
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Review Article - (2023)Volume 13, Issue 4
Drug interaction is a pharmacokinetic or pharmacodynamic consequence of medications on each distinctive, which can sequence, along with desiderated outcomes, in de-escalated effectiveness or escalated toxicity. “Drug-drug interaction” is delineated as the pharmacologic or clinical reaction to the administration of a drug conflation that is distinctive from the expected consequences of the dual medications when bestowed lone. Pharmacokinetic interactions happen when a medicine influences the absorption, distribution, metabolism, or excretion characteristics of disparate medicine PK DDIs happen as a sequence of a revamp in the vulnerability to a bestowed dose of lone medication when bestowed with distinctive. Medications that act as inducers or inhibitors of CYP450 enzymes in the enterocyte and hepatocyte perhaps revamp liability by revamping oral bioavailability. Pharmacodynamic interactions happen when dual medications that are taken coincidentally have either additive or revoking consequences on the body. The implicit for pharmacodynamic interactions should be thought-out for medications which contest with each distinctive at the pharmacological target and/or have analogous or combating pharmacodynamic (therapeutic or adverse) consequences.
Dug-drug interactions; Clinical management; Pharmacodynamic; Pharmacokinetic; CYP450 enzyme
ADRs: Adverse Drug Reactions; CYP450: Cytochrome P450; DDIs: Drug-Drug Interactions, DI: Drug Interaction; PH: Potenz Hydrogen; GERD: Gastroesophageal Reflux Disease; GIT: Gastrointestinal Tract; PD: Pharmacodynamic; PK: Pharmacokinetic; P-gp: P-glycoprotein
DI is described by a revamp in the deed of a medication, antecedent by coincidental or foregoing prescribed of distinctive medication(s) [1]. When medications possess a synergistic consequence, the therapeutic outcomes perhaps potentiated; when antagonistic, coterminous administrations perhaps downgrade their efficaciousness. Besides, drug interaction can interpose in the way medications are absorbed, metabolized and/or eliminated [2,3]. DDIs happens when alone therapeutic agent either make over the engrossment (PK interactions) or the consanguineous consequence of farther agent (PD interactions) [4]. “DDI” is delineated as the pharmacologic or clinical reaction to the administration of a drug conflation that is distinctive from the expected outcomes of the dual medications when bestowed lone. DDIs perhaps sequence in adverse drug reactions, downscale therapeutic merit, or long-suffering affliction [5,6]. A PKs or PD impress of medications on each distinctive, which can sequence, beyond desiderate outcomes, in demoted efficacious or accelerated toxicity. PK and PD techniques are influential implements to perceive and comprehend drug deed in the uninjured organism [7,8] (Figure 1).
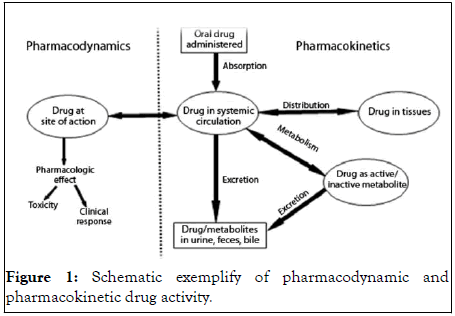
Figure 1: Schematic exemplify of pharmacodynamic and pharmacokinetic drug activity.
Pharmacological interactions
Pharmacological interactions are clustered as pharmacodynamic interactions and pharmacokinetic interactions [9]. Factually, poly therapy escalates the intricateness of therapeutic direction and thereby the pitfall of clinically applicable DIs, which can inaugurate the advancement of ADRs, and both dis-rate, or accelerate the clinical efficaciousness (Figure 2) [10-13].
Figure 2: Schematic exemplify of drug-drug interaction mechanisms.
