
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Research Article - (2021)
Objectives: Heroin, prescription opiate and opioid overdoses have increased over the last decade in the United States. The potency of these drugs available in the communities has also increased. Our Emergency Department (ED) is in a high-volume urban hospital in Detroit, Michigan-Ascension St. John (St. John). This ED treats Acute Opioid and Opiate Overdoses (AOO) daily, often with ventilator support and administration of the antagonist, naloxone.
Methods: We performed a retrospective chart review to assess the demographic characteristics of patients with AOO in our ED from 2012 to 2018, and assessed variation and changes in naloxone dosing, treatment and disposition of patients. Charts were identified through pharmacy records of adult patients receiving naloxone in the critical care area of the ED. We excluded charts with diagnosis codes that did not relate to opiate, opioid or heroin toxicity, poisoning or drug abuse.
Results: We included 722 visits of 657 patients. AOO patients were more likely to be Caucasian (58.7%) and male (60.7%) than those presenting to the ED at large. Naloxone dosing was higher for males than females and was negatively correlated with age.
Conclusions: In congruence with national trends, AOO presentations and deaths increased over the last six years, despite increased naloxone administration, and naloxone being more available to pre-hospital personnel and laypeople.
Opiate; Opioid; Heroin; Fentanyl; Carfentanil; Overdose; Emergency department; Naloxone; Resuscitation
Overdoses involving heroin and prescription opiates and synthetic opioids (AOO) have been increasing for decades across the country [1] and in 2017 numbered 47,600, 68% of all drugs overdose deaths. Addictions, overdoses and deaths involving these drugs constitute an epidemic having profound social and economic implications. The impact on health care, especially on practice in the Emergency Department (ED) has been transformative; ED visits for these presentations increased from 19 to 63 per 100,000 ED visits from 1993 to 2010. As of 2017, mortality from AOO is still increasing. Not only has the number of AOO increased, but also the type and strength of opioid used in the communities have also changed, with an increasing amount of fentanyl and stronger synthetic opioids, driving increased mortality [2] and requiring changes in emergent treatment [3].
The Ascension St. John Hospital (St. John) ED is in a highvolume urban hospital in Detroit, Wayne County, Michigan. The St. John patient population draws from a socio-economic microcosm of the United States; from impoverished, urban neighborhoods, and first-ring suburbs that are variously economically-depressed, middle class and wealthy [4]. Our ED treats AOO daily, which is characterized by varying amounts of respiratory depression and obtundation. Treatment includes lifesaving ventilatory support (ranging from chin tilt/jaw thrusts, positive pressure ventilation to endotracheal intubation) and administration of the competitive μ opioid-receptor antagonist, naloxone. Many patients are discharged after resuscitation and observation, some require admission for acute hypoxic respiratory failure and some die in our ED from respiratory cardiac arrest, or subsequently after admission.
Surveillance data, published in the US Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report (MMWR) indicate that both heroin and fentanyl overdose deaths have been increasing in the Detroit, with fentanyl being detected as early as 2006 [5]. This examination of deaths in Wayne County found an increase in fentanylassociated deaths from two per month in 2005 to 24 per month in 2006. Acetyl-fentanyl deaths have also been reported noted a spike in carfentanil associated deaths using data from the medical examiner’s office of Wayne County over an eight-month period in 2016-2017.
We propose that management of AOO in our ED is changing [6] because of the general increase in recreational and prescription use of opiates and opioids and an influx of carfentanil and fentanyl into Detroit. Concurrently, naloxone became a mandated drug with Emergency Medical Services (EMS) and with law enforcement in Michigan in late 2014, during our study, and is now also available to laypersons in the community. Our objectives were to assess current practices and changes over time in dosing of naloxone, intensity of ventilator support and disposition of the patients. Further, as there is no standard of care for the management of AOO [7] we also assessed inter-physician variability in treatment, specifically naloxone dosing and observation time. Finally, we assessed how the population presenting in AOO differed demographically from our ED population at large.
