative | 174 (87.0) | |||
| Total | 200 (100.0) |
Table 1: Overall Prevalence of Staphylococcus aureus among HIV/AIDS patients on HAART
Prevalence of Staphylococcus aureus among HIV/AIDS patients in relation to study location is shown in Table 2. It showed that the prevalence of S. aureus bactereamia infection among HIV/ AIDS patients in Ido-Ekiti was 14.0% which is higher than the prevalence obtained in Ado (12.0%). However despite the variation in the prevalence rate in these study locations, it was not statistically significant (p value=0.674, X2=0.18, df=1), suggesting that S. aureus infection was not just common to specific location but rather a problem among HIV/AIDS patients.
| Location | Positive | Negative | Total % | p-value | x2 | df |
|---|---|---|---|---|---|---|
| IDO | 14 | 86 | 100 | |||
| % of total | -14 | -86 | -100 | 0.674 | 0.18 | 1 |
| Ado | 12 | 88 | 100 | |||
| % of total | -12 | -88 | -100 | |||
| Total | 26 | 174 | 200 |
Table 2: Prevalence of Staphylococcus aureus among HIV/AIDS patients in relation to study location.
Prevalence of Staphylococcus aureus among HIV/AIDS patients in relation to age is shown in Table 3. It revealed that age 41-50years had the highest prevalence 12(6.0%) of S. aureus bactereamia, followed by 31-40 years with prevalence rate of 8(4.0%), while age groups 51-60 years had prevalence of 4(2.0%). This is in agreement with previous study conducted by Senthilkumar who reported that age group 30-39 years had the highest occurrence of S. aureus associated bacteremia [21].
| AGE(years) | Positive no(%) | Negative no(%) | Total% | p-value | x2 |
|---|---|---|---|---|---|
| 44136 | 0(0.0) | 2(1.0) | 2(1.0) | ||
| 21-30 | 2(1.0) | ||||
| 31(15.5) 33(16.5) | |||||
| 31-40 | 8(4.0) | ||||
| 38(19.0) 46(23.0) | |||||
| 41-50 | 12(6.0) | 50(25.0) | 62(31.0) | 0.225 | 8.18 |
| 51-60 | 4(2.0) | 130(15.0) | 34(17.0) | ||
| 61-70 | 0(0.0) | 10(5.0) | 10(5.0) | ||
| 71-80 | 0(0.0) | 13(6.5) | 13(6.5) | ||
| Total | 26(13.0) | 174(87.0) | 200(100.0) | ||
| SEX | |||||
| Male | 11(5.5) | 83(41.5) | 94(47.0) | ||
| Female | 15(7.5) | 91(45.5) 106(53.0) | |||
| Total | 26(13.0) | 174(87.0) 200(100.0) | |||
| MARITAL STATUS | |||||
| Married | 14(7.0) | 76(38.0) | 90(45.0) | ||
| Single | 5(2.0) | 35(17.5) 40(20.0) | |||
| Engage | 7(3.5) | 63(31.5) 70(35.0) | |||
| Total | 26(130) | 174(870) | 200(100.0) | ||
| OCCUPATION | |||||
| Civil servant | 11(5.5) | 84(42.0) | 95(47.5) | ||
| Farmer | 5(2.5) | 30(15.0) | 35(17.5) | 0.851 | 0.32 |
| 2 | |||||
| Business | 10(5.0) | 60(30.0) | 70(35.0) | ||
| Total | 26(13.0) | 174(87.0) | 200(100.0) | ||
| EDUCATION | |||||
| Primary | 6(3.0) | 24(12.0) | 30(15.0) | ||
| Secondary | 8(4.0) | 90(45.0) | 98(49.0) | 0.124 | 4.18 |
| 2 | |||||
| Tertiary | 12(6.0) | 60(30.0) | 70(35.0) | ||
| Total | 26(13.0) | 174(87.0) | 200(100.0) |
Table 3: Prevalence of Staphylococcus aureus among HIV/AIDS patients in relation to Demographic data.
The prevalence in relation to sex showed that female HIV/AIDS patient had the highest prevalence of 15(7.5%) compare to their male counterpart with prevalence rate of 11(5.5%) which is statistically not significant (P value=0.607, X2=0.26, df= 1).
Also, the marital status of HIV/AIDS patients is statistically not significant (p value 0.581). Although, the married had the highest prevalence 14(7.0%) and this is in agreement with the study conducted by Senthilkumar.