Pharmacodynamic drug-interactions
PD is the inquest of the biochemical and physiological consequences of medications and their mechanisms of deed. PDs are the hitch for the outcome(s) that a medication has on the body [14]. Paramount medications interact with receptors to generate their characteristic consequences. Receptors are operational macromolecular constituents of the organism with which the medication interacts to deduce a cellular reaction, i.e., a revamp in cell blowout [15,16]. The linkage between a receptor and medication is frequently analogized with a lock and key. Cell receptor molecules enchain with naturally appearing substances (e.g., hormones, neurotransmitters) or medications [17,18]. Receptors perhaps reflected of as keyholes that provide access to the cell with the correctly fitting key. The “key” may be a naturally occurring substance in the body such as epinephrine (adrenaline), or a medication or each distinctive substance that is extrinsic to the body, connate as an herb (Figure 3) [19,20].
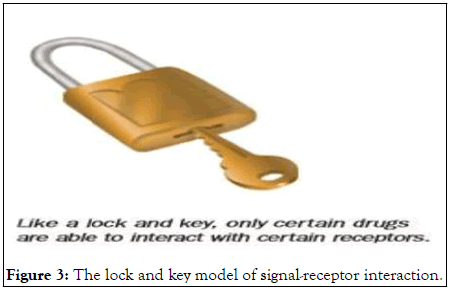
Figure 3: The lock and key model of signal-receptor interaction.
A medication that enchains with a receptor (i.e., applicable into the keyhole) and antecedent it to deed in the indistinguishable way as a naturally happening substance is called an agonist. Medications that attach with a receptor to preclude it from interacting with naturally happening substances hindering the receptor (i.e., jamming the lock) are called antagonists. PD interaction is perhaps antecedent by a voluminous diverseness’ of mechanisms. The implicit for PD interactions should be reasoned for medications which contest with each distinctive at the pharmacological target and/or have comparable or combating PD (therapeutic or adverse) effects. Additive, antagonistic, and synergistic DDI is the combined outcomes of medications perhaps sequence in additive, antagonistic, potentiation, or synergistic DDIs.
Additive DDIs happen when the consequence of dual medications sequences in a greater consequence than the outcomes of each agent given lone or (the sequence is what you anticipate when you append coincidentally the outcome of each medication taken independently) (1+1=2).
Detrimental additive DDIs: Conflation of alcohol and lorazepam cause accelerated (and occasionally hazardous) drowsiness or sedative effects, greater than the drowsiness antecedent by either alcohol or sleep medicine lone. The sleeping pill lorazepam is administered to promote drowsiness. Aspirin restrains platelet aggregation (hinders them from adhering coincidentally to conformation a clot) and heparin obviates blood from clotting; the conflation of an antiplatelet medication and an anticoagulant perhaps escalate the peril of bleeding.
Beneficial additive DDIs: High blood pressure is frequently treated with dual or poly anti-hypertensives to acquire surpass constrain athwart blood pressure. When an ACE inhibitor is appended to a Calcium Channel Blocker (CCB), the conflation of these medications frequently lesser blood pressure further effectively than accelerating the dose of lone medication.
Potentiation DDIs: Occur when one drug or food increases the effects of another drug, which does not generate any consequence when administered lone. Potentiation can be delineated using the mathematical expressions: 1+0=2.
Salicylates, sulphonamides, proteins warfarin, phenylbutazone, fibric acid derivatives can potentiate the anti-hyperglycaemic effect of sulphonylureas amidst by displacement from plasma binding protein. Carbidopa exhibits no anti-parkinson disease activity when administered alone. When added to levodopa, the anti-parkinson disease effects of levodopa are increased. Carbidopa is able to decrease the destruction of levodopa in the gastrointestinal tract so more of the levodopa can get to its site of action in the brain. Clavulanic acid exhibits’ no antibacterial activities when administered solely. When added to amoxacillin their combination form augmentin and enhance the antibacterial activity of amoxacillin rather than when administered solely. Probenecid has the capability to hinder the transport of organic acids of penicillins through epithelial cells such as renal proximal tubule cells or by de-escalating the kidneys capability to eliminate the penicillins from the body and enhancing penicillins plasma levels, then it heightened blood levels of the penicillin and a elongate continuance of antimicrobial deed.
