Journal of Infectious Diseases & Preventive Medicine
Open Access
ISSN: 2329-8731
ISSN: 2329-8731
Short Commentary - (2020)Volume 8, Issue 2
Infectious uveitis is a common entity representing 15–20% of all uveitis cases worldwide. The aim of this short commentary is to provide a summary of the identification, treatment, and complications associated with syphilitic uveitis. While syphilitic uveitis may involve any part of the eye from cornea to optic nerve and retina, the most devastating complications are represented by posterior segment involvement. As syphilitic uveitis can mimic various types of immun-mediated uveitis, clinical suspicion, recognizing certain clinical features including multi-modal imaging characteristics are crucial for visual recovery and preservation.
Infectious uveitis; Syphilis; Ocular syphilis
Syphilis which is common sexually transmitted disease caused by a spirochete called Treponema pallidum, can spread to almost every part of the body if left untreated [1]. Current guidelines reported by the World Health Organization show a high incidence of syphilis in worldwide. Approximately 12 million new cases of syphilis is diagnosed annualy more than 90% of whom is reported from developing countries [2].
The diagnosis of syphilis is challenging for clinicians globally. The sensitivity and specificity of dark-field microscopy is relatively 90% and 100% respectively in the diagnosis of disease. But its function is limited. The popularity of polymerase chain reaction is growing that T. pallidum genomes is revealed from ulcerative lesions, lymph node aspirates, cerebrospinal fluid, blood and vitreous aspirates [3]. Nevertheless, in daily practice, ratification of the diagnosis relies extensively on serological tests. Serological tests can be divided into two groups: non-treponemal tests are usually used for screening and monitoring the disease activity. Unfortunately tests false positive (due to cross-reactivity) and false negative (in HIV-positive patients) results are not uncommon with non-treponemal tests. Therefore treponemal tests are used for confirmation of the diagnosis in case non-treponemal tests are positive [4].
Syphilis, is also called as 'the great imitator' due to its ability to simulate clinical manifestations of various other diseases. The disease may influence many systems of the human body including the skin, heart, nervous system and the eye. Ocular syphilis may occur in both immunocompetent and the immunosuppressed patients. The severity of symptoms also varies greatly and can include tearing, mild to moderate pain, vision loss, floaters, flashing light or photophobia. Syphilis has been reported to influence almost every part of the eye. Ocular involvement does not commonly occur in patients with primary syphilis, except for chancres of eyelid and conjonctiva. The average time between acquisition of syphilis and the initiation of the first ocular symptom is approximately 6 weeks [5]. Syphilitic conjunctivitis is manifested by marked congestion and chemosis. The incidence of conjunctivitis has decreased dramatically in the post-antibiotic era. Interstitial keratitis is a rare finding which is usually bilateral and become symptomatic as watering and photophobia. Scleritis is generally detected in secondary or tertiary stage of the illness. The manifestation of posterior segment involvement is broad. Panuveitis is generally the most common finding in ocular syphilis. Nevertheless, it has been reported that panuveitis is the predominant diagnosis in immunosuppressed patients, whereas, posterior uveitis is the most common finding in immunocompetent patients [6]. The largest ocular syphilis series in the literature which was reported by Furtado at al stated that posterior uveitis (76.2%) is the most common feature in ocular syphilis [7]. The most common presentation (75%) of posterior ocular involvement; chorioretinitis, generally affects the posterior pole and mid-periphery accompanied with vitritis [8]. The retinal or choroidal infection commonly occurs during the secondary stage of syphilis. Optic nerve involvement may be unilateral or bilateral resulting in perineuritis, anterior or retrobulbar optic neuritis and disc edema [9].
The features of ocular syphilis determined by fundus florescein angiography (FFA), and indocyanine green angiography (ICGA) are well documented in the literature. The most common features detected on FFA include retinal/capillary leakage, vascular wall staining, disc hyperfluorescence and macular edema, indicating a nonspecific ocular inflammation. On the other “Leopard spots”, late-phase scattered hyperfluorescent spots and persistent staining of retinal vessels have been suggested to be characteristic findings for syphilitic uvetitis. On ICGA dark dots, indicating an active lesion and hot spots, suggesting a long duration of disease may also be seen [10]. The optical coherence tomographic findings include disruption of the ellipsoid zone, thickening and irregularity of the retina pigment epitelium, subretinal fluid and increase in optic nerve head thickness [11]. Our case presented with dense vitreous hemorrhage in the right eye blocking adequate retinal visualization, 10 days after the intravitreal dexamethasone injection. The patient had also received intravitreal dexamethasone injection for the left eye 2 months priorly. Bilateral anterior chamber cell reaction and especially white colored patches compatible with retinal necrosis in the left eye reminded us probable infectious causes (Figure 1).
