Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Review - (2020)Volume 10, Issue 2
Myalgia, also known as muscle pain, is a common issue in the population and frequent cause of medical appointment, especially in adults. It should be noted that myalgia is different from myopathy or myositis, these being muscle disease and muscle inflammation, respectively. On the other hand, Polyarthralgia is defined as joint pain in more than 4 joints and it is commonly confused with polyarthritis, but the latter is defined as joint disease where more than 5 joints are involved, accompanied by polyarthralgia and joint inflammation.
In the clinical practice, a confusion arises when it comes to approach the signs and symptoms of these pathologies, making it similar with other diseases. In addition to that, under a clinical view, doubts may arise when making an approach, management and treatment.
The purpose of this study is to clarify and expose the approach of myalgias and polyarthralgias syndrome for family practice, general practitioners, internist, orthopedists and rheumatologists.
Myalgias; Polyarthralgias; Myopathies; Joint pains; Arthritis
Myalgia, also known as muscle pain, is a common issue in the population and frequent cause of medical appointment, especially in adults. Following that, in the course of their life almost everyone will experience any type of muscle sorrow. This disease affects one or more muscles; it may also involve ligaments, tendons, fascia, bones and organs. The most common causes for myalgia are over effort, trauma and viral infections. Even though most of these are benign and self-limited, myalgia could be the trigger of disorders associated with morbidity. It should be noted that myalgia is different from myopathy or myositis, these being muscle disease and muscle inflammation, respectively [1,2].
The patient's history and a complete physical examination is the key to narrow the causes of the myalgia to a few manageable. When the myalgia is severe and persistent with unknown cause, it is necessary selected testing to identify the diagnosis and be able to direct the treatment. Meanwhile, it's very important to identify and classify the diffuse from localized symptoms.
Up to 60%-85% of the population has or had nonspecific back pain of muscular origin at some time in their life. Muscle disorders are the first cause of chronic pain in Spain, with a significance impact in the person's social and work environment. People 50 years or younger present with muscle pain due to repetitive work or sports activities; and muscular injuries are most frequent in professional sports and they could be up to 30% of all lesions. The prevalence of chronic musculoskeletal pain in the population is estimated to be between 10-15%. Another study showed that musculoskeletal pain is the most common reason for a person to visit a doctor [2,3].
“Pain evoked by myofascial trigger points has a point prevalence of approximately 30%” [3]. Studies have shown that fibromyalgia has a prevalence up to 1-5% of the population and the relation women-men is 8:1 between the ages of 30-60 years old; also “7% of all women aged 70-80 years suffer from the fibromyalgia syndrome” [2,3].
“Muscle tends to be referred pain more often” [3]. Muscle pain is produced by the activation of nociceptors which are special for detecting stimuli that can be capable of damaging the tissue and be perceived as painful. There are free nerve endings that connect with the Central Nervous System through thinly myelinated fibers or unmyelinated fibers. This can be activated by a mechanical
stimulus like trauma or endogenous inflammatory mediators such as bradykinin, prostaglandin E2 and serotonin. The most important components to generate muscle pain are the use of ATP and protons; they attach to the receptor molecule in the membrane of the nerve ending so they activate nerve endings. Also, the nerve growth factor is related with muscle pain; because it activates muscle nociceptors and it´s concentration increases when a muscle is inflamed [3].
The doctor has to take into account the fact that some muscle pain has its origin in a bone, organ or central nervous system disease. But other possible triggers are drugs and alcohol.
Another cause of myalgia although there are little amount of studies about it, is the one caused by SARS-CoV-2 (COVID-19)
Myalgias are classified into different types according to their relationship to exercise
• Muscle pain during or immediately after exercise: usually involves specific muscles and begins during or just after the physical activity that causes it. Exercise intolerance is one of the most characteristic symptoms of late-onset metabolic myopathies, and may appear associated with progressive muscle weakness and myoglobinuria [2,4].
• Post-exercise muscle pain: it is a spasmodic, acute and involuntary pain that appears after 24-48 h after the end of the continuous muscular exercise, in healthy subjects, who practice long duration anaerobic and/or aerobic activities of great intensity; it is a product of inflammation and microtrauma. They are not a symptom of muscle disease, they usually affect people with lack of training and may associate elevated CK levels [2,5,6]. The main risk factor for myalgias is the practice of ineffective irregular muscle stretching.
• Muscle pain at rest: if there is no weakness, it is not usually associated with muscle disease [2].
The most common causes of myalgia are:
• Injuryor trauma.
• Overload.
• Tensionor stress.
Less frequently, myalgia can also be due to:
1. Non-muscular causes:
They generally produce myalgias not related to exercise.
a) Metabolic and endocrine disorders:
• Hypothyroidism.
• Hypoparathyroidism.
• Osteomalacia.
• Uremia.
• Liverfailure.
• Suprarrenal insufficiency.
• Magnesiumdeficiency.
• Seleniumdeficiency.
• Thiaminedeficiency.
• Hemodialysis.
b) Rheumatic diseases:
• Polymyalgiarheumatica.
• Fibromyalgia.
• Myofascialpain.
• Lupus.
• Mixedconnectivetissuedisease.
• Sjogren'ssyndrome.
• Rheumatoidarthritis.
• Benignhypermobilitysyndrome [2].
2. Muscular causes:
a) Inflammatorymyopathies:
• Autoimmuneoridiopathic.
• Infectious
b) Hereditarymyopathies:
• Metabolic.
• Congenital.
c) Toxicmyopathies.
In this review we will focus on this last group of causes of myalgia, the causes of muscle diseases that includes inflammatory myopathies, hereditary myopathies and toxic myopathies.
Inflammatory myopathies (MI) or myositis are a heterogeneous group of rare muscle diseases, characterized by inflammation of the different components of muscle tissue, either in isolation or more commonly in the context of a systemic condition [7]. We divide inflammatory myopathies for a more didactic term into those that have infectious and primary causes, autoimmune or idiopathic causes (Figure 1).
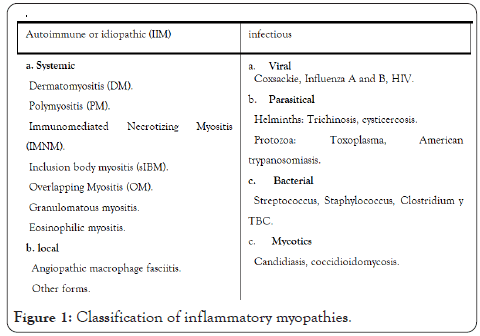
Figure 1 : Classification of inflammatory myopathies
Autoimmune or idiopathic myopathies
Autoimmune or idiopathic inflammatory myopathies are a group of diseases whose main characteristic is muscle weakness and the identification of an underlying inflammation in muscle biopsy [8].
They are classified on the basis of different clinical and pathological characteristics into four subtypes: dermatomyositis, polymyositis, immune-mediated necrotizing myositis, inclusion body myositis, and overlapping myositis [9].
Dermatomyositis: DM is undoubtedly the best uniformly recognized and best-defined entity within autoimmune inflammatory myopathies. It is observed in both children and adults and has a marked female predominance, particularly after 45 years. The frequency of myalgias and the sensitivity (generally mild) varies (25% to 50% of patients) [9,10].
The disease is usually slowly progressive (weeks to months) and its distinctive feature is skin involvement, being the first symptom, which manifests itself as a skin rash that can precede weakness, or present without it (amyopathic dermatomyositis). Patients show red-purple or purplish rashes in photosensitive areas, including periorbital heliotrope rash (blue-purple) with edema (Figure 2); erythematous rash on the face, knees, elbows, malleoli, V-shaped (V sign) at the base of the neck and chest and on the upper back and shoulders (shawl sign). Gottron's papules (Figure 3) occur symmetrically over the dorsal region of the metacarpophalangeal and interphalangeal joints [7,9,10].
