Clinical & Experimental Cardiology
Open Access
ISSN: 2155-9880
ISSN: 2155-9880
Research Article - (2022)Volume 13, Issue 12
Background: Atrial Fibrillation (AF) is a common health problem associated with valvular heart disease. AF is abnormal atrial rhythm which is associated with unsynchronized atrial contraction that leads to loss of atrial kick and subsequently affects the stroke volume in around 25%. Resistant cases for control with medication required ablation percutaneous or simultaneously with valve surgery.
Aim: Is to assess the outcome after ablation with minimal invasive technique in association with mitral and tricuspid valve surgery.
Method: This is a retrospective study enrolled n=220 patients who underwent Cox Maze through minimal invasive approach in association with mitral and/or tricuspid valve surgery.
Result: this study included 220 cases according to the study design, mean age was 53.1 ± 9.1 years and most of the cases were 59.1% of male gender. n=63 patients under went mitral valve repair, n=157 patients needed mitral valve replacement 132 of them had tissue valve, and 179 had a concomitant tricuspid valve surgery.
Conclusion: Cox Maze procedure is effective with low recurrence rate of AF in cases done through minimal invasive mitral and tricuspid valve surgery.
Atrial fibrillation; Minimal invasive; Abolition
AF: Atrial Fibrillation; LAA: Left Atrial Appendage; CCT: Cross Clamp Time; CPB: Cardiopulmonary Bypass Time; MIVS: Minimal Invasive Valve Surgery; CABG: Coronary Artery Bypass Graft; PM: Pacemaker; ATA: Atrial Tachyarrhythmias; ICU: Intensive Care Unit; LOS: Length of Stay; LA: Left Atrium
The Cox Maze technique has been established as surgical strategy for atrial fibrillation with impressive results, since it has been introduced in 1987 by James Cox who made a multiform incision on the left and right atrium aiming to mess up the re-entrant circuits thinking that it is the cause of atrial fibrillation, many modifications were performed later using different ablation methods like bipolar or unipolar Radio Frequency (RF), laser, ultrasound and cryosurgery [1,2]. Atrial Fibrillation (AF) is common with mitral valve disease, so usually this procedure is classically performed during mitral valve surgery, via traditional sternotomy with curing rate up to 90% [3]. Recently with less invasive techniques, minimal invasive approach turned into popular for most of surgeons to do Maze procedure, with debate of its result and better approach [4,5]. In this study the aim is to evaluate the results for Cox Maze procedure associated with mitral and tricuspid valve surgery via minimal invasive approach.
Surgical technique
Under general anesthesia with complete set up and patient monitoring. All cases underwent the minimal invasive protocol for incision and cannulation to proceed for surgery for mitral valve surgery either (replacement or repair) in addition to tricuspid valve surgery if needed. During cardiopulmonary bypass, starting with right atrial (Figures 1-3) on the beating heart then left atrial were achieved on arrested heart, linear ablation usually done by using Medtronic bipolar radiofrequency clamp to replace the incisions of Cox maze III, while the unipolar ablation Medtronic Cardioblate XL pen was used for the tricuspid and mitral valve annuli, and the coronary sinus (Figure 4). Plication of LAA (left atrium appendage) at the end of the procedure were done using prolene suture in cases with large left atrium and LAA (Figure 5). After weaning off bypass TEE (Trans Esophageal Echocardiography) were done in all cases to confirm success of surgical technique and valves. We considered the guidelines definition for AF paroxysmal, persistent or long standing, all pre-operative and post-operative profiles data were determined, follow up ECG with or without 24 hours Holter monitor (in cases of doubt symptoms) were recorded postoperatively, at 3 months, 6 months, and one year. We considered AF Recurrence if any episode of AF or atrial flutter recorded for more than 30 seconds. Early if before 3 months and late if after 3 months, we expressed success Cox Maze procedure if there is no recorded of Atrial Tachyarrhythmias (ATAs). Anti-arrhythmic drugs and warfarin were prescribed for all patients during the first 3 months, and then continued only for those with AF recurrence, warfarin also was continued for patient had mechanical valve.
