Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Mini Review - (2023)Volume 12, Issue 1
This mini-review discusses the value of Proton Magnetic Resonance Spectroscopy (1H-MRS) and Diffusion-Weighed Imaging (DWI) in prediction of Testicular Sperm Extraction (TESE) outcome and testicular histopathology in men with Non-Obstructive Azoospermia (NOA). Intra-testicular signal levels such as Choline (Cho), Lipids, Creatine (Cr), Myo-Inositol (MI) as well as diffusion parameters mainly the apparent diffusion coefficient (ADC) will be compared against the previously mentioned outcome measures. The review will cover the points of strength, weakness and opportunities in this field. It will propose recommendations in order to enhance the current practice and refine the evidence.
1H-MRS; DWI; Testicular signals; ADC; Sperm retrieval; NOA
Testicular Sperm Extraction (TESE) is the corner stone in the management of men with Non-Obstructive Azoospermia (NOA) [1-4]. A meta-regression analysis on sperm recovery and Intra-cytoplasmic Sperm Injection (ICSI) outcomes in men with NOA showed that Surgical Sperm Retrieval (SSR) per cycle was independent of age and hormonal parameters at enrolment. However, the SSR increased as a function of testis volume [5]. Majzoub and colleagues in their recent meta-analysis, on NOA men with chromosomal abnormalities, reported favorable microdissection TESE (m-TESE) outcome in younger men and those with higher testosterone levels. They also reported better Testicular Sperm Aspiration (TESA) in men with Lower Luteinizing Hormone (LH) and Follicular Stimulating Hormone (FSH) values. No parameter predicted SSR rates in patients with Y-chromosome AZFc micro-deletions [6]. Therefore, predicting SSR is big challenges that face the anthologists whenever they confront a case with NOA.
TESE is an invasive intervention and dissection of the parenchyma may lead to testicular damage and hypogonadism [7-9]. Moreover, TESE is often scheduled with egg collection and ICSI. Consequently, unsuccessful SSR causes major inconveniences for the couple [5,10].
MR Spectroscopy and diffusion weighted imaging in men with azoospermia
Recently, Proton Magnetic Resonance Spectroscopy (1H-MRS) and Diffusion-Weighed Imaging (DWI) have been investigated as non-invasive imaging modalities that help differentiating Obstructive Azoospermia (OA) from NOA, predicting testicular pathology as well as SSR in men with NOA [11]. 1H-MRS is a non-invasive method for assessing brain function and metabolism. H-MRS can measure low-molecular-weight metabolites in the living brain and display their spectra without the use of a tracer. Diffusion Weighted Imaging (DWI) is a signal contrast generation technique that generates signal contrast by utilizing differences in Brownian motion. DWI is a technique for evaluating the molecular function and microstructure of the human body. Proton Magnetic Resonance Spectroscopy (1H-MRS) is a non-invasive technique used to assess brain function and metabolism. 1H-MRS can detect low-molecular-weight metabolites in the living brain and display their spectra without the use of a tracer. We introduce 1H-MRS and MRS for imaging metabolite distribution in this paper. The use of 1H-MRS imaging for a variety of neurological disorders will be discussed. Key articles describing the use of MRI in this field are illustrated in Table 1.