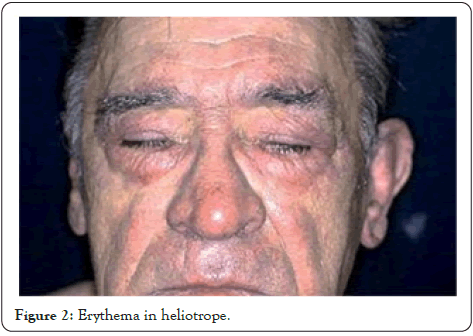
Figure 2 : Erythema in heliotrope.

Figure 3 : Gottron papules.
It is important to highlight that adult patients with DM and PM have a higher risk of malignancies compared to the general population, this risk is triple in patients with DM (13.8%) compared to those with PM (6.2%). The most common cancers are ovarian cancer, breast cancer, colon cancer, melanoma, nasopharyngeal cancer (in Asians), lung cancer, and non-Hodgkin lymphoma; The risk of these cancers requires a thorough annual study in the first 3 years after the onset of the disease [9,11].
Polymyositis
Polyomyosis (PM), initially defined by Bohan and Peter as evidence of symmetric proximal myositis and the absence of histopathological signs of other myopathies or complete absence of any other features (obviously including the skin and lung, but also joint, vascular manifestations and general). This definition has been constantly changing due to the rapid discovery of new autoantibodies making the definition of pure PM less and less valid [10]. Polymyositis is rare as a separate entity and is often misdiagnosed; most patients whose condition has been diagnosed as polymyositis have inclusion body myositis, immune-measured necrotizing myositis, or inflammatory dystrophy [9].
In the course of weeks or months, the patient develops proximal and symmetrical weakness of the extremities, although it can sometimes be asymmetric, which can be associated with fatigue and myalgia in up to 50% of cases. The facial muscles are not affected, and the distal muscles engage only in late stages. Rarely, the paravertebral and neck muscles are affected, which can produce, respectively, camptochoria and the sign of the fallen head [11].
Immune-mediated necrotizing myositis: Necrotizing autoimmune or autoimmune necrotizing myositis (IMNM) is a distinct clinicopathological entity that occurs more frequently than polymyositis, accounting for up to 19% of all inflammatory myopathies [9].
It can occur spontaneously, in isolation, or in the context of a viral infection, associated with cancer, in patients with autoimmune connective tissue diseases or exposed to statins, even after their intake is suspended (if the myopathy improves within 4 to 6 weeks after the discontinuation of the statins it was probably caused by the toxic effects of the drug rather than by immune myopathy) [7,9]. It can occur at any age, but is mainly seen in adults; its onset is acute or subacute, and is associated with muscle pain and very high levels of creatine kinase (CK). Exceptionally, the IMNM shows a slowly progressive, asymmetrical evolution, with skeletal deformities, winged scapula, and selective atrophy of some muscle groups, mimicking the pattern of muscular dystrophy, which should be excluded. Patients often report difficulty getting up from a chair, climbing the stairs, or raising the arms above the head [7,9,11]. Approximately 60% of patients with IMNM show high titers of anti-SRP or anti-HMGCR antibodies. It is interesting to note that, at least in theory, statins are the only drug capable of generating an autoimmune reaction against its own drug target [7]. Histology confirms the necrotizing nature of myopathy, showing no (or little) inflammation, but a diffuse appearance of necrosis/regeneration [12].
Overlapping myositis: This myositis subtype is the most recently established. Similar to what occurs with other autoimmune connective tissue diseases, overlapping myositis occurs when autoimmune inflammatory myopathy presents with extramuscular signs and symptoms such as those seen in systemic lupus erythematosus (SLE), scleroderma, or mixed connective tissue disease. Antisynthetase syndrome (ASS) is the most common form of overlay myositis (OM). It is a particularly severe form of MII defined by the presence of anti-synthetase antibodies (most commonly anti-Jo-1), associated interstitial lung disease (ILD), Reynaud's syndrome, fever, symmetric distal polyarthritis of the hands and feet, skin rashes (“rash ”), Being indistinguishable from those of the DM, as well as the“ mechanic's hands ” [7].
Inclusion body myositis: Inclusion body myositis (MCI) is the most common and disabling inflammatory myopathy among people age 50 and older [9]. Unlike the predominant dermatomyositis and polymyositis in females, as in most systemic autoimmune diseases, MCI is more common in males [8].
In inclusion body myositis: the condition begins insidiously, usually asymmetrically, progressing for years, sometimes making it difficult to distinguish it from motor neuron disease or late- presenting dystrophy. The clinical findings of MCI are the distal beginning in the flexors of the fingers in the upper extremity, with atrophy of the forearm, of the anterolateral compartment of the legs (dorsiflexion of the foot), associated with atrophy of the quadriceps, which makes it somewhat characteristic of MCI because most myopathies mainly affect proximal muscle groups [7,11].
Patients complain of difficulty climbing stairs, standing from a chair, and frequent falls. Limb weakness is usually accompanied by moderate facial weakness and compromised axial musculature, which can result in camptocormia or a droopy head syndrome. Difficulty swallowing (dysphagia), occurs in more than half of cases [7].
Infectious myopathies: In general, they appear suddenly and in a generalized way, in fact, myalgias are considered within the clinical manifestations of a cold and it is peculiar that they are self-limited. The main infectious cause of myalgia is viral infections, which in turn have the influenza virus as the main exponent, other examples of viral infections can be, for example, cytomegalovirus, parvovirus B19, arbovirus, as in the case of dengue virus. coxsackie, hantavirus, and HIV, usually presenting as a prodromal symptom.
Among the infectious causes, there is also the multifactorial bacterial etiology. Streptococcal infection deserves a special mention, since the manifestation of myalgia in the course of an infection caused by this agent is usually common in invasive infections such as pneumonia, bacteremia, toxic shock syndrome, and pyomyositis; The presence of myalgias has also been described as part of the post streptococcal syndrome, which is normally composed of various non-suppurativesequelae such as pneumonitis, hepatitis, vasculitis, uveitis, scleritis, erythema nodosum, rheumatic fever and post streptococcal rheumatic arthritis, in this case more than of a prodrome it is a severe presentation of the picture, called severe reactive myalgia syndrome [12,13].
They are a group of clinically and genetically heterogeneous diseases that primarily affect the muscle fiber, the neuromuscular junction and the peripheral nerves until reaching the motor neurons of the medullary anterior horn, most of which appear as muscle weakness and hypotonia at birth or during the first year of life [14-16].
These pathologies present different degrees of functional limitation due to weakness of the skeletal musculature and secondary articular contractures, and may also be associated with cardiac compromise such as cardiomyopathies and conduction disorders, and also with respiratory compromise with compromised ventilatory mechanics. Hereditary neuromuscular diseases cover different causes, among them we find metabolic and congenital [15].
Metabolic myopathies
They are a group of inherited disorders caused by enzyme deficiencies that compromise the muscle's energy system, block energy production, muscle cells cannot work properly, and interfere with muscle function [2,17].
From the etiopathogenic point of view, metabolic myopathies have been grouped into:
• Glycogenmetabolismdisorders.
• Disorders of lipidmetabolism.
• Mitochondrialrespiratorychaindefects.
• Purine metabolism disorders (myoadenylatedeaminase deficiency).