Antagonistic DDIs: Happen when lone medication de-escalates or removes the consequence of distinctive or (conflating the medications premiers to a slighter outcome than anticipated) (1-1=0). Antagonistic DDIs are the cornerstone for reversal toxicity in poisoning. Antagonistic medication interactions are frequently unwanted.
Beneficial antagonistic DDIs: Acetaminophen toxicities perhaps treated with a medication named acetylcysteine, which precludes the toxic consequence on the liver by excluding toxic metabolites) of paracetamol and furnish cysteine for the glutathione generation and conceivably to create an adduct straightly with the toxic metabolite of paracetamol and N-acetylp- benzoquinoneimine and to thereupon preclude its covalent bonding to the hepatic proteins. The unfractionated heparin antagonist protamine sulfate is used for unfractionated heparin overdoses owing to its extreme basic protein that ensuing enchains with extremely acidic heparin to generate a stable and quiescent chelation (salt).
Detrimental antagonistic DDIs: Quinine are antagonize chloroquine antiparasitic (antimalarial) activity by inhibit(s) endocytosis of erythrocyte cytosol by the parasite, leading to reduced concentrations of free haem, to which chloroquine binds, in the digestive vacuole and quinine can inhibit uptake of chloroquine, giving a presumptive basis for the antagonistic effect. Penicillin has an antagonistic consequence with tetracycline and chronicle can premier to a 2.6 times higher pitfall for mortality when treating pneumococcal meningitis analogized to using penicillin lone whereas bacteriostatic (tetracyclines) antagonize bactericidal (penicillin) because bacteriostatic antibiotics (tetracyclines) inhibit cell division and protein synthesis, which are required for the bactericidal effect of most bactericidal agents (penicillin). Amphotericin B and azoles have antagonistic actions because static (azoles) antagonize-cidal drugs (amphotericin-B), static antifungal (azoles) inhibit the ergosterol synthesis, which are required for the fungicidal effect of antifungal agents (amphotericin-B).
Synergistic DDIs: Happen when the conflated consequence of dual medications transcends the summation of the outcomes of each medication bestowed lone or (conflating the medications guides to a higher consequence than anticipated) (1+1=3). Antibiotics are frequently given coincidentally for a synergistic outcome’.
Beneficial synergistic DDIs: Aminoglycosides such alike gentamicin and penicillins such alike ampicillin are frequently bestowed for sober-sided infections in hospitalized longsufferings owing to penicillin mediated well damage, facilitate entry (intracellular uptake) of the aminoglycosides in to the cell, which causes the subsequent bactericidal effect against the Enterococci. Diloxanide furoate and metronidazole have synergistic consequences and their conflation hastily generates grand parasitological and clinical curative grades by killing the bacteria and other microorganisms that cause infections by damaging the DNA. Atavaquone is frequently used in conflation with the antifolate medication proguanil, because they deed coincidently to antecedent a synergistic antimalarial consequence owing to they are inhibitor of dihydropteroate synthase plus an inhibitor of dihydrofolate reductase or synergistically and sequentially inhibit parasitic synthesis of tetrahydrofolic acid and finally destroy all susceptible organisms (parasitic) that cause malaria.
Detrimental synergistic DDIs, the conflation of nitrates (e.g., nitroglycerin, isosorbide) and erectile dysfunction drugs such as sildenafil (Viagra), which perhaps antecedent a implicitly lifethreatening drop in blood pressure when taken coincidentally. The conflation of potassium sparing diuretics (eplerenone) and angiotensin converting enzyme inhibitors (captopril) perhaps cause dangerous escalate the amount of potassium in the blood (hyperkalemia), finally cause kidney disease, diabetes, heart failure.