| Study/Country | Population/Numbers | Testicular signals | Outcome measure(s) | Major findings | Details |
|---|---|---|---|---|---|
| Hesham, et al. (Egypt) | 120 (60 OA and 60 NOA) | N- ADC, Lipids Cho, Cr | TESE outcome,Testicular pathology | N-ADC and proton MRS are helpful in differentiating OA from NOA and predicting SR and pathological abnormality | -N-ADC is significantly higher in NOA as compared to OA |
| -Testicular Cho and lipids are significantly higher in OA | |||||
| Cho level at a cut-off 0.195 predicts +ve m-TESE | |||||
| N-ADC was significantly lower in +ve m-TESE | |||||
| The following variables could predict testicular pathology (Testicular volume, N-ADC, and Lipids) | |||||
| Karakus and Ozyurt (Turkey) | 10 NOA,10 fertile men | Lipids, Cho, Cr,Lactate | TESE outcome | Detection of high Cho metabolite in the spectra before TESE in NOA men increases SR rates in m-TESE. | SRR is 50%. |
| Cho and Creatine signals were found to be significantly lower in NOA cases where no sperm could be found in m-TESE. | |||||
| Cho and Cr signal intensities in TESE +ve were significantly higher than those with TESE –ve | |||||
| Cut-off value of Cho was 1.24 ppm (AUC 0.665, p=0.01 {95% CI: 0.722–1.00}) | |||||
| Cut-off value of Cr was 1.18 ppm (AUC 0.887, p=0.02 {95% CI}): 0.620–1.00) for +ve TESE | |||||
| Tsili, et al. (Greece) | 41 NOA, 17 fertile men | V-ADC | TESE outcome, Testicular pathology | Testicular V-ADC histogram parameters may identify subpopulation of NOA with a specific type of maturation arrest | The median ADC proved the most significant metric (p=0.007) to predict the presence of sperm. |
| Tsili, et al. (Greece) | 48 NOA,18 fertile men | N-ADC, Cho, Lipids, MI, MTR | Etiology of NOA, 1, idiopathic; 2, genetic; 3, non-genetic causes | MRI may provide useful, noninvasive information on the microstructural and biochemical milieu of NOA testes | MRS testis signals are helpful in discriminating NOA etiology. |
| Regression analysis failed to identify the most discriminating MR imaging feature for NOA etiology | |||||
| Çelik ,et al. (Turkey) | 9 NOA, 5 fertile men | Cho, Cr, MI, lactate& lipids | TESE outcome | MRS is a Non-invasive screening method to predict the successful SR of m-TESE. | A high Cho peak was detected in 87% of the NOA men with +ve TESE. NOA men without sperm at the previous m-TESE showed a marked ↓ in Cho and Cr signals. |
| For +ve sperm retrieval in m-TESE, the cut-off value of Cho is 1.46 ppm, the cut-off value of Cr is 1.43 ppm, and the cut-off value of MI is 0.79 ppm. | |||||
| Ntorkou, et al. (Greece) | 49 NOA, 50 fertile controls | Cho, TLM, MI, Glutamate | TESE outcome,Testicular pathology | MRS Provides metabolic information about the testis in NOA patients and assesses spermatogenic status before m-TESE | ALL signals were significantly reduced in NOA compared to fertile men, ↑ normalized concentrations of glutamate were observed in NOA with –ve TESE |
| Ntorkou ,et al. (Greece) | 49 NOA, 45 fertile controls | Testicular volume (TV), N-ADC, and MTR | TESE outcome, Testicular pathology | TV, ADC, and MTR predict SR in men with NOA | A positive correlation between higher JS and TV (p<0.001) and a negative correlation between JS score and both ADC (p=0.015) and MTR (p=0.003). |
| TV is reduced in men with –ve TESE. | |||||
| ADC (p=0.011) and MTR (p=0.045) were `significantly ↑ in NOA testes with –ve TESE. | |||||
| Tsili, et al. (Greece) | 21 NOA, 21 fertile controls | N-ADC, FA | TESE outcome, Testicular pathology | Both ADC and FA are ↑ in NOA testes compared to fertile men; N-ADC is proven to be a more useful diagnostic tool in the identifying focal spermatogenesis. | DTI/FA DTI parameters were not predictive of sperm retrieval after TESE. |
| Higher values of FA were found both in NOA testes with JS ≥ 8 and JS<8. | |||||
Abbreviation: Cho: Choline; Cr: Creatine; DTI: Diffusion tensor imaging; FA: Fractional Anisotropy; JS: Johnsen Score; MTR: Magnetization Transfer Ratio; m-TESE: Microsurgical Testicular Sperm Extraction; MRS: MRI Spectroscopy; MI: Myo-Inositol; NOA: Non Obstructive Azoospermia; N-ADC: Normalized-Apparent diffusion coefficient; OA: Obstructive Azoospermia; SR: Sperm Retrieval; TV: Testicular Volume; TLM: Total Lipids and Macromolecules; V-ADC: Volumetric ADC.
Table 1: Studies evaluating MR spectroscopy and diffusion weighted imaging in men with azoospermia and relation to TESE outcome and testicular histopathology.
