Clinical & Experimental Cardiology
Open Access
ISSN: 2155-9880
ISSN: 2155-9880
Case Report - (2022)Volume 13, Issue 6
Background: Myocardial Bridging (MB) is a congenital coronary artery malformation. Various clinical symptoms related to MB have been reported; however, subxiphoid pain has rarely been reported. Moreover, it is rarer for Electrocardiography (ECG) to show such obvious ischemia in patients with MB.
Case presentation: We report a 36-year-old male who presented with subxiphoid pain. ECG showed ST segment depression and T-wave inversion with symmetry in leads V2 to V6. Emergency Coronary Angiography (CAG) confirmed that it was caused by MB.
Results: CAG showed MB of the Left Anterior Descending (LAD) artery with a 1.5 cm intramural segment and that the vascular lumen was compressed 80% during systole. At the same time, gastroscopy showed peripyloric and antral ulcers. The patient received Calcium Channel Blockers (CCBs) and drug treatment for peptic ulcers, and then the symptoms disappeared.
Conclusion: ECG showed obvious myocardial ischemia. MB may have been one of the reasons for ischemia. When the heart contracts, the myocardial bridge compress the mural coronary artery and further narrows its lumen. The longer and thicker the myocardial bridge is, the greater the angle between the myocardial fibers and blood vessels the more severe the mural coronary artery stenosis is, the more severe the distal myocardial ischemia.
Coronary artery malformation; Myocardial bridge; Coronary artery disease; Coronary angiography
The authors declare that they do not have any conflicts of interest.
We thank AJE (www.aje.cn) for its linguistic assistance during the preparation of this manuscript.
Conceptualization: Mei-lian Cai, Data curation: Mei-lian Cai Investigation: Mei-lian Cai, Resources: Mei-lian Cai Supervision: Wei Zhang, Writing- original draft: Mei-lian Cai Writing-review and editing: Mei-lian Cai
Some or all codes generated or used during the study are available in a repository or online (provide full citations that include URLs or DOI).
Some or all data and material generated or used during the study are available in a repository or online (provide full citations that include URLs or DOI).
The work has been approved by all the authors for publication.
The work was approved by all the authors for participation.
Written informed consent was obtained from the patient.
MB: Myocardial Bridging; ECG: Electrocardiogram; CAG: Coronary Angiography; LAD: Left Anterior Descending; CCB: Calcium Channel Blocker; CHD: Coronary Heart Disease, ACS: Acute Coronary Syndrome; LCX: Left Circumflex Artery; IVUS: Intravascular Ultrasound; HCM: Hypertrophic Cardiomyopathy; CCTA: Coronary Computed Tomography Angiography; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; CABG: Coronary Artery Bypass Grafting; PCI: Percutaneous Trans luminal Coronary Intervention.
Funding information is not applicable.
The patient refused IVUS and FFR evaluations, so we could not better evaluate his myocardial ischemia. The most important limitation of this study is its lack of long-term follow-up, and the subsequent inability to assess the patient's prognosis.
Two months after discharge, a repeat gastroscopy showed that the peripyloric and antral ulcers were cured. At the 11-month outpatient follow-up, the patient stated that he was taking his medicine regularly and paying attention to his diet, and he had no further attacks of subxiphoid pain.
Surgery is an effective treatment for symptomatic MB patients for whom drug treatment is ineffective, and these surgical techniques include Coronary Artery Bypass Grafting (CABG) and surgical unroofing. CABG is more suitable for patients with deep (>5 mm) or long (>25 mm) myocardial bridges. There is a risk of ventricular wall perforation after myocardial bridge resection, but Hemmati, et al. confirmed that surgical unroofing is a safe option for patients with isolated MB. In this case, in addition to the myocardial ischemia caused by MB, subxiphoid pain was also related to gastrointestinal ulcers.
The patient suffered from subxiphoid pain with connection to daily activities, and ECG showed evident myocardial ischemia. At the same time, CAG showed that there was MB of the Left Anterior Descending (LAD) artery. Therefore, he was diagnosed with myocardial bridge syndrome. Myocardial bridge syndrome occurs when a MB overlies the coronary artery and causes myocardial ischemia changes in ECG. The features of myocardial bridge syndrome include: (1) ECG shows multi lead ST segments depression, T-wave inversions or even obvious inversions. (2) Patient has a history of angina or syncope. (3) CAG shows a normal coronary artery, but myocardial bridge is found over the coronary artery, and (4) a normal ST-T is shown after the myocardial bridge is removed. In addition, similar ECG changes were seen for ACS and Hypertrophic Cardiomyopathy (HCM). Echocardiography showed normal results, which excluded HCM.