The pain arises in relation to exercise, when the energy demand exceeds the muscle's ability to produce ATP (adenosine triphosphate). Depending on the type of enzyme defect, muscle pain and other symptoms typically appear at a specific phase of exercise. The most common cause of myoglobinuria in adults is CPTII (Carnitinepalmitoyltransferase 2) deficiency, followed by McArdle disease and very long-chain acyl coenzyme A dehydrogenase deficiency (VLCAD) [5].
Its manifestations can be very variable, depending on the age of onset and environmental factors. They can be grouped clinically into three large groups of clinical manifestations:
• Permanent symptoms (progressive muscle weakness).
• Episodic or intermittent muscle dysfunction symptoms (exercise intolerance, myalgia and/or myoglobinuria).
• Mixed: syndromes in which both types of symptoms coexist.
In disorders of glycogen metabolism, symptoms typically appear in the early stages of moderate or intense exercise, characterized by the presence of brief, intense contractions in isometric exercises, and eccentric contractions, such as lifting weights, also often triggering symptoms [5].
In disorders of fatty acid metabolism, symptoms appear after prolonged exercises of mild intensity, especially in fasting conditions or during feverish illnesses (Figure 4). Muscle pain can be accompanied by edema and inflammation and cramps, and if the episode is severe enough it can cause rhabdomyolysis, with significant elevation of CK5.
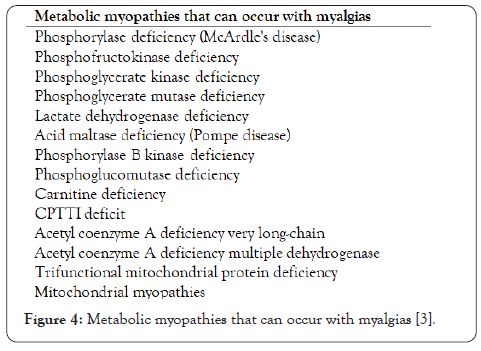
Figure 4 : Metabolic myopathies that can occur with myalgias [3].
Congenital myopathies
It covers pathologies in which there is an alteration of the contractile apparatus and the different components that condition its normal functioning. The clinical spectrum is broad, with great variability ranging from neonatal involvement to presentation symptoms in childhood or in adults with mild symptoms. The distribution of weakness is usually generalized or more pronounced in the axial, proximal, and facial muscles. The course of the disease is usually slowly progressive or relatively stable, and the levels of muscle enzymes are often normal or slightly elevated. In general there is no cognitive impairment [14].
Some patients with type 2 myotonic dystrophy may associate myalgias. Other examples are 2I girdle dystrophy, 2L girdle dystrophy, and Becker muscular dystrophy can also cause cramps and myalgia. In almost all cases, myalgias appear associated with exercise and always accompanied by other specific signs or symptoms: weakness, myotonia, atrophy, hypertrophy or episodes of rhabdomyolysis [5].
They occur secondary to the ingestion of some substances, mostly drugs, which due to their active ingredient or their mechanism of action present metabolic activity that generates the clinical manifestations of myalgia, in most cases these will have a character transient and will depend on the dose of the drug in question, to adequately illustrate this scenario we will pay special attention to myalgias secondary to the use of statins, d-penicillamine and the use of succinylcholine. The first ones are due to the activity of coenzyme A reductase, it occurs in the use of top doses, especially simvastatin, so the way to control these myalgias is to standardize the use of intermediate doses to avoid myalgic manifestations [18- 20].
With d-penicillamine there is no clear dose relationship. It has a frequency of 1% associated with rheumatoid arthritis, in which it begins during any stage of treatment. Weakness is proximal and can be associated with dysphagia (40%), myalgia, itching in some patients, and blockage in cardiac conduction. D-Penicillamine can also induce myasthenia gravis, neuromyotonia, and pemphigus [21].
Diagnosing a muscular disease can become a challenge for the health professional, due to the diversity of symptoms and clinical presentations that they manifest; The number one step for a proper diagnosis of myalgia is the collection of patient data through the medical history, which should determine three main variables: scope, class and location of pain, which provide predominant clues about the cause and evolution. From muscle aches among these two factors, other key components of the diagnosis must in turn be determined: i) sudden onset of pain; ii) formation of bruises; iii) persistence of pain; iv) rapid pain relief; v) severe pain or; vi) the appearance of pain at rest (Figure 3) [2].
The clinical history should allow us to find out what the fundamental symptoms are (pressure sensation, sensitivity to touch, stiffness, heaviness, stiffness, etc.) [22]. Other muscle symptoms that are present along with myalgia often provide the clue towards a diagnosis. Among these we can find weakness, cramps and myotonia, as well as the type of pain [2,3]inquire about its location, the start time and its evolution, possible triggers, associated symptoms or signs; as well as the existence of a relevant medical history, a family history of similar symptoms and a history of exposure to drugs [22]. An example is statins as they are common
inducers of muscle symptoms. Up to 29% of statin-treated patients experience a series of related muscle side effects from very mild to severe. In cases of exercise-dependent myalgia, a possible metabolic muscle disease should be considered. It is important to determine the exact moment of the onset of muscle pain, in order to determine thecorrect diagnosis. In some diseases such as Duchenne muscular dystrophy and Becker muscular dystrophy, myalgias occur at the beginning of the disease, and sleep or bedtime is an aggravating factor [23].
The second step is the physical examination, which establishes the following sections: i) the identification of skin lesions; ii) the evaluation of the active, passive mobility and inflammation of any joint of the body; iii) neurological examination which should: "evaluate the function of the eyelid lift and eye movements to rule out a chronic progressive external ophthalmoplegia [...] that is frequently secondary to a mitochondrial disease and can be associated with nonspecific myalgias" [22]; iv) exploration of muscle strength in relation to its function, which: “details whether you can get up from the floor or from a chair without support, if you can get up from the stretcher with anterior trunk flexion without help, if you can walk on tiptoe and jump on the heels, jump on the toes of both feet ” (Figure 3) [22].
The examination of the patient with muscle pain must be complete, since myalgias often have a different cause than myopathy. The search for skin lesions, the exploration of passive and active joint mobility, as well as the search for signs of joint inflammation should always be included. The examination of muscle strength, in addition to being done manually muscle to muscle, must include a functional examination through the description of the maneuvers that the patient can do [22].
This in order to differentiate if there is an indication of a possible muscle disease, since that there are diseases such as polymyalgia rheumatica (PMR), which according to Healey (1984) describes a diagnosis [24].
• Persistent pain (for at least one month) that affects at least two of the following areas: neck, shoulder girdle and pelvic girdleb.
• Morningstiffnessfor>1hour.
• Age>=50 years.
• Erythrocyte sedimentation rate (ESR) >=40mm/h.
• Rapid response to glucocorticoid treatment.
• Absence of other defined musculoskeletal diseases [24].
Polymyalgia rheumatica (PMR) is a clear example in which muscular pain, in exceptional cases, can be an indication of a muscular disease, therefore, the importance of a timely and reliable diagnosis. Polymyalgia rheumatica is an inflammatory disorder. The highest incidence is in people older than 65 years, with a peak of age between 70-79 years, characterized by intense pain and stiffness that affects the shoulders and proximal parts of the arms bilaterally. Pain and stiffness are also common in the neck. Patients have morning stiffness that lasts between 45-60 min, it worsens after rest or when the patient is inactive for a long time. On physical examination, active shoulder movement is restricted due to pain without clinically observable edema. In laboratory tests, increases in acute phase reactants (that is, sedimentation of erythrocyte rate and C-reactive protein) can be observed, this being a characteristic feature of the disease [25]. Therefore, myalgias are caused by strains, cramps, muscle breaks, which in turn are characterized by muscle spasms and severe pain related to functional limitation of the affected area, which would lead to palpation (exploration) to identify signs ax that would rule out minor or low-level injuries.