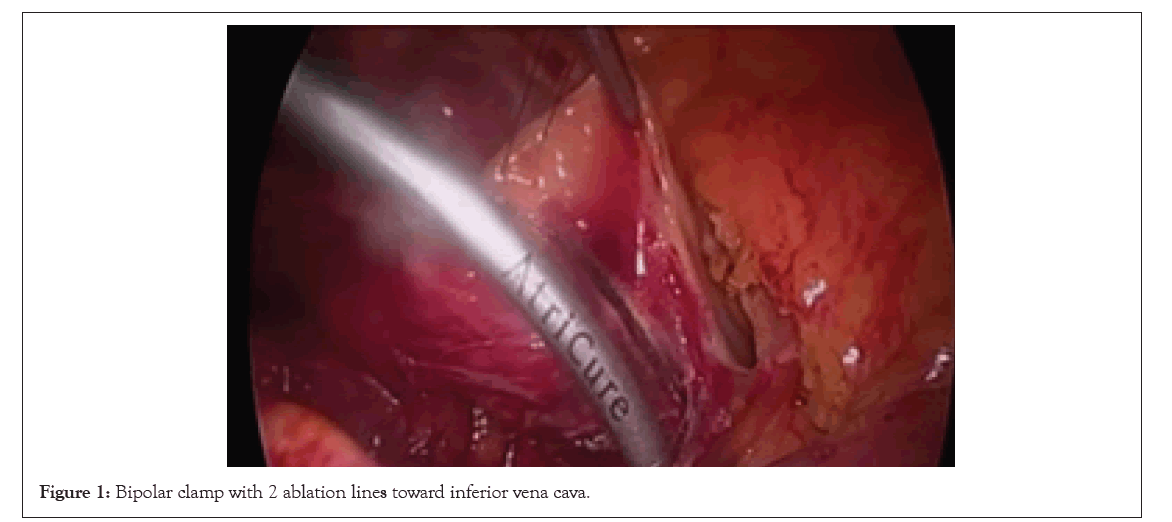
Figure 1: Bipolar clamp with 2 ablation lines toward inferior vena cava.
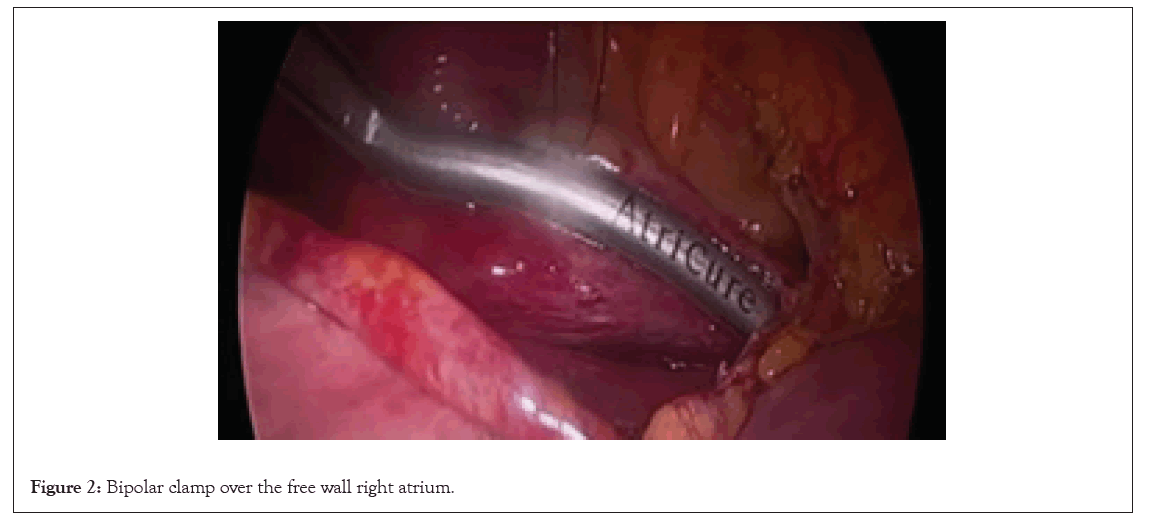
Figure 2: Bipolar clamp over the free wall right atrium.