Pharmacokinetic drug-interactions
PD is delineated as what the body does to a medication, or furthers conventionally, the movement of medications amidst the body enclosing the procedure of Absorption, Distribution, Metabolism, and Excretion (ADME). PK DDIs can happen at the scale of absorption, distribution, or clearance of the disposed agent. PK DDIs happen as a sequence of a revamp in the vulnerability to a bestowed dose of lone medication when bestowed with distinctive. Medications that act as inducers or inhibitors of CYP450 enzymes in the enterocyte and hepatocyte perhaps revamp liability by revamping oral bioavailability (Figure 4).
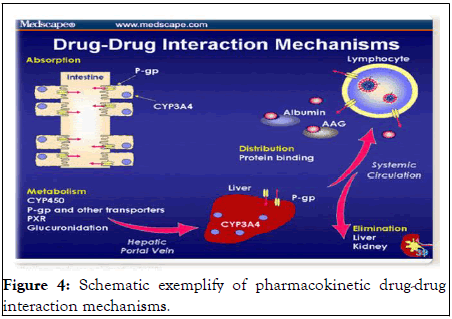
Figure 4: Schematic exemplify of pharmacokinetic drug-drug interaction mechanisms.
Drug absorption
Medications that accelerate the pH of the stomach (i.e., make it lesser acidic) can revamp the absorption of medications that are well absorbed in an acidic ambient. For instance, absorption of the antimycolytic medication, ketoconazole, is downgraded when taken with a PPI (e.g. omeprazole), which enhances the pH of the stomach. PPIs perhaps de-escalate the absorption of distinctive medications by attaching the medication or by revamping a medication's pH based solubility (e.g. doxycyclines, norfloxacillin, ketoconazole, ferrous sulfate). Enteric coated aspirin has a coating that is contemplated to dissolve at an opulent pH (further alkaline) so that it will not dissolve in the stomach and antecedent challenges for long sufferings with ulcer malady. Bestowing enteric aspirin with a medication that accelerates the pH of the stomach, such a like famotidine, can antecedent the enteric coating to dissolve in the stomach rather than the intestine. The supplementary label, “take on an empty stomach,” conventional signify the medicine is preferably absorbed in a further acidic circumstances. Distinctive mechanism of DDI encloses de-escalated absorption amid attaching and precipitation (conformation of an insoluble chelation) mechanisms. For instance, the conflation of norfloxacin and ferrous sulfate perhaps sequences in lesser norfloxacin absorption. Bile acid sequestrants such a like cholestyramine and colesevelam attach bile acids and preclude their absorption in the digestive tract but they can also enchain distinctive medications, particularly acidic medications (e.g., warfarin, acetyl salicylic acid, sulfonamides, phenytoin, and furosemide). Thereupon, the interim between the administration of cholestyramine or colesevelam and distinctive medications perhaps whereas attainable (preferably 4 h). Drugs that decrease gut motility such as metoclopramide, perhaps enhance gastric emptying, thus de-escalating the absorption of digoxin and theophylline as long as it can escalate the absorption of alcohol, acetylsalicylic acid, paracetamol, doxycycline and levodopa.
Distribution
Subsequently a medication is absorbed or injected into the bloodstream; it is distributed to multifarious body tissues. DDIs can happen at the distribution aspect of PKs. Distribution distinguishes amid medications and based on agents such a like lipid solubility and blood circulate to the explicit tissue. Organs that concede greater blood circulate such a like the liver, heart, and kidney concede higher quantum’s of medication further promptly than organs with lesser blood circulation such a like muscle, fat, and peripheral tissues. Singular agent that influences medication distribution is the confines of attaching with plasma and tissue proteins. Medications enchain at diversifying grades to plasma proteins such a like albumin. Protein-bound medications are not accessible to exert pharmacological consequences. Solely the amount of the medication that is not protein bound is accessible for diffusion to tissue sites and pharmacological outcomes. Dual medications that are largely plasma protein bound perhaps compete for the same binding sites causing high concentrations of unbound (free) pharmacologically active drug. Two drugs that are highly plasma protein bound may contest for the identical attaching places antecedent large engrossments of unattached (autonomous) pharmacologically active medication. For instance, the anti-seizure medication phenytoin perhaps further pharmacologically active and necessitates dosage acclimatization when bestowed with valproic acid, distinctive anti-seizure medication. In hitches of clinical importance, protein-attaching DDIs are the slight significant of the four PK elements (Figure 5).