The diagnostic study for myalgia should be carried out in a standardized way in order to avoid missing important information and to avoid invasive examinations if not necessary [2,3]. The initial study of a patient with myalgia includes general tests with ion determination, liver and kidney function tests, vitamin D, and thyroid function. Plasma muscle CK levels should always be studied, at least on three different occasions, taking care that the patient does not make physical efforts the days prior to each determination. If CK levels are always normal, the origin of the myalgias will most likely be different from a primary muscle disease. Myalgias secondary to toxins (drugs, alcohol) can have normal CK.
The exercise test in ischemia: "serial measurements of lactate and ammonia before and during exercise in ischemic conditions can detect absence of lactate production and defects in glycogen metabolism" [2].
In turn, it is vitally important to use magnetic resonance imaging and musculoskeletal ultrasound when significant injuries are identified. Similarly, other diagnostic tests such as blood biochemistry can be used where "inflammatory markers and rheumatic serology may indicate non-muscular causes" [2]; Electromyography: it is based on collecting muscle action potentials by means of a bipolar needle electrode that is incorporated into the muscle; Muscle MRI: Atrophy, fatty infiltration, or edema may be seen in skeletal muscle; muscle biopsy facilitates the diagnosis of neuromuscular disorders, endocrinopathies, toxins, infections and other abnormalities thereof; Last but not least, genetic testing can be implemented, which is recommended if there is no presumption of a genetic alteration. A series of gene panels is proposed that are related to muscle diseases (Figure 5) [2,26].
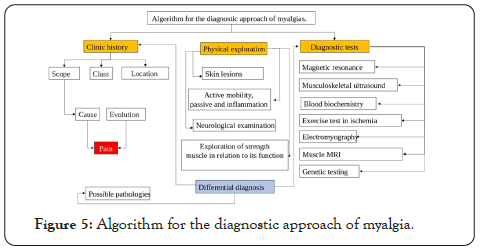
Figure 5 : Algorithm for the diagnostic approach of myalgia.
In the case of suspected rheumatic polymyalgia, the rate of globular sedimentation and/or the C-reactive protein should be studied [22]. There is no pathognomonic test or established diagnostic criteria for polymyalgia rheumatica PMR [1].The diagnosis of myalgia is summarized in Figure 6.
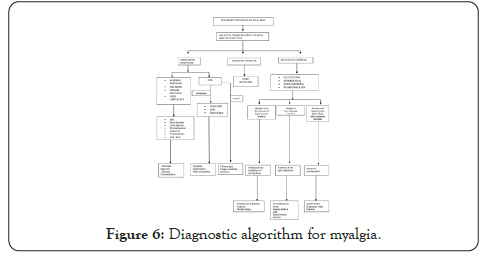
Figure 6 : Diagnostic algorithm for myalgia.
Many conditions can present clinically as myalgias or polymyalgicsyndrome, among them are the following [24]:
• Active infection (e.g. viral infection, infective endocarditis and tuberculosis).
• Malignancy.
• Rheumatic diseases (e.g. rheumatoid arthritis, systemic lupus erythematosus and polymyositis).
• Drug-induced myalgia (e.g. statins).
• Chronic pain syndromes (e.g.fibromyalgia and osteoarthritis).
• Soft tissue injuries (e.g. rotator cuff injuries).
• Endocrine disorders (e.g.thyroid disorders).
• Neurological conditions (e.g. Parkinson's disease).
Many patients with diffuse myalgic disease do not have a specific etiological diagnosis despite extensive research. Due to this, it is important to guide diagnostic studies and their interpretation according to clinical suspicion.
In the patient with elevated ESR or CRP, the presence of systemic inflammation should be considered, as in infectious processes or systemic rheumatologic diseases such as Polymyalgia Rheumatica and Inflammatory Myopathy. Conversely, normal ESR levels are the expected finding in fibromyalgia patients. An important clinical finding is that Fibromyalgia patients usually do not have a good response to corticosteroids.
Patients with Polymyalgia Rheumatica, in addition to having usually high inflammatory markers (ESR or PCR), may also have normochromic normocytic anemia and liver tests may be moderately altered, especially alkaline phosphatase [24].
Caution should be used since elevations of ESR or PCR are not specific and normal levels of these do not rule out a particular cause of myalgia [27].
It is important to note that obese patients may have elevated inflammatory markers due to their disease, as it is characterized by a low-grade systemic inflammatory response. Abdominal adipose tissue is an important source of cytokines such as TNF-α and IL-6, which increase hepatic production of C-Reactive Protein (PCR). However, careful interpretation of clinical data in obese patients is necessary, since fibromyalgia in these may present with elevated inflammatory markers [28].
Autoimmune marker tests should be reserved for patients in whom the probability of this diagnosis is suspected, and if they are positive, they should undergo the necessary analysis to determine whether autoimmune disease is the cause of the myalgias or other etiologies should be considered.
In the context of differential diagnosis, it is of great importance to keep in mind that in addition to the initial laboratory studies for a patient with myalgia, electromyography (EMG) and muscle biopsy are useful for seeking specific etiological diagnoses. However, most patients with myalgia will not require a muscle biopsy. ESR and CK levels could be one of the best parameters for deciding whether a patient would benefit from an EMG. In the case of being elevated, the possibility of a systemic etiology is considered rather than of the muscle tissue itself. "A retrospective/prospective study showed that the probability that a patient with isolated muscle pain and
CK levels <7 times the normal upper limit has a defined myopathy is 2%." Also, it must be taken into account that the majority of patients have a normal muscle biopsy result. This test is reserved for patients with suspected neuropathic processes, metabolic or inflammatory myopathies [29].
Management of myalgias generally depends on the underlying cause. When the cause is not easily identified, patients should be treated symptomatically and should be observed periodically. In the absence of contraindications, empirical treatment may include heat, rest, paracetamol, non-steroidal anti-inflammatory drugs, and/or muscle relaxants [27].
If the myalgias correspond to muscle injuries, treatment could include NSAIDs orally, topically, or by injection. Selective COX-2 inhibitors and muscle relaxants could also be used [2].
In the case of myofascial pain, the most widely used medications are tricyclic antidepressants, muscle relaxants, benzodiazepines, calcium channel blockers, non-steroidal anti-inflammatory drugs, corticosteroids, opioids, botulinum toxin or capsaicin [2].
Initial treatment of inflammatory myopathies (dermatomyositis, polymyositis, and autoimmune necrotizing myositis) includes glucocorticoids, often prednisone at a dose of 1mg/kg/day orally in the first few weeks. When the onset of the disease is severe or the patient worsens rapidly, the therapy of choice is intravenous glucocorticoid for 3 to 5 days and then switch to glucocorticoid orally. If the response to glucocorticoids is insufficient, the therapy of choice is intravenous immunoglobulin. If the patient finally does not respond to glucocorticoids or immunoglobulin, it is recommended to reconsider the diagnosis or start treatment with rituximab if the diagnosis is reconfirmed [9].
In the case of diagnosing fibromyalgia, non-pharmacological measures of treatment include: rehabilitative and physical treatment, psychological treatment or natural therapies (there is not enough evidence on the latter). The most frequently used pharmacological measures are: antidepressants, muscle relaxants, pregabalin, tramadol, paracetamol (pain reliever most used in fibromyalgia) or other drugs considered by the treating physician [2].