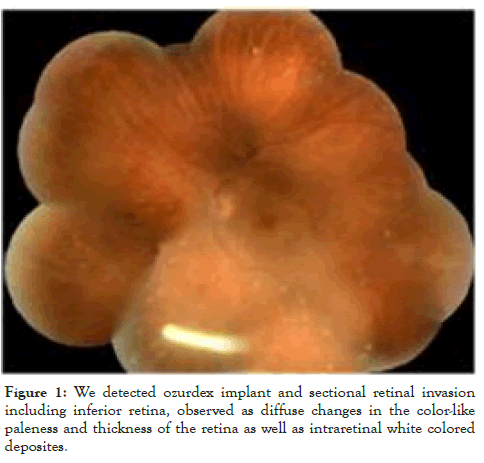
Figure 1: We detected ozurdex implant and sectional retinal invasion including inferior retina, observed as diffuse changes in the color-like paleness and thickness of the retina as well as intraretinal white colored deposites.
A full thickness necrotizing retinitis is almost always associated with infectious uveitis causes including herpes viruses, HIV, syphilis and CMV.
The diagnosis of ocular syphilis requires a high clinical suspicion as it can mimic a variety of eye diseases. The current treatment guidelines suggest the use of parenteral penicillin G regardless of the stage of syphilis [12]. A single dose of intramuscular benzathine penicillin G 2.4 million units is sufficient for early stage of disease without neurological or ophthalmic involvement. However in case of neurosyphilis the treatment of choice is intravenous aqueous crystalline penicillin G 18-24 million units per day for 10 to 14 days [13]. In patients with penicillin allergy, 100 mg doxycycline twice a day orally for 28 days or ceftriaxone 2 g daily either intramuscularly or intravenously for 10 to 14 days is recommended [12]. Ocular syphilis should be treated as neurosyphilis, even if the cerebrospinal fluid study seems normal. Systemic steroids have not been demonstreated to be advantageous in the treatment of syphilis. Nevertheless, supporting with steroid therapy may diminish the intensity of inflamation a few days after the initiaton of antibiotic treatment to prevent Jarisch-Harxheimer reaction. Topical steroids can be used for syphilitic iridocyclitis and interstitial keratitis. The use of intravitreal corticosteroids in the treatment of syphilitic uveitis, however, is rare, due to concerns of syphilis reactivation. Therefore infectious causes of uveitis should be ruled out prior to periocular or systemic steroid applications. Accordingly there are several reports in the literature one of which is our case defining worsening of untreated ocular syphilis after intraocular steroid injections [14-16]. In our case report the patient had undergone bilateral intravitreal dexamethasone implantation 10 days before in the right eye and 2 months before in the left eye without penicillin treatment. Nevertheless, Lautredou at al reported successful utilization of intravitreal corticosteroid therapy for uveitis-related with cystoid macular edema for patients with treated syphilitic uveitis [17]. All patients with ocular syphilis should be tested for HIV due to the high rate of co-infection. In the presence of concomitant HIV infection, anti-retroviral theraphy should be used [18].
In conclusion diagnosis of ocular syphilis is challenging due to its ability to mimic ocular manifestations of various systemic diseases. Early diagnosis with a high clinical suspicion together with appropriate treatment are critical in achieving good visual outcomes and low recurrence rates. Regular follow-up is also advised on account of recurrence or relapse can happen in spite of completing treatment.
Citation: Yilmaz S, Yildiz AM, Avci R (2020) Ocular Syphilis- An Unusual Case Presentation of the Great Imitator and Minireview of the literature. J Infect Dis Prev Med. 8:198. DOI:10.35248/2329-8731.20.08.198.
Received: 18-Mar-2020 Accepted: 07-Apr-2020 Published: 15-Apr-2020 , DOI: 10.35248/2329-8731.20.08.198
Copyright: © 2020 Yilmaz S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.