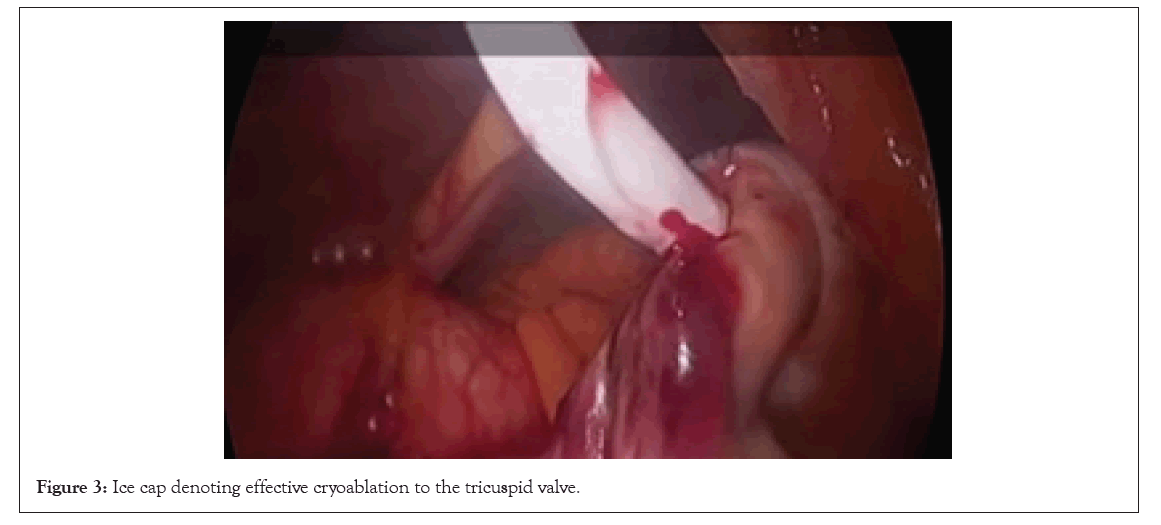
Figure 3: Ice cap denoting effective cryoablation to the tricuspid valve.
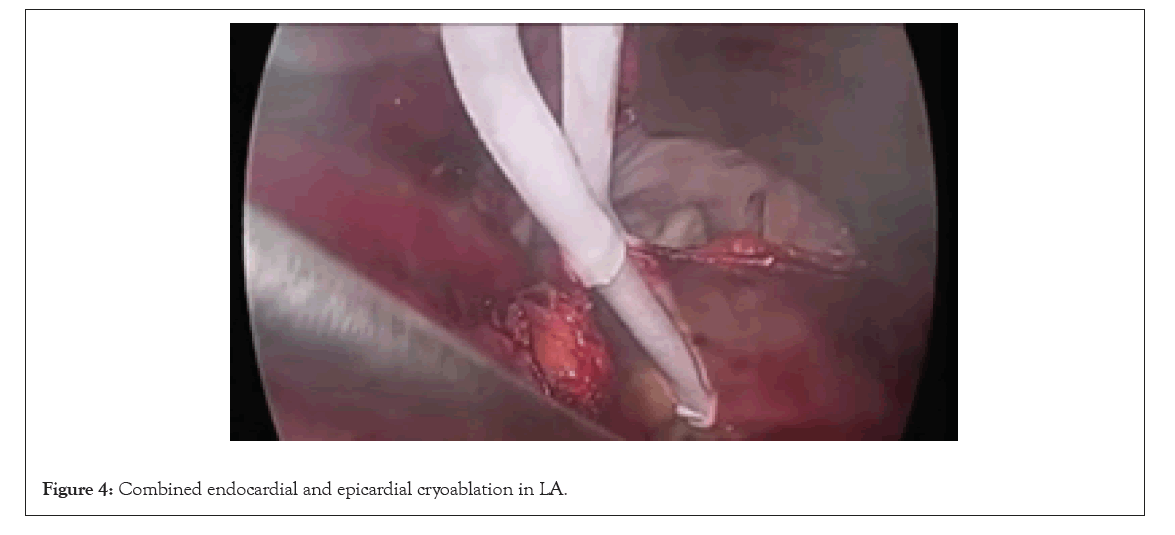
Figure 4: Combined endocardial and epicardial cryoablation in LA.