If the patient is diagnosed with Polymyalgia Rheumatica (PMR), the treatment of choice is prednisone 15-20 mg/day orally, initially for 4 weeks. The response to steroids is generally rapid and 70% of patients improve in the first week. If after 4 weeks the patient has improved and has an adequate response, it is recommended to decrease the prednisone dose 2.5 mg every 2 to 4 weeks until achieving a dose of 10 mg/day. Once the patient is stable, this dose can be decreased 1 mg every 4 to 6 weeks, until achieving a maintenance dose of 7 mg/day, which must be continued for at least 12 months [24].
In the case of patients who develop statin myalgias, a comprehensive evaluation must be made and treatment defined according to CK levels and the symptoms that appear. In patients with CK levels>10 times the normal limit, suspension of statins should be considered. Other options that the treating physician should consider are: evaluating the tolerability of symptoms with the patient versus the need for statin consumption, trying a lower dose, changing the statin or changing to other medications. All of the above must be determined by the doctor [30].
Polyarthralgia is defined as joint pain in more than 4 joints [31,32]. Among the different causes of joint pain are viral infection, bacterial infection, crystal-induced synovitis, systemic rheumatic diseases, systemic vasculitis, spondyloarthropathies, endocrine disorders, malignant causes, such as metastatic cancer, and others such as osteoarthritis, fibromyalgia, among others [31]. Polyarthralgia is a term that is commonly confused with polyarthritis, but the latter is defined as joint disease where more than 5 joints are involved [33] and is accompanied by polyarthralgia (joint pain) and joint inflammation.
In many of these joint pathologies, the joints present symptoms of synovitis, that is, inflammation (for example in rheumatoid arthritis, Still's disease and psoriatic arthritis, etc.); but in others this joint inflammation is not involved as in fibromyalgia, joint hypermobility syndrome (BJHS) and viral arthritis. Therefore, polyarthralgias can be classified into inflammatory and non- inflammatory causes. The most common non-inflammatory condition is osteoarthritis; and there are over 100 potential causes of inflammatory arthritis, the majority of cases attributable to rheumatoid arthritis, spondyloarthropathies, and psoriatic arthritis [34]. Polyarthritis could initially be confused with self-limited joint pain due to periarticular pathologies such as tendinitis and bursitis (Figure 7) [35], therefore a good medical history, good initial physical examination and relevant laboratories are requiredto reduce possible differential diagnoses [36,37].
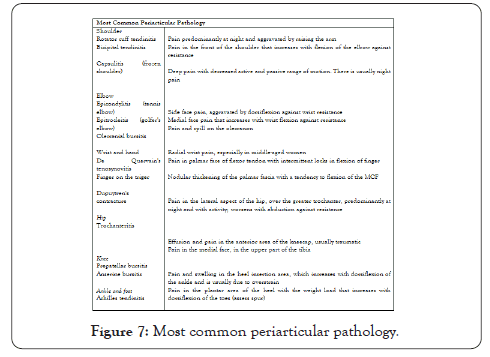
Figure 7 : Most common periarticular pathology.
Polyarthritis is the leading cause of disability in the United States, accounting for approximately 20% of outpatient visits. It is estimated that 25% of patients, after the disease has started, in 7 years will not be able to work. Among the most common pathologies are osteoarthritis, rheumatoid arthritis (RA), pseudogout and gout. The prevalence of polyarthropathies increases with age; an estimated 60% of adults over 65 in the US suffer from chronic joint symptoms. The incidence rate worldwide is 15 to 40 new cases/100,000 people/year [36].
Joint pain can be classified according to joint involvement as inflammatory and non-inflammatory (Figure 4) [33] and according to the time of evolution in acute and chronic. Acute polyarticular pain is defined as pain that is less than 6 weeks, and chronic pain is defined as pain that is greater than 6 weeks [31,38]. It is important to mention that juvenile idiopathic arthritis is the most frequent chronic rheumatic disease, and covers all forms of chronic arthritis in the pediatric age [39].
Diet and lifestyle, act as protective or risk factors, which are of importance and clinical monitoring, this because technically all these factors are modifiable. Although it has been shown that the female gender influences a risk 3 times greater than that of the male [3,4]. Within this, there are modifiable factors associated with hormonal manipulation, including oral contraceptives, hormone replacement therapy, parity and breastfeeding [40].
Smoking
Smoking has been shown to contribute an increased risk for Rheumatoid Arthritis (RA) by 18-25%, especially in men with seropositive RA, according to [the Epidemiological Investigation of RA (EIRA) in Sweden], the interaction was reported with the alleles of the shared epitope, where smoking patients with two A + copies for this epitope had a relative risk of 21.0, compared to non-smokers. The two United States-based cohorts, “Nurses Health Study and Nurses Health Study II”, with their results of 238,308 women evaluated aged 25-42 years, suggest smoking as a dose-dependent risk factor in packets/year, where consumption greater than 10 packages/year makes the relative risk evident. Also, it's supposed to be a long latency factor [40].
Red meat consumption
Unlike the protective influence of the Mediterranean diet, it is believed that there is a high risk factor in people who frequently consume red meat, this due to the inverse relationship with the consumption of fruits, vegetables and fish oil, and the association of these meats with a high intake of saturated fat, calories and a low fiberdiet [40].
Obesity
Regarding obesity, two ways have been proposed in which the relative risk for arthritis is increased, considering the first, being the increase in available amount of estrogen due to an increased conversion of androsterone into estrogens, and one decrease in sex hormone binding globulin, with a higher prevalence in postmenopausal women. The other proposed route of interaction is through leptin, which is a hormone secreted by adipose tissue. In obese patients, increased serum levels are found, which responds as a modification of the immune response to Th1 phenotypes and a substantial increase of proinflammatory cytokines (IL-1, TNF-a) [40].
Social class
Social class and education have been considered as a marker for lifestyle variables, and has been associated with a poor prognosis in established rheumatoid arthritis. In a Swedish study, an inverse association was found between higher education and the incidence of rheumatoid arthritis, especially seropositive. This was supported by the EIRA study, in which patients without a college degree were at increased risk compared to those with at least a college degree [40].
Breast-feeding
The first episode of lactation has been associated with an increased risk for rheumatoid arthritis in susceptible subjects, this due to the production of prolactin as a pro-inflammatory hormone, which could trigger occult arthritis [40].
Infections
Infections have been speculated as a trigger in the pathophysiology of rheumatoid arthritis, especially viral infections such as Epstein Barr Virus and Parvovirus. In addition, an epidemiological link between different types of microorganisms present in periodontal infections has been proposed, which is recognized as a risk factor for arthritis [3,4].
Identifying the cause of joint pain is difficult since many differential diagnoses are found, including periarticular pain (Figure 7). Therefore, a good medical history and a complete physical examination are necessary to correlate findings with possible causes (Figures 8 and 9) [31,32]. To reduce possible differential diagnoses, it is necessary to know the following clinical factors: chronology and course of the disease, existence of inflammation, extra-articular manifestations, distribution and demographics of the patient [31].
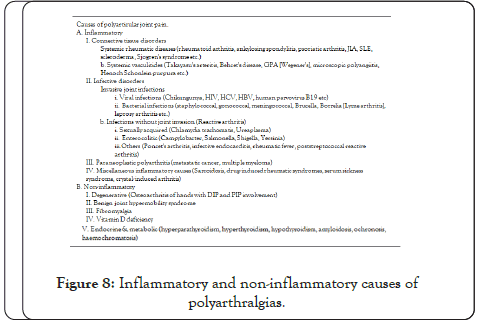
Figure 8 : Inflammatory and non-inflammatory causes of polyarthralgias.
