Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Case Report - (2020)Volume 10, Issue 2
A 72 year old lady, who presented with blurry vision in both eyes, was diagnosed based on ophthalmological exam as having occult Giant Cell Arteritis (GCA) without any systemic symptoms despite the fact that she did not respond initially to intravenous steroids. Patient was directly switched to Tocilizumab to notice marked improvement in her symptoms afterwards. Interleukin-6 has been shown to be a key cytokine in GCA, and that explains why Tocilizumab, a humanized monoclonal antibody targeting interleukin- 6 receptor, was FDA approved for the treatment of GCA. However, encountering a patient with occult GCA, having almost complete blindness, responding acutely to Tocilizumab after failing initial high dose steroid therapy, such as in the present case, was not reported before. In addition, the marked improvement in the symptoms, along with the patient being able to avoid long term steroid side effects, raises the subject of whether Tocilizumab should be attempted promptly in patients with steroid resistant occult GCA.
Occult giant cell arteritis; Tocilizumab; Steroids
Giant cell arteritis (GCA) is the most common primary vasculitis in adults, affecting almost exclusively individuals above 50 years of age. The mainstay of treatment remains glucocorticoids which is usually introduced promptly to prevent vision loss, the most feared complication of this systemic illness [1].
However, despite the use of corticosteroids, vision loss may still occur in 14% to 20% of patients with GCA [1]. Tocilizumab, an interleukin-6 receptor alpha inhibitor, was previously shown to be effective when studying the rates of GCA relapse during glucocorticoid tapering [2]. However, what if we encountered a devastating case of vision loss secondary to GCA with no improvement on initial high dose intravenous steroids?
We describe a 72-year-old lady who presented to the ophthalmologist with a two week history of sudden visual loss in the right eye noted upon awakening. She then presented to the ophthalmology clinic one week later and was found to have a counting finger vision near face in the right eye and 20/50 vision in the left eye which was asymptomatic at the time.
Her exam revealed a swollen optic nerve head on the right side with the left optic nerve head looking within normal ranges (Figure 1). Magnetic resonance imaging (MRI) of the brain was reported to be normal. With the impression of anterior ischemic optic neuropathy in the right eye as per the ophthalmologic exam, laboratory blood tests including ESR, CRP, CBC, ACE, ANCA, PPD, VDRL, and TPHA were done. The erythrocyte sedimentation rate (ESR) was 89 mm/hr and hemoglobin was 8.3 g/dl with normal mean corpuscular volume (MCV), while the rest of the blood tests were within normal limits.
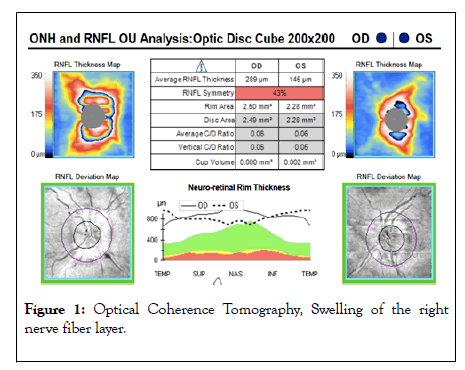
Figure 1: Optical Coherence Tomography, Swelling of the right nerve fiber layer.
Meanwhile, the patient started developing a decrease in her vision of the left eye and was hospitalized again. Four-day course of high dose intravenous (IV) Methylprednisolone (1 g/day) were given. The visual acuity of the left eye kept deteriorating despite treatment with swelling of left nerve fiber layer (Figure 2). The patient did not report any history of headaches, eye pain, joint pain or swelling, skin rash, jaw claudication, or constitutional symptoms such as fever, night sweats or weight loss since the early beginning. Upon physical examination, she had a sluggish pupillary light reflex bilaterally, with a palpable pulse and no tenderness or dilatation over both temporal arteries pulse over both temporal arteries was palpable. The rest of the neurological exam was unremarkable.