Data Abstraction
We conducted a retrospective chart review of patients presenting to the St. John ED for AOO 2012-2018. Charts were initially included based on pharmacy records of naloxone being taken out of the medication cabinet for a patient in the resuscitation bay (i.e., the critical area of the ED). Patients triaged to a loweracuity bed in the ED with symptoms related to opiate use were not included in our study; this lower-acuity group includes patients not in respiratory distress and patients already adequately resuscitated from AOO by pre-hospital personnel or bystanders. Specifically, charts were abstracted from the EMR from January 1, 2012-August 30, 2018. This time period was chosen to include charts since the advent of electronic order inputs at our hospital, to decrease variation and bias in how information was recorded. We queried pharmacy records for milligrams (mg) of naloxone retrieved from the medication cabinet in the resuscitation bay, identifying visits with Medical Record Number (MRN) and Date of Service (DOS). ICD 9 and ICD 10 diagnoses codes associated with the patient visit were also extracted from these pharmacy records.
Charts were then expunged according to exclusion criteria: 1) patients less than 18 years of age; 2) records that were not coded for diagnoses related to AOO or identified as an AOO in physician notes; 3) naloxone not actually given and returned to the medication cabinet as identified via the pharmacy record or physician note. Additional data on sex, age, race, attending physician, time of presentation and disposition (left Against Medical Advice (AMA) from ED, discharged from ED, admitted to hospital under observation status, medical floor or Intensive Care Unit (ICU) or died in the hospital) were abstracted from the EMR when the data were entered electronically. If these data were not recorded in the EMR, they were obtained. Specific information that could only be obtained from individual chart review included amount of naloxone given pre-hospital (EMS personnel, police or bystander), whether a patient was intubated or put on Bilevel Positive Airway Pressure (BiPAP) by EMS or by ED personnel. In addition, diagnosis for each event was categorized: Heroin overdose; prescription opiate/opioid overdose; a combined overdose; opiate/opioid overdose where the agent was not otherwise specified (opiate/opioid NOS). Minutes of observation in the ED were post hoc calculated from the extracted data [8].
To standardize extraction of data from the physician notes, three authors (EP, MW, and KD) read 10% of the charts originally identified from the pharmacy data extraction. After this effort, we discussed any variation and discrepancies in our interpretation of the data. Given little variation and on-going active communication, two investigators (MW, KD) split the remaining charts to abstract and corroborate data. The principal investigator (EP) corroborated data in any chart flagged for additional review.
Statistical analyses
Categorical variables were described using percentages and 95% confidence intervals. Continuous and ordinal variables were described using medians and Interquartile Ranges (IQR). Variation in naloxone administration was evaluated using an ordinal/cumulative logit multi-level/mixed-effects model. Variation in observation time was evaluated using a gamma multi-level/mixed-effects model. Variation in disposition and diagnosis were evaluated using logistic multi-level/mixed-effects models. Mixed-effects models were used in order to account for clustering within providers as well as multiple visits per patients. P-values and 95% confidence intervals were computed using bias-corrected and accelerated bootstrapped estimates (5,000 resamples) [9]. The hypothesized that naloxone dosing began to increase in 2016 because of increased carfentanil in the community. To test this non-linear association with time, we included quadratic splines with a knot at 2016 in the regression analysis. We also extracted sex, age and race of patients from all visits to the St. John ED 2012-2018 to demographically compare the AOO population to the ED population at large. In this atlarge population, we excluded visits subsequent to the first visit, and excluded the AOO subgroup. We used chi-square tests to assess for population differences in terms of sex and race, and a t-test to compare age distributions between the AOO and ED atlarge; alpha-levels for significance were set at 0.05 analyses were conducted using SPSS (v25; Armonk, NY) [10].