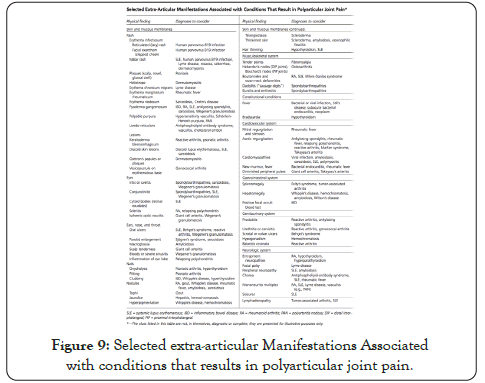
Figure 9 : Selected extra-articular Manifestations Associated with conditions that results in polyarticular joint pain.
Clinic history
In the anamnesis, it is important to take into account the patient's age, gender, occupation, toxics, personal and family history, contact with animals and sexually transmitted diseases [35,38]. To guide diagnosis among the most common causes of joint pain (Figure 10). Likewise, a rigorous system examination must be carried out to identify extra-articular symptoms that allow us to target specific disorders [32].
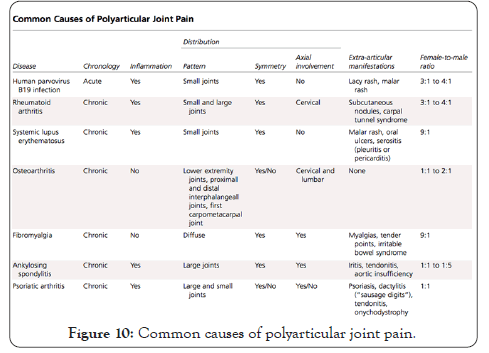
Figure 10 : Common causes of polyarticular joint pain.
As for the current disease, it is very important to investigate the evolution time of the clinical picture, if it is less than 6 weeks, causes of acute joint pain such as viral infections would be suspected. You have to ask the types of joints involved and if there is symmetry (when at least half of the joints involved are symmetrical) [38]. There are different patterns of joint involvement, the main 3 are migratory (characteristic of acute rheumatic fever), additive (pattern suggestive of spondyloarthropathy) and intermittent (adult Still's disease is suspected) [34,37]. You have to assess whether the pain is inflammatory, characteristic because it is not relieved by rest, or mechanical [35,41]; if there are clear signs of joint inflammation (flushing, heat and inflammation) and evaluate the extra-articular manifestations that can be related to polyarticular conditions (Figure 9) [31]. Finally, it is important to investigate the existence of warning signs and symptoms, such as the B symptoms that make us suspect malignancy, among others (Figure 11) [35,38]. Gender is also related to certain pathologies, such as rheumatoid arthritis that mainly affects women in their 40s and 70s [41,42].
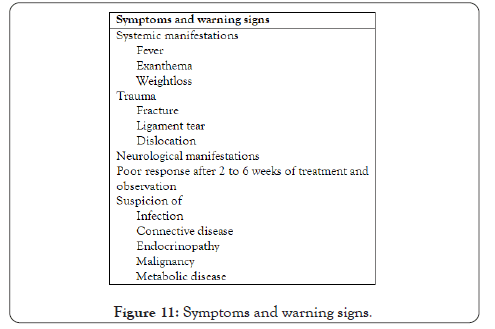
Figure 11 : Symptoms and warning signs.
Once the diagnostic approach has been made with the medical history and the physical examination, we can request paraclinical tests that help us confirm or rule out joint pathologies. As diagnostic aids we have analytical tests such as blood count, uric acid and CPK, arthrocentesis and diagnostic images that are also helpful [35].
Analytics
Initially, a complete blood count, uric acid, CPK, partial urine and a complete metabolic panel should be requested [31,35]. Depending on the clinical suspicion, paraclinical examinations can be expanded, among these [35]:
• Immunological tests: if connective tissue diseases or vasculitis are suspected, rheumatoid factor (RF), electrophysiological and immunoglobulin studies, antinuclear antibodies (ANA), anti- neutrophil cytoplasm antibodies (ANCA), anti-DNA can be requested.
• Serological tests: if polyarthralgias of infectious causes, reactive arthritis or rheumatic fever are suspected.
• Histocompatibility tests: if we suspect spondyloarthropathy, HLA B27 should be ordered.
Arthrocentesis
Synovial fluid cytochemistry should be performed when microcrystalline or septic pathology is suspected. Synovial fluid cytology is a fundamental tool that guides diagnosis in a quick and simple way [39]. This test analyzes the microscopic vision, the cytochemical of the liquid, the presence of crystals, the concentration of glucose must be cultivated and analyzed, depending on the results, the synovial fluid categorizes us as inflammatory, non-inflammatory and septic (Figure 12) [31].
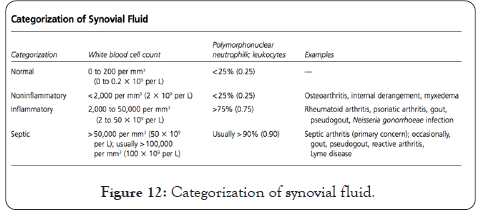
Figure 12 : Categorization of synovial fluid.
Diagnostic Imaging
Radiography can contribute to the diagnosis, especially when rheumatoid arthritis (RA) and spondyloarthropathy are suspected [38]. In RA, radiography is useful in monitoring radiological progression, by applying indices that evaluate erosions and the reduction of joint space [43]. However, the destructive changes and erosions that can be observed on radiographs appear at a late stage of the disease [44].Linear cartilage calcifications in joints such as the knee is suggestive of pseudogout [38].
Ultrasound (ECO) is a recently used technique in rheumatoid arthritis that includes the use of gray scale images (EG) that evaluate anatomical structures and Doppler modalities (Power Doppler- PD), it is a technique non-invasive, quicker and cheaper than magnetic resonance imaging (MRI) and can be easily performed in routine clinical practice [43]. It is mainly used to assess severity and make a differential diagnosis with arthritis. But it is also used, as a clinical follow-up, to evaluate the efficacy of treatment in certain pathologies [38].
There is increasing evidence that radiological evaluation methods, especially high-resolution ECO and MRI, are more sensitive in the detection of synovitis, in the evaluation of the progression of joint damage, in the detection of effusion, destructive changes and dislocation, but its high cost and availability does not allow its constant use [43,44].
All these diagnostic tests must be oriented according to the initial diagnostic suspicion, and must provide us with clues for an accurate diagnosis of joint pathologies (Figure 13) [31] both acute and chronic (Figure 14) [45]. Therefore, an accurate diagnosis requires a complete medical history, a detailed physical examination, and relevant paraclinical tests for diagnostic suspicion. Therefore we expose the diagnostic algorithm of the article entitled ¨Acute joint pain¨ (Figure 15) [35].This seems very successful and can guide us to the next step when we suspect a polyarticular pathology.
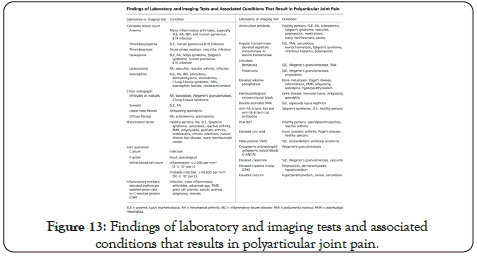
Figure 13 : Findings of laboratory and imaging tests and associated conditions that results in polyarticular joint pain.
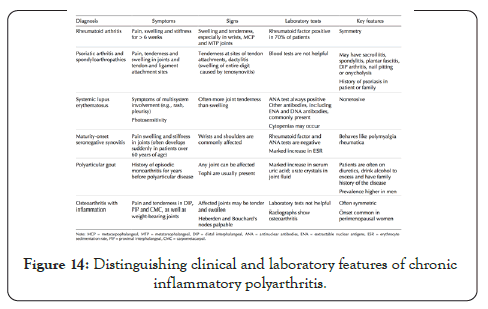
Figure 14 : Distinguishing clinical and laboratory features of chronic inflammatory polyarthritis.