MB is a congenital coronary artery malformation that was discovered 100 years ago. It was first reported by Cranicianu [1], myocardial bridging is a common finding (5%-86%) depending on the imaging modality/autopsy series [2]. The detection rate of coronary angiography (CAG) is 2%-6%, that of Coronary Computed Tomography Angiography (CCTA) is 19%-22%, and that of autopsy is 33%-42%. The CCTA data are closer to the autopsy data. Therefore, CCTA is more sensitive than CAG and intravascular imaging and can be used for general diagnosis [3]. The middle segment of the left anterior descending coronary artery is the most frequent location of MB; however, bridging on the circumflex branch of the left coronary artery and right coronary arteries has also been reported [4]. Cai, et al. found that a case of MB was located in the second right ventricular branch of the right coronary artery [5].
The current methods to diagnose myocardial bridges include CAG, CCTA, IVUS, and cardiac Magnetic Resonance Imaging (MRI). CAG shows compression of the artery caused by the MB with narrowing of the lumen and diastolic relaxation. CAG clearly shows signs of coronary artery ischemia compressed by myocardial bridges during systole, while the coronary artery compression is relieved during diastole. The hemodynamics of a bridging segment may be assessed with the mean FFR measurement. Compared with conventional coronary angiography, Computed Tomography (CT) enables direct visualization of coronary arteries, including the surrounding tissue, and thus allows for the depiction of tunneled segments even when there is only minimal or no systolic compression and no change in the vessel course [6]. The depiction rate of MB is greater with 64-section CT coronary angiography than with conventional coronary angiography. The degree of systolic compression of MB significantly correlates with the tunneled segment depth but not the length [6]. MRI shows the relationship between the mural coronary artery and MB and judges whether the coronary artery blood supply function at the MB is abnormal through the functional imaging of the MB.
MB usually has a benign prognosis; however, it can lead to dangerous complications, including ischemia and acute coronary syndromes, coronary spasm, ventricular septal rupture, arrhythmias, coronary thrombosis, ventricular dysfunction and sudden death [7]. Young reported a rare case of MB presenting as myocardial ischemia-induced cardiac arrest, and he highlighted MB as one of the important causes of sudden cardiac death. They considered vasospasm, which was confirmed by a transient ST elevation on ECG, to be a trigger factor. The patient survived; in addition, some patients also have vascular endothelial dysfunction and micro-vascular disease complications, resulting in myocardial ischemia [8]. In addition, some patients also have vascular endothelial dysfunction and microvascular disease complications, resulting in myocardial ischaemia. Some studies have shown a prevalence of MB of 28%-50% in HC patients [9-12]. MB has been linked to sudden death, and patients with combined HCM and MB have a worse prognosis [12].
The direction of myocardial fibers of the myocardial bridge is at a nearly at a right angle to the long axis of the vessel at the anterior and posterior descending branches, while it is at a smaller angle at the anterior right ventricular branch and the anterior left ventricular branch. In the cross section of the mural coronary artery, the lumen is small, and the wall is thin, which is more obvious when the muscle bridge is thick. The mural coronary artery segment does not easily form atherosclerosis, and atherosclerosis is often seen in the intima of its proximal and distal vessels. Due to the above anatomical characteristics, when the heart contract, the myocardial bridge compresses the mural coronary artery and further narrows its lumen. The longer and thicker the myocardial bridge is, the greater the angle between the myocardial fibers and blood vessels the more severe the mural coronary artery stenosis is, the more severe the distal myocardial ischemia, and the development of myocardial infarction becomes more likely. The degree of systolic compression of MB significantly correlates with the tunneled segment depth but not the length [6]. Systolic vessel compression has been shown to persist into mid-to-late diastole [13].
Sternheim, et al. pointed out that for patients without clinical symptoms, treatment should focus on risk factor correction, including the appropriate treatment of concomitant coronary artery disease and the mitigation of potential inducements. The predisposing factors include coronary artery spasm, smoking and use of excitatory substances (cocaine), physiological stress and an insufficient functional exercise reserve [3]. It is estimated that the predisposing factors of the patient are smoking and coronary artery spas. MB can accelerate the progression of atherosclerotic plaque, so it is very important to control atherosclerotic plaque.