We extracted 1790 charts associated with naloxone having been taken out of the medication cabinet in the resuscitation bay of the St. John ED 2012-2018. We eliminated charts of patients less than 18 years of age (26 charts), and those charts which did not have at least one ICD 9/10 code associated with AOO (219 codes, Appendix; 1012 charts) resulting in 752 charts involving likely AOO. We further eliminated 30 charts, based on individual review of the physician notes, which demonstrated that naloxone was not actually given, and/or the diagnosis was not actually associated with AOO. These data were then merged with extraction from the EMR of race, sex, date of birth, date of visit. The remaining 722 charts came from 659 different patients. Of the 722 visits, 612 (92.6%) were the single resuscitation event for a particular patient at our ED during our study period. 42 patients (6.4%) were resuscitated twice, with seven patients (1.1%) making three or more presentations to the critical area of our ED for AOO. The mean number of visits was 1.09 (SD 0.38), median 1, with a range of 1-6.
Demographics and other characteristics of the 722 patients are presented. The sample was 60.8% male and 39.2% female, had a median age of 39 years (IQR: 28-57), and was predominantly Caucasian (60.9%), then African American (38.8%).
The median dosage of naloxone was 2.0 mg (IQR: 1.2-2.8). Naloxone dosing increased over the study period (OR=1.25, 95% CI: 1.16-0.34, p<0.001). This remained significant when age, sex, and race were controlled (OR=1.25, 95% CI: 1.17-1.34, p<0.001) (Figure 1). When the splines were added, time was no longer significant (p=0.29); however, both the linear (OR=4.4, p<0.001) and quadratic (OR=0.58, p<0.001) splines were significant. This finding indicates that, prior to 2016, naloxone dosing was relatively stable. Beginning in 2016, naloxone dosing first increased and then decreased towards the end of the study period (Figure 1).
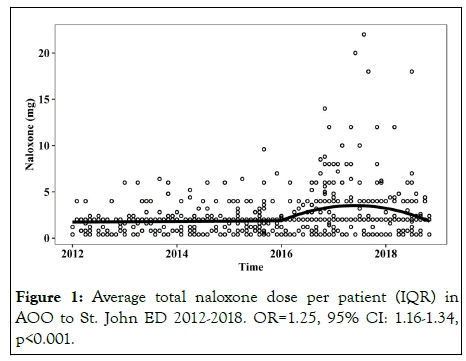
Figure 1: Average total naloxone dose per patient (IQR) in AOO to St. John ED 2012-2018. OR=1.25, 95% CI: 1.16-1.34, p<0.001.
The median/IQR naloxone doses for the first visit were 2.0 mg (1.2-2.7). For subsequent visits, the median doses were 2.0 mg (0.8-3.6) at the second visit, 3.2 mg (2.0-4.0) at the third visit, and 1.2 mg (0.4-4.0) at the fourth visit. The association between visit number and dosage was not significant (OR=1.22, p=0.91).
Naloxone dosing did not different between male and female patients (OR=0.82, p=0.14), nor as a function of patient race (OR=1.20, p=0.27). Age was significantly associated with dosing (OR=0.98, p=0.02) such that older patients received lower doses of naloxone.
BiPAP was used in 4.4% of cases. A logistic regression found a trend towards increasing BiPAP use over time; this trend was not significant (OR=1.24, 95% CI: 0.98-1.58, p=0.07). This trend did not change when age, race, and sex were controlled (OR=1.24, 95% CI: 0.98-1.57, p=0.07). Intubation was used in 15.1% of cases. The rate of intubation has remained relatively stable over time (OR=1.09, 95% CI: 0.97-1.22, p=0.15).
Discharged (40.4%), admitted to the ICU (24.8%) and to the hospital floor (20.2%) were the most common dispositions. Leaving AMA from the ED (OR=1.23, 95% CI: 1.05-1.44, p=0.01) and death in the hospital (OR=1.29, 95% CI: 1.04-1.62, p=0.02) became more common over the study period, whereas being sent to the ICU became less common (OR=0.90, 95% CI: 0.82-0.98, p=0.02). The trends for leaving AMA (OR=1.29, 95% CI: 1.10-1.51, p=0.001), death (OR=1.27, 95% CI: 1.01-1.59, p=0.04) and ICU admission (OR=0.84, 95% CI: 0.76-0.93, p=0.001) remained significant after controlling for age, sex, race, and naloxone dose. Being discharged (OR=1.03, 95% CI: 0.95-1.12, p=0.43), sent for observation (OR=0.78, 95% CI: 0.53-1.13, p=0.19) and being admitted to the floor (OR=0.95, 95% CI: 0.86-1.05, p=0.32) remained relatively stable over the study period.