Risk factors of HIV/AIDS patients with Staphylococcus aureus is shown in Figure 1. It showed that low CD4 + cell count of ≤400 cell/ul was a major predisposing factor with 100% occurrence rate. This is because impaired cellular immunity is hallmark of HIV infection, but HIV patients particularly those with advance infection, may also have adequate humoral immunity, and abnormal chemotaxis, phagocytosis and bactericidal activity, resulting in increased susceptibility to bacterial pathogen including S. aureus [22]. This is in agreement with study conducted by several authors who reported that there is association between low CD4 +T cell (200 cells/μl) and higher risk of both asymptomatic colonization and clinically significant community acquired MRSA. Also multiple previous hospital admission had 88.5% occurrence rate in this study. This is also supported by Chacko who reported that the colonization of individuals with HIV/AIDS by pathogenic microorganisms has been associated with higher risk of morbidity and mortality, principally when related to Staphylococcus aureus [23]. Researchers found a rate of 76.7% of colonization with this bacterium in this population, indicating prolonged hospitalization (over 10 days) as a risk factor for resistance to methicillin.
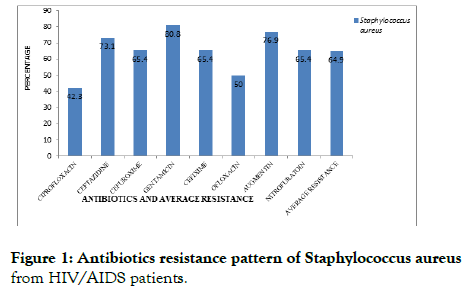
Figure 1. Antibiotics resistance pattern of Staphylococcus aureus from HIV/AIDS patients.
The antibiotics resistance pattern of Staphylococcus aureus from HIV/AIDS patients is shown in Figure 1. It showed that ciprofloxacin and ofloxacin had the least resistance rate. However, in this study, the resistances to all the tested antibiotics range from as low as 42.3% in ciprofloxacin to as high as 80.8% in gentamicin with an average resistance of 64.9%. This high resistance rate seen among the S. aureus from the HIV/AIDS patients might be because immunosuppression and the constant use of antimicrobials can viabilize colonization with multi resistant bacteria and the occurrence of infections. Prescott reported that strains of multiple drug resistant S. aureus have appeared and proven very difficult to treat. But nevertheless, ciprofloxacin and ofloxacin, a fluroquinolone class of antibiotics with less resistant pattern in this study might be very helpful in treatment of secondary bacterremia infection in HIV/AIDS patients.
Since the beginning of AIDS epidemic, the bacteraemia has become a frequent secondary infection. This is because of the depilated immune system. However, the advent of HAART has reduced these secondary infections; but despite this, the HIV infected patients are still face with varying secondary infection including bactereamia. This study further confirmed that Staphylococcus aureus is one of the causes of bactereamia in HIV/AIDS patients in Ekiti State and that bacteria was detected among HIV/AIDS patients whose CD4 + T cell counts falls within 20 –400 cells/ul. This suggested that the pathogen might have taking the advantage of dysfunctional macrophage and β- cell deficiency of HIV/AIDS patients. However, the multiple antibiotic resistances among bacterial isolates from various study groups are frightening because such organisms can become endemic within the environment and pose serious public health threats. The antibiotics resistant of S. aureus range from as low as 42.3% to 80.8%.
Staphylococcus aureus has emerged as a significant opportunistic pathogen among HIV and AIDS patients in both nosocomial and community settings. The clinical manifestation of HIV secondary infections in developing countries, including Nigeria, shows a high prevalence of infections of the blood and intestines. It is important to recall that the outcome of this study showed that NTS infections tend to occur in HIV/AIDS patients with low CD4+ lymphocyte counts and that the antibiotic resistance profile in this study will provide an updated data for clinicians, medical laboratory scientists and other health care workers in order to facilitate the use of appropriate and more effective treatment regimes. Nevertheless, in order to curb the problem of antibiotic resistance, indiscriminate use of antibiotics and over the counter sales of antibiotics should be discouraged and avoided. Therefore, ciprofloxacin with is highly recommended for the treatment of bacteraemia in HIV/AIDS patients. There is also need for continuous search for more effective antibiotics in different locations.
Citation: Okunnuga A, Ojo-bola O, Alo B, Okunnuga N (2021) Prevalence and Antibiotics Resistance of Staphylococcus Aureus Among Hiv/Aids Patients on Highly Active Antiretroviral Therapy in Ekiti State. Cell Dev Biol. 10: 235
Received: 02-Jul-2021 Accepted: 15-Jul-2021 Published: 22-Jul-2021 , DOI: 10.35248/2168-9296.21.10.235
Copyright: © 2021 Okunnuga A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.