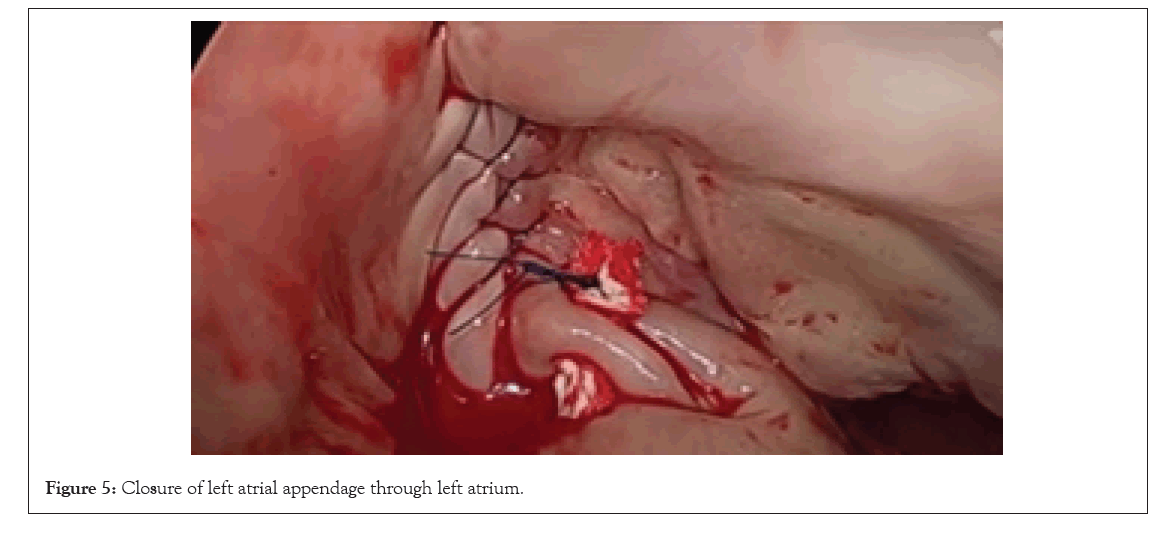
Figure 5: Closure of left atrial appendage through left atrium.
Statistical analysis
We statistically analysed the collected data aiming to describe our results, in the form of mean or the average alongside with the standard deviation using SPSS 11.0 for windows.
| Variables | n=220 |
|---|---|
| Mean age (years) | 53.1 ± 9.1 |
| Male gender (%) | 130 (59.1%) |
| AF duration (years) | 7.3 ± 6.0 |
| Paroxysmal AF (%) | 82 (37.2) |
| Persistent AF (%) | 113 (51.4) |
| Longstanding persistent AF (%) | 25(11.4) |
| NYHA Class 3 or 4 (%) | 137 (62.3) |
| Mean LVEF (%) | 50 ± 22 |
| LA diameter (cm) | 5.5 ± 2.8 |
Note: AF: Atrial Fibrillation; NYHA: New York Heart Association; LVEF: Left Ventricular Ejection Fraction; LA: Left Atrium.
Table 1: Patients’ characteristics.
| Procedure types | Total patients |
|---|---|
| Mitral valve Replacement | 157 (71.3%) |
| Mechanical | 25 (11.3%) |
| Tissue | 132 (60%) |
| Mitral valve repair | 63 (28.6%) |
| Tricuspid valve: | |
| Repair | 177 (80.5%) |
| Replacement tissue valve | 2 (0.9%) |
Table 2: Distribution of cases according to surgical procedure concomitant with Cox Maze procedure.
| Variables | Total patients (%) |
|---|---|
| Mean CMIV procedure time (minutes) | 15 ± 7 |
| Mean CCT (minutes) | 97 ± 37 |
| Mean CPB (minutes) | 125 ± 6 |
| Permanent PM | 1(0.45%) |
| Myocardial infarction | 0 (0.0%) |
| Stroke | 2(0.9%) |
| Reoperation for bleeding | 7(3.2%) |
| Renal failure requiring dialysis | 4(1.8%) |
| Mortality intra-operative | 0 (0.0%) |
| Mortality post-operative | 3 (1.3%) |
| Median ICU LOS in days (range) | 1 (1-15) |
| Median hospital LOS in days (range) | 7 (4-23) |
Note: CCT: Cross Clamp Time; CPB: Cardiopulmonary Bypass Time; PM: Pacemaker; ATA: Atrial Tachyarrhythmias.