Medical management with negative inotropic and negative chronotropic agents is considered first-line therapy [14]. β Receptor blockers can slow down the heart rate, increase the diastolic filling time and reduce the arterial pressure in the tunnel section. Calcium Channel Blockers (CCBs) are also commonly used to treat symptomatic myocardial bridges, especially for patients with myocardial infarction. CCBs are preferred in patients with receptor blocker contraindications (such as bronchospasm). In addition, CCBs cause vasodilation and may be beneficial to patients with vasospasm. If the ischemia of myocardial bridge patients cannot be alleviated by drugs, Percutaneous Transluminal Coronary Intervention (PCI) is not impossible, but there are some disputes. Because the radial pressure of the myocardial bridge on the stent is significantly greater than that of atherosclerosis, there is a high risk of coronary perforation (up to 6.3% in the study), stent rupture (reported in individual cases), in-stent restenosis (75% in BMS and 25% in DES) and in-stent thrombosis (reported in individual cases). After strict screening of patients, PCI could be considered in patients who had poor drug treatment effects, a short life expectancy or surgical contraindications [15]. In short, MB can be stented [16-18].
A 36-year-old male presented with subxiphoid pain for 3 days that was aggravated for 13 hours on July 3, 2021. Three days prior, the patient suffered from subxiphoid pain that was related to his daily activities and the pain was a paroxysmal distending pain that was located in the lower 2 transverse fingers of the subxiphoid area and lasted from a couple of seconds to 5 minutes with no connection to eating. The symptoms were relieved after rest, and they were not accompanied by palpitations, shortness of breath, dizziness, acid regurgitation, belching or haemoptysis. He did not receive treatment in the previous three days. The symptoms worsened 13 hours prior. The patient went to the emergency department for treatment. He underwent electrocardiographic examination. The electrocardiography results showed the following: sinus rhythm left ventricular high voltage, ST segments with significant depressions on the V2 to V6 leads, and T-wave inversions with symmetry (Figures 1A and 1B).
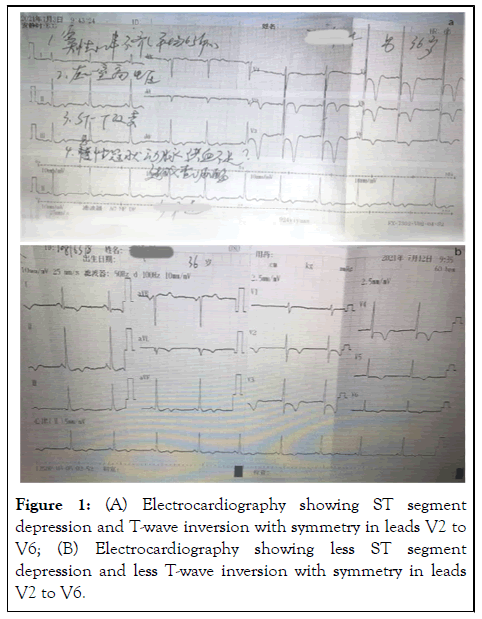
Figure 1: (A) Electrocardiography showing ST segment depression and T-wave inversion with symmetry in leads V2 to V6; (B) Electrocardiography showing less ST segment depression and less T-wave inversion with symmetry in leads V2 to V6.
Preliminary diagnosis
Coronary Heart Disease (CHD) or Acute Coronary Syndrome (ACS)? He was transferred immediately from the emergency department to our department for Emergency Coronary Angiography (CAG). He had smoked one pack a day for 10 years. He denied the use of any alcohol and did not have other known chronic diseases. There were no similar diseases or any other genetic history of disease in his family.
The patient’s vital signs were normal upon admission. On physical examination, the patient’s body temperature was 36.5°C, pulse rate was 59 beats/min, respiratory rate was 20 breaths/min, blood pressure was 113/73 mmHg, weight was 66 kg, and height was 1.70 meters. The patient had a clear mind, clinostatism, and no cyanosis of the lips. The abdomen was flat and soft, with slight tenderness in the subxiphoid, without rebound pain and the bowel sounds were normal. No other unusual findings were present on his physical examination.
