Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Research Article - (2015) Volume 5, Issue 4
Objective: Visceral obesity is an etiological factor and a marker of poor prognosis in acute pancreatitis (AP). Non-Alcoholic Fatty Liver Disease (NAFLD), a marker for visceral obesity, has also been recognized to have a stronger correlation to poor outcomes. With this study, we aim to assess the role of NAFLD as an etiologic factor in patients with AP.
Materials and Methods: In this retrospective electronic medical record (EMR) based case control study of 530 non-alcoholic adults were classified into cases with acute pancreatitis and controls without pancreatitis. Further subgroup was classified based on gallstone formation as an etiology of pancreatitis. Data was evaluated with McNemar’s Test.
Results: Results showed that patients with AP due to Gallstones had a higher incidence of NAFLD as seen on abdominal imaging [OR=1.688, p=0.0235 (CI: 1.070-2.701)], but Patients with AP due to unclear etiology did not have statistically significant higher rates of NAFLD [OR: 1.400, CI: 0.688 – 2.919]. Patients with AP due to all etiologies combined had higher incidence of NAFLD [(OR: 1.596, CI: 1.094-2.349, P-value 0.0145)].
Conclusion: We conclude from this study shows that NAFLD may be an independent risk factor for development of acute pancreatitis. It is also possible that NAFLD may have pathophysiologic interplay with formation of gallstones that is a known risk factor for acute pancreatitis.
Keywords: Acute pancreatitis; Etiology; Non-alcoholic fatty liver disease; Obesity; Risk factor
Acute pancreatitis (AP) is one of the most common diseases of the gastrointestinal tract. The most common cause of AP is gallstones and alcohol. Other causes include mediations, infectious agents and metabolic causes like hypercalcemia and hyperparathyroidism [1]. Recent studies have identified obesity as an etiological factor and a marker of poor prognosis in AP. Visceral obesity has also been recognized to have a stronger correlation to poor outcomes. Non-Alcoholic Fatty Liver Disease (NAFLD) is a condition, which is characterized by the deposition of lipid in the hepatocytes of the liver parenchyma and thus is a marker of visceral obesity. The prevalence of NAFLD is estimated to be 10-24% in various populations [2]. The association between NAFLD and AP has yet not been studied. We hypothesize that visceral obesity of which NAFLD is a marker may be a strong risk factor in the development of AP because of the pro-inflammatory nature of fat. The knowledge of the co-relation between NAFLD and AP thus can help us determine the risk of development of AP in patients with NAFLD after an ultrasound.
Thus the aim of this study is to assess the role of NAFLD as an etiologic factor in patients with AP.
In this retrospective electronic medical record (EMR) based case control study, data from our institution on 530 non-alcoholic adult hospital admissions was analyzed. Approval from the Institutional Review Board was obtained prior to initiating the study from our institution. As per the American Association for the Study of Liver Disease (AASLD) criteria, significant alcohol consumption was defined as >21 drinks per week for men and >14 drinks per week for women over a minimum of 2 year period [3]. On admission, abdominal imaging in form of abdominal ultrasound (AUS) was available. The diagnosis of NAFLD or its exclusion was based solely on radiologist’s interpretation of the abdominal imaging study. The diagnosis of AP was made based on the American College of Gastroenterology guidelines [1].
The first group consisted of non-alcoholic patients diagnosed with AP. The first group was further divided into 2 subgroups with the etiology of AP attributed to gall stones or AP due to unclear etiology. A review of the abdominal imaging was performed to look for the presence of absence of NAFLD. The second group consisted of non-alcoholic patients admitted to the hospital for all diagnosis except AP who underwent abdominal imaging for other reason. These patients were matched for Age, Sex and Race with the first group and subgroups. They were also matched for Body Mass Index (BMI) with the first group. A review of the abdominal imaging was also performed in these patient too look for the presence of absence of NAFLD. Data from both these groups was analyzed and compared using the McNemar’s test. P-value was considered significant for values lower than 0.05. Only study participants had access to patient information.
The results are tabulated in Table 1.
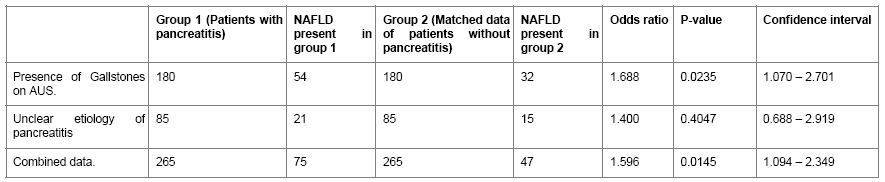
Table 1: Data analyzing the association of NAFLD and Acute Pancreatitis in patients matched for Age, Sex and Race.