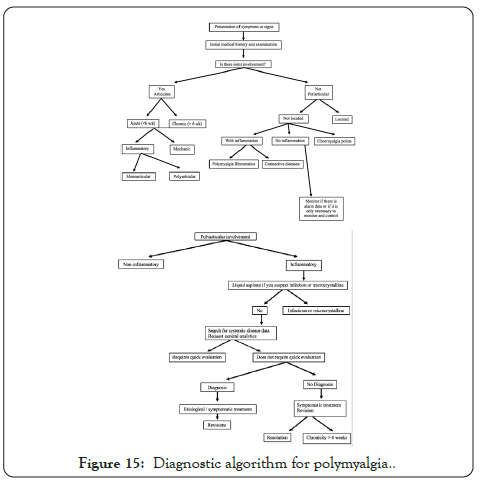
Figure 15 : Diagnostic algorithm for polymyalgia.
Polyarthritis, term used to define the involvement of at least 5 joints with arthritis. Since it is difficult to differentiate joint involvement from causes that generate polyarticular pain, and taking into account the wide range of diseases that can present with similar characteristics, from rheumatoid arthritis to infectious diseases. Therefore, the classification of each patient according to phenotypic, genotypic characteristics, sociodemographic factors and the characterization of polyarthritis according to the time of evolution, symmetry, the pattern of joint involvement, type of affected joints, clinical course, and associated systemic involvement will be very important.
These are characteristic patient patterns, can reduce the possibility of differential diagnoses, based on epidemiological data and pathophysiological incidence, for example: in a young male patient, systemic lupus erythematosus will be the last option for differential diagnosis38.
• Young males: Spondyloarthropathy. Also, do not forget the arthritis associated with sexual transmission in sexually active individuals.
• Young women: Connective tissue disorders (connective diseases) and viral arthritis (parvovirus B19, rubella).
• Middle-aged women: rheumatoid arthritis.
• Elderly: polymyalgia rheumatica, calcium pyrophosphate arthritis (crystal arthropathy), or giant cell arthritis (Figure 16) [46].
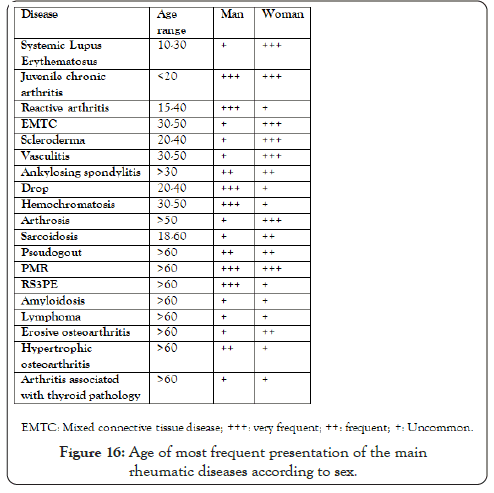
Figure 16 : Age of most frequent presentation of the main rheumatic diseases according to sex.
Onset may be abrupt, characteristic of septic and microcrystalline arthritis, or gradual, typical of connective diseases [46].
If the polyarthritis is limited to an evolution of less than 6 weeks, it is considered as acute and these are frequently associated with viral infections. If the evolution picture is longer than 6 weeks, it is classified as chronic polyarthritis, in which case rheumatoid arthritis is considered more frequent [38].
It is classified as symmetric polyarthritis, if at least half of the affected joints are ipsilateral. The involvement of large and/or small joints will also delimit us and guide us towards an accurate differential diagnosis, taking into account symmetry and involvement [38].
• Symmetric involvement of small joints (metacarpophalangeal, interphalangeal, and metatarsophalangeal): rheumatoid arthritis, systemic lupus erythematosus, viral arthritis, psoriatic arthropathy [46].
• Large joints (ankles, knees, elbows, shoulders and wrists): spondyloarthropathies (psoriatic arthropathy, reactive arthritis, enteropathicarthropathy), rheumatic fever, polyarticular gout, Behçet's disease, sarcoidosis [46].
• Detection of the involvement of the axial skeleton (spine) is important, since this reduces the differential diagnosis to the group of spondyloarthropathies (ankylosing spondylitis and the rest of spondyloarthropathies) (Figures 17 and 18) [46].
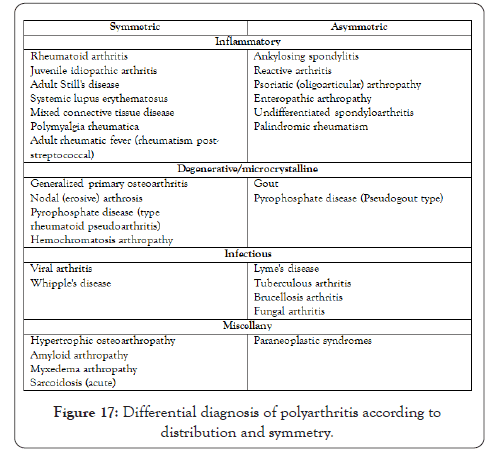
Figure 17 : Differential diagnosis of polyarthritis according to distribution and symmetry.
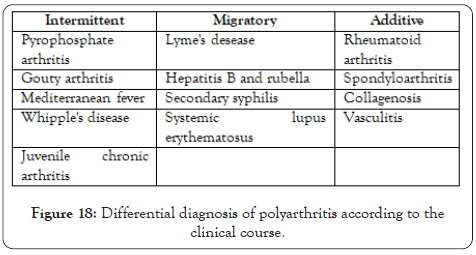
Figure 18 : Differential diagnosis of polyarthritis according to the clinical course.
Migratory
At the beginning of arthritis, one or several joints are affected, which improvement coincides with the involvement of a new joint. It is usually typical of acute polyarthritis, such as acute rheumatic fever and Neisseria arthritis [38].
Additive
Involvement of new joints while those previously affected remain symptomatic. Classic examples of this pattern are spondyloarthropathies, rheumatoid arthritis, osteoarthritis, and reactive arthritis [38].
Intermittent
Complete remission of signs and symptoms between different episodes; elderly with still disease, familial Mediterranean fever, microcrystalline arthritis and Whipple's disease [46].
Drug-associated inflammatory arthritis is generally a diagnosis of exclusion, but it cannot be completely ruled out, as an example is the case of migratory polyarthritis associated with clopidogrel and ticlopidine: Clopidogrel is a selective inhibitor of P2Y12, Belonging to the thienopyridine family, the exact mechanism of inflammatory arthritis is unknown, but mouse models have suggested that it may be due to an effect on cells and not on platelets directly, increasing proinflammatory factors (IFN-g cytokines , IL-6 and IL1b) [47].
The combination of pancreatitis, panniculitis, and polyarthritis (PPP Syndrome) is a very rare complication of pancreatic disease. The symptoms and characteristics of arthritis are usually symmetrical involvement in large and small joints (knees, heels, elbows, metatarsus and metacarpus) but it can also present as large joint monoarthritis. The pathophysiology of joint involvement is unknown for sure, but it has been proposed that the symptoms are due to the release of lipolytic pancreatic enzymes (lipase and amylase) into the bloodstream, subcutaneous adipose tissue, and bones, and the hypothesis is also proposed of fatty acid release from adipose tissue due to increased lipolysis could be the cause of joint pain (Figure 18) [48].