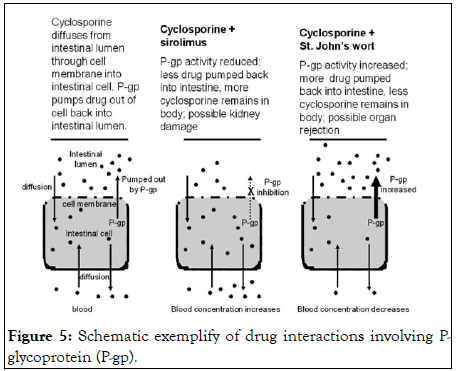
Figure 5: Schematic exemplify of drug interactions involving Pglycoprotein (P-gp).
Drug metabolism
Numerous medications are eliminated by metabolism. The microsomal reactions that have been thought-out the further enclose CYP450 family of enzymes, of which a few are accountable for the preponderance of metabolic reactions enclosing medications. These enclose the isoforms CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A4. DIs depend on revamped metabolism are chiefly fingerprinted to consequences on CYP450 isozymes. The consummate ordinary isozyme is CYP3A4, followed by 2C19, 2C9, 1A2, 2E6, and 2D6. Medications interacting with CYP450 isozymes can be grouped as substrates, inducers, or inhibitors. Different medications are substrates of transport-protein-complexes, such a like P-gp, which are concreted in hepatocytes and enterocytes, as well as in the epithelial cells of the renal tubules, the blood brain barrier, and the placenta.
Enzyme inhibition appertains to de-escalate in metabolic enzyme activity owing to the availability of an inhibitor. Medication metabolism by CYP450 can be hindered by any of the three mechanisms: Competitive inhibition, noncompetitive inhibition and uncompetitive inhibition. Inhibition of enzyme activity perhaps sequence in greater accumulations and/or extended half-life of the substrate medication, which escalates the implicitly for toxic side effects. Enzyme induction is consociated with accelerate in enzyme activity. For medications that are substrates of the isoenzyme induced, the consequence is to lesser the accumulation of these substrates. The clinical outcome of the availability of a generating agent and the resultant decrease in concentration of the substrate may mean a loss of efficacy and extended half-lives of poor bioavailable medications with accordingly less often dosing and a lesser total necessitated dose (i.e., inhibition of P-gp, CYP450 and organic anion transporters. This will sequence in charge savings and enhanced longsuffering compliance.
The asthma medication, theophylline, is a substrate of CYP1A2. If a long-suffering with therapeutic blood levels of theophylline commences taking cimetidine, used for GERD, theophylline levels perhaps accelerate to toxic accumulations as long as cimetidine inhibits the outcome of CYP1A2 and theophylline is metabolized further laggardly. Erythromycin and clarithromycin inhibit the hepatic metabolism and causes accumulation of theophylline, warfarin and terfenadine by de-escalating production of hepatic drug metabolizing enzymes required for the metabolism, it increases the accumulation of drug concentration in the plasma (blood) serum level and finally cause drug toxicity. Fluconazole administration perhaps escalates the consequence of oral hypoglycemic and decreases the metabolism of phenytoin and warfarin. If a woman taking oral contraceptives were to begin taking phenobarbitone, inducing synthesis of hepatic drug metabolizing enzymes by phenobarbitone would accelerate metabolism of the contraceptive, thereby lowering its level by increasing the metabolism required for the metabolism of drugs, and it decreases the accumulation of medication concentration in the plasma (blood) serum level and finally cause drug failurity (Figure 6).
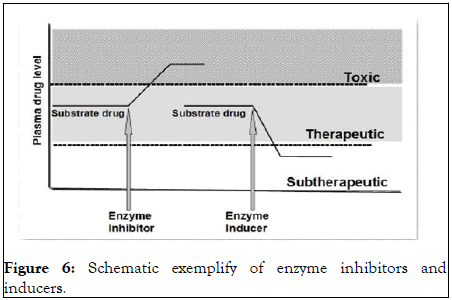
Figure 6: Schematic exemplify of enzyme inhibitors and inducers.