Table 1 compares the incidence of NAFLD in the two groups of non-alcoholic patients with and without AP. Patients with AP due to Gallstones had a higher incidence of NAFLD as seen on abdominal imaging and this this difference was statistically significant as a risk factor with a P value of 0.0235 (CI: 1.070-2.701). Patients with AP due to unclear etiology had higher incidence of NAFLD as seen on abdominal imaging but this difference was not statistically significant as a risk actor (CI: 0.688-2.919). NAFLD as a risk factor was higher when both these groups were combined and this difference was also statistically significant with a P value of 0.0145 (CI: 1.094-2.349).
In our study from patients admitted to the facility, we found that patients with AP had significantly higher incidence of NAFLD compared to patients without AP. We also noticed higher incidence of NAFLD with gallstones pancreatitis as compared to patients without AP. Our study therefore suggests that NAFLD can be a potential risk factor for development of AP.
NAFLD is a well-recognized objective marker of visceral obesity [4-6] Obesity is associated with increased incidence and even worsened severity on AP. A pooled data of 3 studies involving 1029 patients showed that relative risk of developing AP in individuals with a waist circumference >105 cm as compared to individuals with waist circumference <75 cm was 2.37 (95% CI 1.50-3.74). Similarly a meta-analysis of 11 prospective studies with pooled population of 8702 individuals showed a pooled relative risk (RR) of 1.43 (95% CI 1.09-1.87, p value<0.01) for developing AP in individuals with BMI>25 as compared to individuals with normal BMI [7]. AP is a cytokine-mediated disease. Many, if not all, systemic complications of AP are attributed to the pro-inflammatory cytokines. Higher serum cytokines like interleukin 6, monocyte chemo attractant protein -1 and adipokines like resistin and visfatin are noted in patients with severe AP. Visceral obesity leads to acute pancreatitis by pro-inflammatory cytokines release [8-10].
In the study we noted higher incidence NAFLD in patients who had pancreatitis compared to patients who did not have AP (OR: 1.596, CI: 1.094 – 2.349, P-value 0.0145). NAFLD with increased obesity leads to higher levels of these cytokines, which may in tern explain the increased incidence of NAFLD in patients with pancreatitis in our study [11].
On further subgroup analysis we noted higher incidence of NAFLD in patients with gallstone pancreatitis (OR: 1.688, CI: 1.070 – 2.701, P-value 0.0235), but not in patients with pancreatitis due to other causes when compared to similar subgroups without pancreatitis.
Association between gallstones and NAFLD was suspected based on shared pathogenic factors such as Obesity, Insulin resistance as well as diabetes type 2. On both conditions were quite common among patients with known metabolic risk factors (41% had NAFLD, 34% had gallstone disease). But several studies aimed to prove association between gallstones and NAFLD have shown contradictory results [12-15].
NAFLD patients have decreased level of foresaid X receptor and its mRNA in liver tissue, which has an important role in regulating the transcription of ATP-binding cassette transporters on the hepatocyte canalicular membrane resulting in the decreased activity of bile salt export pump (BSEP; ABCB11) and multidrug resistant glycoprotein (MDR3, ABCB4). This may lead to reduction in the biliary concentration of bile acids and phospholipids, thereby reducing the solubility of cholesterol [12,16,17].
Though NAFLD has higher incidence in patients with gallstone pancreatitis, this study cannot definitively answer if NAFLD causes pancreatitis due to gallstone formation or can it cause AP without gallstones.
While there was a higher incidence of NAFLD in patients with pancreatitis of unclear etiology, it was not statistically significant (OR: 1.400, CI: 0.688 – 2.919, P-value 0.4047). The fact that difference could not be detected may be related to the sample size.
NAFLD was identified in the study with AUS. AUS is a commonly employed imaging modality that is available widespread, cheap and avoids radiation. The sensitivity and specificity of AUS in finding hepatic fatty infiltrate is 93% and 77% respectively. The presence or absence of fatty liver was based solely on a radiologist’s interpretation of the ultrasound without any grading system. Secondary causes of fatty liver were not individually randomized due to small number of sample size.
The study is retrospective in nature, therefore cannot establish causality between the conditions. Further prospective studies should be done to demonstrate NAFLD as an independent risk factor for acute pancreatitis. We have randomized the groups with regards to age, sex, race as well as BMI to avoid confounding factors, though bias due to unidentified confounding factors cannot be completely ruled out due to limited cases of non-gallstone pancreatitis due to sample size.
This study shows that NAFLD can be an independent risk factor for development of AP. It is also possible that NAFLD may have pathophysiologic interplay with formation of gallstones, which is a known risk factor for AP.