Several primary skin diseases are associated with arthritis and joint symptoms may even be present before skin lesions. Common skin disorders, such as acne and psoriasis, have well-known musculoskeletal manifestations [49].
Psoriatic arthritis(PSA)
Affects between 6% and 42% of patients with psoriasis. Arthritis can precede skin lesions in up to 20% of patients. X-rays can be very helpful in diagnosing psoriatic arthritis. typical findings include erosions, joint space narrowing, bone proliferation, ankylosis, and syndesmophytes [49].
Acne and related syndromes
The incidence of musculoskeletal involvement in fulminant acne is common; In fact, many authors use it as part of the diagnostic criteria. Arthralgia, non-erosive and destructive arthritis, osteitis and lytic bone lesions have been reported with fulminant acne. Pain and prolonged morning stiffness are common. Peripheral involvement tends to involve large joints in an asymmetric, oligoarticular pattern. Radiological findings include narrowing of the joint space, bone erosions, unilateral or bilateral sacroiliitis, and syndesmophytes. Skin lesions occur before the onset of arthritis in most cases; however, arthritis has been reported to precede skin disease. It is important to note that the two medications used in the treatment of acne [49].
Dermatomyositis(DM) is an inflammatory idiopathic myopathy with characteristic skin lesions, usually affecting the muscles of the shoulder and the pelvic girdle. Gottron's papules and Gottron's sign are considered pathognomonic for DM [49].
Arthritis has a high prevalence globally and includes more than 100 types, among which the most common are rheumatoid arthritis, osteoarthritis, psoriatic arthritis and inflammatory arthritis [50]. Among inflammatory arthritis, the most common are rheumatoid arthritis and spondyloarthropathies (a family of inflammatory diseases including psoriatic arthritis and ankylosingspondyloarthritis) [3,4]. This review of treatment will focus on the more common arthropathies already mentioned above, adding ongoing research for new therapeutic options.
The use of oral corticosteroids, intramuscular or intra-articular injections have quick and effective effects, but the risks of adverse effects (diabetes, osteoporosis) limit their uses. These drugs are used especially in cases of early disease or reactivation, combined with methotrexate [3,4].
Disease modifying antirheumatic drugs (DMARDS) are considered the cornerstone of treatment. They are subdivided into conventional synthetic (csDMARD) or specific (DMARDs), within which are biological drugs (bDMARDs) and synthetic (tsDMARDs) such as JAK inhibitors [3,4].
CsDMARD
Includes methotrexate, sulfasalazine, hydroxychloroquine, and leflunomide. Other old ones of this family, that are little used is gold and penicillamine. Methotrexate is the ideal medicine for the management of rheumatoid arthritis, it is effective in early disease and has a good long-term safety profile, used in co-prescription of folic acid to reduce the main adverse effects (macrocytic anemia) [3,4].
bDMARDs
This group of biological drugs includes Tumor Necrosis Factor Inhibitors (TNFi), monoclonal antibodies (infliximab, adalimumab, golimumab and certolizumabpegol, monoclonal antibody IL-6 receptor inhibitor tocilizumab and sarilumab, CD-20 inhibitor rituximab, and the T lymphocyte stimulation inhibitor abatacept) [3,4].
tsDMARDs
Among the specific synthetic drugs are the janus kinase inhibitors (JAK), tofacitinib and baricitinib [3,4].
Surgical intervention
May be required in advanced or refractory cases, surgical procedures include joint fusion, arthroplasty, and synovectomy [3,4].
Psoriasic arthritis
The main pharmacological options are, as in rheumatoid arthritis, the csDMARDs or tDMARDs. The use of intra-articular steroids has been used in monoarticular involvement, but its recommendation has been reduced because it can exacerbate skin psoriasis, hypertension, diabetes and weight gain. Methotrexate is the first line of therapy for csDMARDs, and the most widely used of bDMARDs are anti-TNF. New biologic therapies have been approved for use, such as secukinumab and ixekizumab (monoclonal antibodies against IL-17a), and austekinumab (against IL12/IL23), these have been shown to be more effective for skin psoriasis. An alternative is the 4 phosphodiesterase inhibitor, apremilast [3,4].
Ankylosing Spondylitis
The non-pharmacological intervention with the greatest impact on this disease is physical therapy; stretching exercises for the spine, helps decrease pain, inflammation and maintains spinal motility in the long term [3,4].
The drugs with the greatest importance for pain control and pathophysiology are non-steroidal anti-inflammatory drugs. Conventional synthetic DMARDs (methotrexate and sulfalazine) have no effect and are not approved as a treatment algorithm for ankylosing spondylitis. Biological anti-TNF drugs are highly effective in managing the disease (Figures 19 and 20) [3,4].
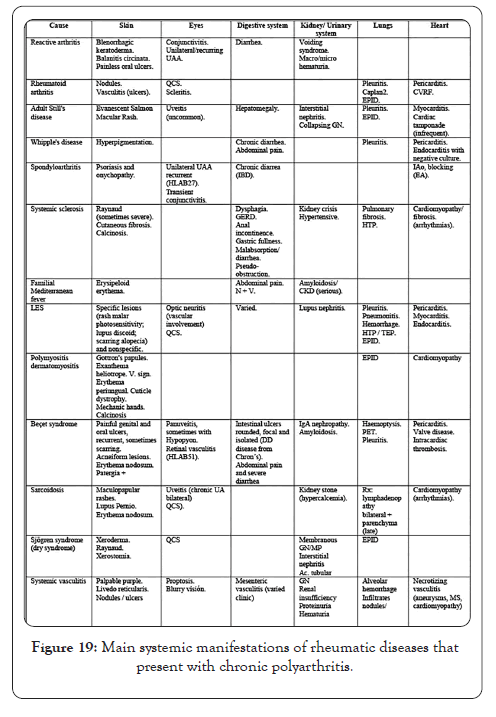
Figure 19 : Main systemic manifestations of rheumatic diseases that present with chronic polyarthritis.
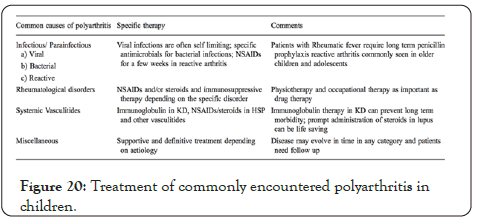
Figure 20 : Treatment of commonly encountered polyarthritis in children.
• Synthesis of an analog, 6-(2,4-difluorophenyl) -3-(3 (trifluoromethyl) phenyl) -2H benzo oxazine-2,4 (3H)-dione (Cf- 02), which shares structural similarity with Quercetin, a powerful flavonoid anti-inflammatory present in many fruits and vegetables. Cf-02 has shown the ability to suppress inflammation and damage to cartilage.
• In an experimental model of RA, Collagen-Induced Arthritis (CIA), Tsai et al, discovered a natural diterpene compound, Sclareol, inhibits the release ofinflammatory cytokines (TNF and IL-6) in synovial fibroblasts and relieves the severity of arthritis.
• In their article, Jung et al, indicate that the active component of the herb Dictamnusdasycarpus, fraxinellone, alleviates synovial inflammation and osteoclastogenesis in mice with collagen-induced arthritis.
Citation: Manotas JA, Pérez SG, Suaréz MJ (2020) Myalgias and Polyarthralgias Syndrome: A Brief Review. Rheumatology (Sunnyvale). 10:262. DOI:10.35248/2161-1149.20.10.262.
Received: 29-Apr-2020 Accepted: 13-May-2020 Published: 20-May-2020 , DOI: 10.35248/2161-1149.20.10.262
Copyright: © 2020 Manotas JA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.