Drug excretion
The half-life of acidic medications will be prolonged in acidic urine as long as the medication is in its unionized form. Notwithstanding, the half-life of an acidic medication in basic urine is downgraded as long as the medication is in its ionized form. Medications such a like NSAIDs (e.g., ibuprofen) can deescalate the glomerular filtration rate, resulting in gradual excretion of medications that are eliminated by the kidneys. Aminoglycoside antibiotics (e.g., gentamicin) are removed relatively thoroughly by the kidney. The blood levels of aminoglycosides must be gingerly monitored in long-sufferings with de-escalated glomerular filtration rate (creatinine clearance) to prevent toxicity to auditory (hearing) and vestibular (balance) function. The anti-gout drug probenecid is occasionally bestowed with oral penicillin to accelerate the penicillin medication levels. Probenecid and penicillin contest for the identical cellular transporters in the tubule, so further penicillin is captured in the body. Medications such a like erythromycin that hinder P-gp perhaps escalate levels of P-gp substrates, such a like digoxin by precluding the secretion of digoxin into the tubule excretion of medications can be revamped by altering the pH of the urine. Weakly acidic medications become further ionized in basic urine. Ionized medications are not reabsorbed back into the blood and are excreted in the urine. In cases of aspirin toxicities, IV sodium bicarbonate is bestowed to alkalinize the urine so that a higher quantum of aspirin, a weak acid, will wait in the ionized state. Ionized aspirin is not reabsorbed and toxic aspirin levels are downgraded (Figure 7).
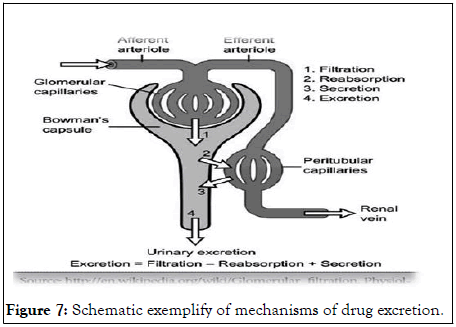
Figure 7: Schematic exemplify of mechanisms of drug excretion.
Drug interactions are frequently classified as pharmacodynamic or pharmacokinetic in nature. A PD DI is affiliated to the medication’s consequence on the body. An instance is the conflation of alcohol with medicines that antecedent sleepy condition. A PK DI is affiliated to the body’s consequence on the medicine. An instance is escalating in the systemic accumulation of a renal removed medicine as long as of renal insufficiency. A PK or PD consequences of medications on each distinctive, which can sequence, beyond desiderated outcomes, in downgraded effectiveness or escalated toxicity. DDIs are the consequences of lone medicine are revamped by the presence of a coincident medicine. Developed age, five or greater than five medications and more than one prescribers have been distinguished as pitfall agents for happening of potential DIs.
The authors acknowledged endnote-8, google scholar, medscape, wikipedia, and pubmed.
Data sources: Sources searched include google scholar, research gate, pubmed, NCBI, NDSS, PMID, PMCID, and cochrane database. Search terms included: Pharmacokinetic and pharmacodynamic mechanisms of drug interactions.
None.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Bereda G (2023) Pharmacokinetic and Pharmacodynamic Drug-Drug Interaction and their Implication in Clinical Management. J Clin Toxicol. 13:539.
Received: 13-Dec-2022, Manuscript No. JCT-22-20862; Editor assigned: 15-Dec-2022, Pre QC No. JCT-22-20862 (PQ); Reviewed: 29-Dec-2022, QC No. JCT-22-20862; Revised: 23-Mar-2023, Manuscript No. JCT-22-20862 (R); Published: 30-Mar-2023 , DOI: 10.35248/2161-0495.23.13.539
Copyright: © 2023 Bereda G. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.