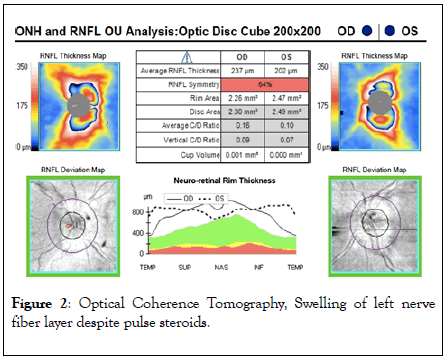
Figure 2:Optical Coherence Tomography, Swelling of left nerve fiber layer despite pulse steroids.
The metabolic and serologic profiles including anti Aquaporin 4 antibody titers, and cerebrospinal fluid studies, including oligoclonal bands, were all unremarkable. Repeated MRI brain and orbit with gadolinium did not show any pathology. Bilateral temporal artery biopsies (1.5 × 0.15 cm) failed to show any evidence of arteritis. She was then started on IV Tocilizumab (8 mg/kg) with immediate improvement in her vision after few hours. She was able to ambulate on her own, her ESR dropped down from 86 to 7 mm/hr, and funduscopic exam was stable during the first 2 days post Tocilizumab, to start improving after, with some decrease in optic disc edema in the right more than the left eye. She was diagnosed as having occult.
GCA is an immune-mediated granulomatous inflammation of the walls of medium and large-sized arteries, occurring mostly in people beyond the age of 50 years [3]. Our patient did not fulfill the diagnostic criteria for GCA, therefore she was referred to as “Occult” GCA which usually occurs in about 20% of the cases [4]. It is defined as ocular involvement, manifesting with early massive visual loss (counting fingers vision or worse), sequential vision loss within days or weeks, and white disk edema, without any associated systemic features as headache, scalp tenderness, jaw claudication, ear or neck pain, low-grade fever, weight loss, malaise, joint or muscle pain and swelling [4].
The challenge was mainly related to the diagnosis from the rheumatology and neurology point of view since our patient did not have any systemic symptoms of GCA, with no inflammatory changes over the wall of both temporal arteries as per the biopsies taken, in addition to the fact that she did not have any improvement in her vision after receiving high dose of steroids. That is when the ophthalmologic examination came to prove that it was a case of GCA with the theory that the bilateral vision loss might have been secondary to the sequential onset of central retinal artery occlusion, anterior ischemic optic neuropathy or less likely, posterior ischemic optic neuropathy, in any combination [5, 6].
Tocilizumab (8 mg/kg IV) was attempted after failure of steroids [7], with marked improvement shortly after. She is still maintained on monthly intravenous (IV) Tocilizumab since 18 months but was spaced to every 6 weeks after 12 months, with persistent good response. Her current vision is counting fingers at 2 meters in the right eye and 3 meters in the left eye and her optic nerve heads are pale.
Interleukin-6 has been shown to be a key cytokine in the pathogenesis of GCA [8]. Tocilizumab, a humanized monoclonal antibody targeting interleukin- 6 receptor, is FDA approved for the treatment of GCA [8]. However, encountering a patient with occult GCA, having almost complete blindness, responding acutely to Tocilizumab after failing initial high dose steroid therapy, such as in the present case, was not reported before. In addition, the marked improvement in the symptoms, along with the patient being able to avoid long term corticosteroid side effects, raises the question whether Tocilizumab should be attempted promptly from the early beginning in patients presenting with severe acute visual loss due to GCA.
No statistical analysis was conducted.
The authors have nothing to declare.
Rola Hamam and Tarek El Halabi contributed equally to the manuscript. They, along with Mira Merashli, did the literature review, clinical follow up and case write up
Maria Ramia: Clinical follow up
Maan El Halabi: Case write up
Not applicable.
The authors thank Dr. Marwan Atallah for his clinical contribution.
Reports no disclosures
Citation: Hamam R, EI Halabi T, Ramia M, EI Halabi M, Merashli M (2020) Occult Giant Cell Arteritis Responding Promptly to Tocilizumab after Failure of High Dose Corticosteroid Therapy. Rheumatology (Sunnyvale). 10:260. DOI: 10.35248/2161-1149.20.10.260.
Received: 09-Apr-2020 Accepted: 23-Apr-2020 Published: 30-Apr-2020 , DOI: 10.35248/2161-1149.20.10.260
Copyright: © 2020 Merashli M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.