Admission diagnosis
The causes of chest pain that needed to be investigated were as follows: CHD, Acute Coronary Syndrome (ACS) and gastritis. Emergency CAG showed that there was MB of the Left Anterior Descending (LAD) artery with a 1.5 cm intramural segment, the vascular lumen was compressed 80% during systole, and there was a TIMI glow of grade 3 (Figures 2A and 2B). No plaques were observed, occlusion was observed in the Left Circumflex Artery (LCX), and the retention of contrast medium was observed. No plaques were observed in the right coronary artery and the bloodstream was unobstructed. The patient refused Intravascular Ultrasound (IVUS) and Fractional Flow Reserve (FFR) evaluation. Auxiliary examination results from the emergency department showed no detectable changes in the abdominal color ultrasound, standing abdominal plain film, myocardial enzymes, myoglobin, serum troponin T, routine blood tests, coagulation function, liver and kidney function, serum glucose, or electrolytes. After CAG, re-examination of myocardial enzyme and serum troponin T were normal. The Electrocardiogram (ECG) showed no change from before. No abnormalities were found in thyroid function, glycosylated haemoglobin, or echocardiography. Gastroscopy showed peripyloric and antral ulcers, and antral biopsy showed moderate chronic nonatrophic gastritis with erosion. The carbon 14 exhale test was negative.
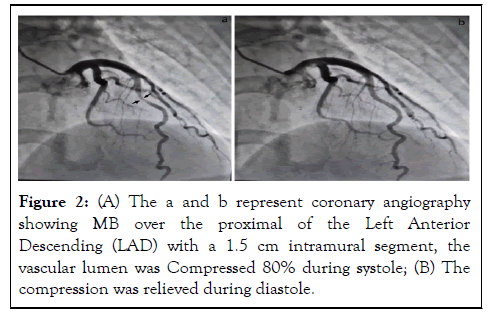
Figure 2: (A) The a and b represent coronary angiography showing MB over the proximal of the Left Anterior Descending (LAD) with a 1.5 cm intramural segment, the vascular lumen was Compressed 80% during systole; (B) The compression was relieved during diastole.
Definite diagnosis
Myocardial bridge syndrome (the proximal of the left anterior descending), Peripyloric and antral ulcers. During his hospitalization, he asked the Gastroenterology Department and cardiothoracic surgery for consultation. The patient was treated with dirthiazem (90 mg, qd), indobufen (100 mg, bid), atorvastatin (20 mg, qn), pantoprazole (20 mg, q12 h), rebaperate (100 mg, tid), and Kangfuxin (10ml, tid). He was advised to quit smoking. He refused to undergo surgical unroofing. After 7 days, the patient’s subxiphoid pain disappeared. Re-examination of the ECG indicated sinus rhythm, left ventricular high voltage, less ST segments with significant depressions on leads V2 to V6, and less T-wave inversions with symmetry (Figure 1B). The patient improved and was discharged on July 14, 2021.
ECG shows multi lead ST segments depression, T-wave obvious inversions, which are often misdiagnosed as Acute Coronary Syndrome (ACS) before examination of coronary Computed Tomography Angiography (CCTA) or Coronary Angiography (CAG). In addition, similar ECG changes are seen for Myocardial Bridging (MB), Single Coronary Artery (SCA) and Hypertrophic Cardiomyopathy (HCM). This is a rare case report of the patient who was diagnosed as myocardial bridge syndrome with ECG showing obvious myocardial ischemia and CAG showing MB over the proximal of the Left Anterior Descending (LAD) compressed 80% during systole. MB can lead to sudden death, so early intervention is crucial, however, it is difficult to find asymptomatic MB patients at present. It is believed that we can create a simpler means of diagnosing MB in the future.
Citation: Cai ML, Zhang W (2022) Myocardial Bridge Syndrome: A Case Report and Literature Review. J Clin Exp Cardiolog. 13.731.
Received: 20-Jun-2022, Manuscript No. JCEC-22-17995; Editor assigned: 23-Jun-2022, Pre QC No. JCEC-22-17995(PQ); Reviewed: 11-Jul-2022, QC No. JCEC-22-17995; Revised: 18-Jul-2022, Manuscript No. JCEC-22-17995(R); Published: 25-Jul-2022 , DOI: 10.35248/2155-9880.22.13.731
Copyright: © 2022 Cai ML, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.