The among-physician variability in the mixed-effects model was small and non-significant (intraclass correlation coefficient=0.03, 95% CI: 0-0.15, p=0.60) indicating that attending physicians did not differ with respect to the amount of naloxone administered. For patients discharged from the ED, the median observation time 3.7 hours (IQR: 2.4-5.4). A gamma regression determined that observation times were decreasing by 4.59% per year (95% CI: 1.09-8.06, p=0.02). This remained significant after controlling for age, race, and sex (β=5.44, 95% CI: 1.98-8.88, p=0.03). The between physician variability in observation time in the mixed effects model was small and nonsignificant (Intraclass correlation coefficient is 0.02, 95% CI: 0-0.25, p=0.50).
Heroin was the most common method of overdose (68%) followed by prescription opiates at 23.1%. A multinomial logistic regression determined that prescription opiates (OR=0.79, 95% CI: 0.72-0.88, p<0.001) and opiate overdose NOS (OR=0.76, 95% CI: 0.65-0.89, p<0.001) have decreased over time relative to heroin. The rate of combined (heroin prescription) overdose was stable relative to heroin (OR=1.06, 95% CI: 0.741.53, p=0.74).
207,475 different patients presented to the St. John ED 2012-2018. Therefore AOO represents 0.3% of (first) visits to our ED. Compared to this ED population at large, the patients presenting in AOO at the first visit (649) were more often male (60.7% for AOO vs. 44.3% for All ED, p<0.0001) and more often Caucasian (58.7% for AOO vs. 38.9% for All ED, p<0.0001) during the same time period. The AOO subgroup did not differ from the ED group in terms of mean age (p=0.3) of 33 patients that we determined had died by AOO during the course of our study (a hospital rate of 5% of individuals that presented in AOO), 22 (67%) had an autopsy with cause of death identified by Wayne County Medical Examiner (LH). 100% of these 22 deaths had a cause of death involving an opiate or opioid. Four patients (18%) also had fatal levels of cocaine. Seven patients (32%) had benzodiazepines in their serum, and 1 of 22 the patients had acetyl fentanyl.
We found not only an increasing number of presentations of opiate overdoses, requiring immediate resuscitation to our emergency department, but an increasing proportion of these patients died (2012-2018). Both of these findings mirror national trends [1]. The increase in proportion of deaths may be due to the increase in fentanyl, carfentanil and other higher potency opiates mixed with or replaced for heroin, as found in data from the Wayne County office of the medical examiner and nationwide. These trends have occurred while naloxone was made more available in the community [2], EMS and law enforcement. Despite increasing mortality, we found no increase in intubation or BiPAP use and a decreasing rate of ICU admission over time. This is in contrast in contrast with nationwide increase in ICU admissions from 2009-2015 [3]. The reason is unclear, but may be related to increased resuscitation of moderate cases outside of the ED (due to layperson and EMS access to naloxone), and our AOO cases reflecting increasingly more severe cases.
There is no gold standard of treatment of opiate overdose in the emergency department [4] however we found no difference in the dosing of naloxone among our ED attending physicians. An effective dose of naloxone depends on the opiate/opioid ingested, its amount and the patient’s weight. Therapeutic trials suggest the initial dose of naloxone for adults should be 0.04 mg, and this should be increased every two minutes to the maximum of 15 mg [5] intravenous dose of naloxone and found 48% recommended starting at a dose less than or equal to 0.05 mg, however 36% recommended an order of magnitude higher, and one reference suggested a 2 mg initial dose for patients under cardiac arrest. Our mean dose was 2.5 and up to 16 mg was used on one patient, who is within these guidelines; although notably above the suggested mean starting dose of 0.04 mg or 0.05 mg. In a prospective study [6] in Dayton, Ohio of 89 patients, mean dose was 0.1 (0.6 SD), however only after 5.8 mg on average was given prehospital; of note, patients unable to communicate and consent to their prospective study were eliminated, which likely biased low the dosing of naloxone. This all said, our data showed no significant variation in dosing of naloxone nor observation time among attending physicians, suggesting de facto standardization [7] documented a doubling of dosing of naloxone during an increase in heroin overdose presentations, that were suspected of being laced with carfentanil and fentanyl, and we also saw a an increase anchored around the carfentanil spike in our community in 2016.