The evidence so far highlights the value of MRI in prediction of TESE outcome and identifying testicular pathology in men with NOA [12-18]. However, MRI comes with a substantial risk; not only for the patient, but also for health care team and any other personnel who may come in proximity to the magnetic fields in or around the scanner [19-21]. Ultrasonography, on the other hand, seems to be an alternative safe and cheaper solution [22] measured the testicular volume and the diameter of the head of the epididymis (caput diameter) in men with NOA before TESE. They reported that the caput diameter did not show any difference between NOA men with or without successful TESE. However, men with unsuccessful TESE had significantly lower testicular volume (P=0.0037). The caput diameter did not correlate with the number of retrieved sperm cells, the serum FSH level, or with the percentage of tubules with elongated spermatids at testicular histopathology. Although, the same investigators demonstrated the value of ultrasonography in predicting genital duct obstruction [23]. Its value in diagnosing OA has been confirmed by other investigators [24-26].
Herwig and colleagues reported that high perfusion areas detected by Doppler blood flow examination is associated with higher sperm recovery during TESE [27]. In 2019, Xue and colleagues assessed 70 men with azoospermia (46 NOA and 24 OA) with contrast-enhanced US (CEUS) 10 days prior to TESA. The authors reported that CEUS guided TESA with cognitive fusion did not yield higher sperm retrieval rate in men with NOA probably due to imprecise correlation between the biopsy sites and the target perfusion areas as detected by CEUS [28]. Although, the same technique has been proved to be effective in guiding the surgeon to the best retrieval site in 187 testicles examined. The Sperm Retrieval Rates (SRRs) in the best perfusion area, poorest perfusion area (over the maximal longitudinal section) and conventional area were 63.1, 34.7 and 47.1%, respectively; P<0.05 [28-29]. Therefore, MRI, despite the safety concerns, is considered one of the best diagnostic imaging modalities in predicting TESE outcome and testicular pathology.
Testicular signals such as Choline (Cho), lipids, Myo-Inositol (MI), and Normalized-Apparent Diffusion Coefficient (N-ADC) play undeniable role in predicting successful sperm retrieval [11,12,15,16]. However, the value of creatine in differentiating OA from NOA and in predicting TESE outcome is questionable in a recent study [11] conducted on men with OA rather than fertile controls.
Aaronson and co-workers reported higher Cho levels in men with normal spermatogenesis compared to patients with spermatogenic arrest. Therefore, 1H-MRS could identify the testicles containing spermatids or spermatozoa [30-31] on the other hand, found 1H-MRS to be reliable and sensitive in discriminating infertile or (azoospermic testes) from fertile testicles. It shows alteration in the seminiferous tubules, especially when semen samples cannot be collected [32]. Changes in the levels of metabolites, mainly Cho, reflect testicular parenchymal alterations [32].
Tsili and colleagues [14] were the only investigators exploring the value of 1H-MRS in identifying the etiology of azoospermia in men with gonadal failure. They classified their patients according to the cause such as idiopathic (n=22); genetic (n=5) and acquired causes (n=21). However, genetic cause group included limited number of men with Klinefelter's syndrome (47, XXY) [14].
In practice, diagnosis of genital duct obstruction could be challenging in a significant number of patients. The MRI seems to be beneficial in this context. Hesham and colleagues [11], in their recent work demonstrated that MRI predicted normal spermatogenesis in 95% of men with OA as the pathology has been accurately predicted in 114/120 of the testes [11] although, it was not 100% predictive. On snap frozen testicular tissue from 27 men, quantitative high resolution magic angle spinning spectroscopy was performed on three classic histological patterns: normal spermatogenesis (men with prior paternity undergoing vasectomy reversal), maturation arrest (early or late, MA), and Sertoli-cell only From each biopsy specimen, concentrations of 19 tissue metabolites were determined. The three histologic groups' metabolite concentrations were compared using a one-way ANOVA analysis.
Despite the preliminary evidence regarding the value of MR spectroscopy and testicular signals in predicting TESE outcome and testicular pathology, there are several limitations that should be considered before wide spread use of this strategy in the clinical practice. The treatment of patients with non-obstructive azoospermia (testicular sperm extraction combined with intracytoplasmic sperm injection).
Sperm retrieval is successful in up to 50% of men with NOA; however, no one clinical finding or research can accurately predict a favorable outcome.
Many studies have indicated that testicular biopsy is the strongest predictor of a successful TESE. The current study reveals that tubules with mature spermatozoa in the histopathological specimen are the best predictor of TESE success, regardless of the overall condition of spermatogenesis.