Table 3: Operative and post-operative outcomes.
| Recurrence | Total patients (%) |
|---|---|
| Early ATA | 31 (14.1%) |
| Late recurrence | 23 (10.45%) |
| Freedom from recurrence after one year | 178 (80.9%) |
| Total Patients continue on warfarin | 54 (24.5%) |
| For recurrent AF | 42 (19.09%) |
| for MV+r AF | 13 (5.9%) |
Note: Early ATA included atrial fibrillation and atrial flutter.
Table 4: Percentage of recurrence and need for anticoagulation.
Minimal invasive open-heart surgery is the new trend nowadays in different surgical management. This need training, financial support and to increase the orientation about these approaches [1,2], as well the met-analysis to prove the outcome of minimal invasive techniques. During minimal invasive mitral valve or tricuspid valve surgery Cox-Maze procedure can be done easily with accepted results and almost no significant morbidity or mortality, without significant impact on, bypass or cross clamp times [6]. Using bipolar radiofrequency clamp in sequences with unipolar radiofrequency ablation for the areas cannot be reached by bipolar clamp like coronary sinus, mitral and tricuspid annulus minimize the time needed for doing the procedure and technically will be easier to do complete Cox-Maze IV, through mini thoracotomy incision (Table 4) [7].
In early trials for some surgeon to modify the procedure they were concentrating on pulmonary vein isolation, to minimize the complexity and the challenge to do the complete procedure through the small right intercostal incision [8,9]. Failure of the entire anatomical isolation of left atrial considered one of the risk factors for recurrent atrial arrhythmias as mentioned by Gillinov AM, et al [10]. Also left atrial size reduction in patients with large left atrial size, is not easy to be performed through minimal invasive approach. It is not routinely done through minimal thoracotomy incision. Some literature [11] considered LA (Left Atrium) size reduction helps to reduce the recurrence of AF in those with left atrial size 7 cm or more. Kamata J. et al [12] concluded that large left atrial size is a significant predictor for Cox Maze procedure failure, on the other side few literatures concluded that performing left atrial reduction did not prevent recurrence. Strict medication with careful follow up post-operative decreases any sort of atrial dysrhythmia. Early ATAs also increase the risk of recurrence as mentioned by Byrd GD, et al [13], so we managed early ATAs with chemical and electrical cardio version as early and aggressive as possible during the period between 1 and 4 weeks post operatively. In this study there were n=12 cases who were controlled and resumed sinus rhythm out of n=31 patients had early ATAs. Usually, early ATAs occurs due to post-operative myocardial inflammation produced by ablation (robust inflammatory response) as mentioned by Ishii Y, et al [14,15]. Our study revealed high success rate for Cox-maze performed through minimal invasive approach during concomitant mitral and tricuspid valve surgery, which reached up to 80.9%. This low recurrence rate is comparable percent with most of the centres.
Cox Maze procedure in concomitant mitral or tricuspid valve surgery is safe, affective and had low recurrence rate. Surgical treatment of dysrhythmia is essential to be available in most of the cardiac centres especially those with high rate of valve surgery. The need for anticoagulation can be stopped in saucerful cases after ablation without recurrence AF and with valve repair or tissue valve had been used, but this need further follow up for more studies.
The set for ablation is not available in many centers and need more training; as well the study needs multi-center analysis to prove the outcome. Ischemic cases with AF and isolated cases with AF not included in this study.
Consent for publication: Approval from instructional review board was taken as well-informed consent for publication was taken with confidentiality of patents data. All are available if requested.
No competing conflict of interests.
Self-funded.
Citation: Shaalan AM, Alhuthaifi A, Alfaifi SH, Ezeldin TH (2023) Outcome after Cox-Maze Procedure during Minimal Invasive Surgery for Mitral and Tricuspid Valves. J Clin Exp Cardiolog.13:763.
Received: 27-Dec-2022, Manuscript No. JCEC-22-21179; Editor assigned: 30-Dec-2022, Pre QC No. JCEC-22-21179; Reviewed: 17-Jan-2023, QC No. JCEC-22-21179; Revised: 24-Jan-2023, Manuscript No. JCEC-22-21179; Published: 31-Jan-2023 , DOI: 10.35248/2155-9880.22.13.763
Copyright: © 2023 Shaalan AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.