However, this is in contrast to data from an Atlanta ED where patients overdosing with synthetic fentanyl vs. opiates did not differ in dose of naloxone required for resuscitation.
It is important to note that many of our patients had comorbid conditions including psychiatric disease, chronic pain and mental health problems. Many of our patients had also concomitant ingestions often of alcohol and benzodiazepines, the latter of which is strongly associated with death from AOO [8]. As a result, overdoses have increasingly become not straightforward heroin overdoses, but heroin is mixed with fentanyl, acetyl fentanyl, carfentanil and also include methadone, buprenorphine overdoses all of which have different duration of action. In addition, heating of fentanyl patches, injecting ground tablets and concomitant benzodiazepine use and concomitant over-ingestion of acetaminophen and resultant hepatotoxicity complicates and resuscitation unpredictably, as we see in our increasing variability of naloxone dosing.
We found that the average time to discharge from the ED for a patient with AOO was 4 hours and 47 minutes, and patient is observed for 4 to 5 hours before discharge. However the duration of action of a single dose of naloxone is far shorter than the duration of opiate medications, which can last for 12 hours [9], and thus appropriate observation is unclear and debated especially with increases in synthetic and illegally manufactured opioids. It has been suggested that four hours is sufficient time for observation to ensure that the patient will not relapse into respiratory depression aftereffects of naloxone have worn off completely after 1.5 hours. That our observation time declined from 2012-2018 may in fact ben secondary to papers published during this time about (lack of) utility of prolonged observation.
Patients presenting in AOO to our department differed in terms of sex and race from the population that presented to the ED as a whole. They were more likely to be Caucasian than African American, and more likely to be male. This has been seen in similar studies and reflect the demographics of heroin use and overdoses nationally [10] of those patients who presented in AOO. However younger patients were also resuscitated with higher doses of naloxone. It is unclear whether younger patients needed more naloxone or whether there was some bias in treatment.
Heroin overdose patients were younger than those diagnosis with prescription drug overdoses, also consistent with other studies. Overall, patients presenting with AOO, regardless of drug type, did not differ in age from our ED at large population.
Limitations of our study include that our data are an under representation of the number of opiate overdoses presenting to our ED, as they do not include those patients who did not require immediate resuscitation with naloxone or ventilator support, but instead were cared for in a regular bed in the ED and not in the critical care area. Further, our study did not include patients who were sufficiently resuscitated by bystanders, law enforcement or EMS, and therefore did not present to the critical care area.
Our data reflect nationwide trends in opiate/opioid overdoses and mortality. The number of opiate overdoses is still increasing in the United States despite awareness of the epidemic, public health interventions, and existence of an effective antidote used in the community. More patients are presenting in acute opiate/ opioid overdose to our urban emergency department between (2012-2018), and a higher proportion of these patients are dying. This is despite more aggressive treatment with the opiate antagonist and ventilator support and higher levels of care (i.e., increasing rate of admission). This is also despite more naloxone being available in the community and with first responders. Patients presenting to the ED are more likely to be Caucasian and male compared to the ED population at large, and these patients are also resuscitated more aggressively.
Citation: Peacock E, Moran T, Wheaton M, Daouk K, Hlavaty L, Dunne R (2021) Patterns of Presentation and Treatment of Opiate Overdoses at the Urban-Suburban Divide. J Clin Toxicol. S20:001.
Received: 19-Nov-2021 Accepted: 03-Dec-2021 Published: 10-Dec-2021
Copyright: © 2021 Peacock E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.