The data imply that a lower limit threshold value of 2% of tubules with spermatogenesis in the histopathology specimen will result in positive sperm retrieval. Nevertheless, doing a diagnostic biopsy prior to TESE is not practicable since it would require patients to undergo two procedures, increasing the cost and difficulties.
Before beginning the ICSI cycle, a diagnostic biopsy should be combined with an initial TESE. If extra sperm is required on the day of ovum pick-up and ICSI, patients may be offered a repeat TESE based on the findings of the histology specimen.
In addition, if the initial TESE was negative, the biopsy result will aid in the choice to perform a repeat TESE.
This regimen is less expensive because the ICSI cycle will only begin if sufficient sperm is obtained. The limitations are listed below.
• The majority of studies are single-center.
• All the published studies show limited numbers of participants (range between 14 to 120).
• There is no clear indication based on the etiology of NOA, with special emphasis on the genetic causes.
• Lack of economic evaluation studies (Incremental cost/Incremental benefits).• Lack of studies demonstrating the impact of inter-observer variations.
• Some articles based their SSR on conventional TESE or used inferior methods in optical magnification.
Although, Safety Issues to health care professionals and some hazards may occur to the patients e.g., men with pacemakers. New opportunities in this field are open for future research including, but not limited to, new multi-center studies with larger number of participants, correlating the MRI value against different causes of NOA with special emphasis on genetic causes. Finally, economic evaluation studies (Incremental cost/Incremental benefits) are needed to validate the yield and the true value of the MRI in this group of patients. SWOT analysis is shown in Figure 1.
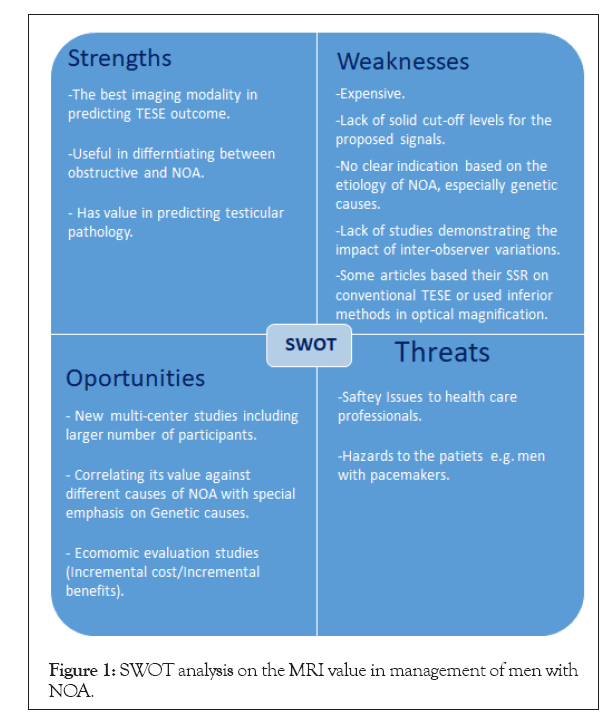
Figure 1: SWOT analysis on the MRI value in management of men with NOA.
Testicular metabolite signal levels and apparent diffusion coefficient values could play a vital role in prediction of TESE outcome and identifying testicular histopathology in men with non-obstructive azoospermia. However, the associated safety concerns and the unclear cost effectiveness of these modalities need to be addressed. Large multicenter studies are required to explore the yield of this approach. Based on the funding model of a healthcare system, economic evaluation studies are needed to explore the cost effectiveness and cost utility of this tool.
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
Citation: Ragab A, Zohdy W (2023) New Dimensions in Predicting Sperm Retrieval in Men with Non-Obstructive Azoospermia: A Mini-Review on MR Spectroscopy and Diffusion Imaging. Andrology.12:279
Received: 14-Feb-2023, Manuscript No. ANO-23-21799; Editor assigned: 17-Feb-2023, Pre QC No. ANO-23-21799 (PQ); Reviewed: 03-Mar-2023, QC No. QC No. ANO-23-21799; ; Revised: 09-Mar-2023, Manuscript No. ANO-23-21799 (R); Published: 20-Mar-2023 , DOI: 10.35248/2167-0250.23.12.279
Copyright: © 2023 Ragab A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.