Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Case Report - (2024)Volume 14, Issue 6
Placenta Accreta Spectrum (PAS) is an abnormality of placentation related to high maternal mortality and morbidity. In this report, a case of abnormal placenta invasion, placenta percreta adhering to the urinary bladder, iliac vessels in a pregnant woman with three previous cesarean sections who presented severe hemorrhage intraoperatively requiring massive blood transfusion but with good postoperative outcome. The objective of this report is to demonstrate the successful management of a high complexity PAS case, the importance of surgical planning and a multidisciplinary team in a center of excellence for PAS.
Placenta accreta spectrum; Percreta; Hysterectomy; Maternal near miss; Intraoperative hemorrhage
Placenta accreta spectrum disorder is an abnormality in placentation, in which the placenta-instead of attaching to the decidua basalis abnormally adheres to the myometrial tissue, the decidua basalis being non-existent. Due to this abnormality, there is incomplete separation between the placenta and uterus at the time of delivery, which causes serious complications such as hemorrhage, disseminated intravascular coagulation, multiple organ failure and even maternal death [1,2].
There are 3 degrees of placental invasion: Accreta, increta and percreta. The first degree (accreta) consists of placenta adhered to the myometrium, but without signs of invasion; the second degree (increta) consists of myometrial invasion by the placenta; the third degree (percreta) occurs when the placental invasion exceeds the serosa, which may affect and invade adjacent structures [3].
Since placenta percreta is the most severe form, producing an especially high risk of maternal morbidity 86% versus 27% in placenta accreta. However, it is the rarest form of presentation, corresponding to 5% to 7% of cases [4-6].
The main risk factors for placental invasion disorders are previous cesarean deliveries and placenta previa. The risk of placenta accreta spectrum disorders increases with the number of cesarean sections, reaching a rate of 67% in patients with five or more previous cesarean sections [3]. An increase in the incidence of this disease has been observed in recent years, due to the increasing rates of cesarean sections [7]. The group with the highest risk of PAS are women with previous cesarean section, presenting a case of placenta previa in the second trimester [3]. By the end of 2017, every 313 pregnant women had at least one pregnant woman diagnosed with placenta accreta spectrum [8].
A 44-year-old woman with 3 previous cesarean sections, was transferred to the reference center for diagnostic and management of placenta accreta spectrum, Hospital de Clinicas de Porto Alegre (HCPA). The patient was referred to the reference center due to placenta previa and vaginal bleeding, at 27 weeks of gestational age. She required 4 units of blood transfusion due to a hemoglobin of 5.1 g/L ultimately reaching 7.6 g/L after the procedure. Patient had already received treatment with betamethasone, cefazolin and one dose of immunoglobulin anti-Rho. Subsequently to the patient's transfer to HCPA, her clinical state was stabilized without any new bleedings hence an obstetric ultrasound and Magnetic Resonance Imaging (MRI) of the pelvis were performed. In which they illustrate placenta percreta with invasion to the following structures: cervix, urinary bladder, ureters and left iliac vessels (Figures 1 and 2). Patient developed pneumonia with a positive SARS-CoV-2 test, without the need for mechanical ventilation and complete improvement during hospitalization. In the pre-operative, the patient received 2 units of blood transfusion and iron replacement therapy.
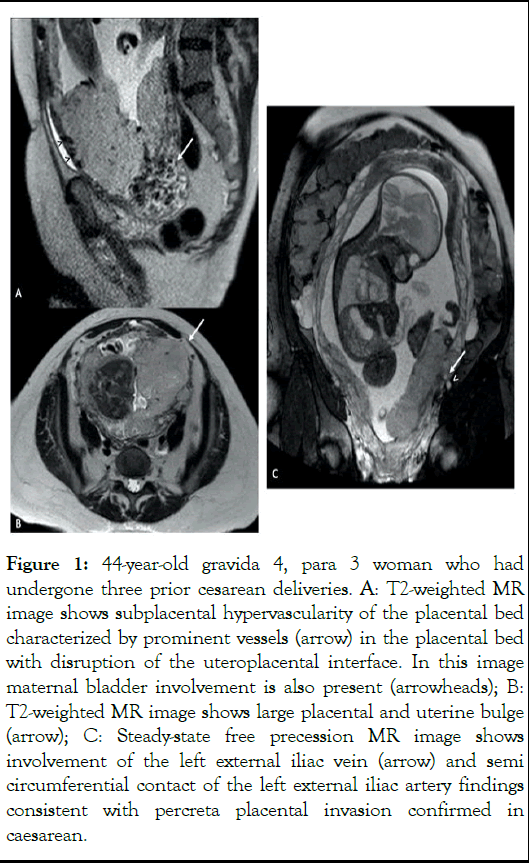
Figure 1: 44-year-old gravida 4, para 3 woman who had undergone three prior cesarean deliveries. A: T2-weighted MR image shows subplacental hypervascularity of the placental bed characterized by prominent vessels (arrow) in the placental bed with disruption of the uteroplacental interface. In this image maternal bladder involvement is also present (arrowheads); B: T2-weighted MR image shows large placental and uterine bulge (arrow); C: Steady-state free precession MR image shows involvement of the left external iliac vein (arrow) and semi circumferential contact of the left external iliac artery findings consistent with percreta placental invasion confirmed in caesarean.
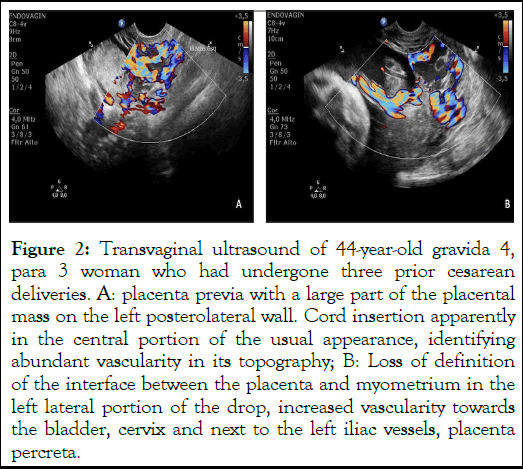
Figure 2: Transvaginal ultrasound of 44-year-old gravida 4, para 3 woman who had undergone three prior cesarean deliveries. A: placenta previa with a large part of the placental mass on the left posterolateral wall. Cord insertion apparently in the central portion of the usual appearance, identifying abundant vascularity in its topography; B: Loss of definition of the interface between the placenta and myometrium in the left lateral portion of the drop, increased vascularity towards the bladder, cervix and next to the left iliac vessels, placenta percreta.
During hospitalization at HCPA, there were board meetings with around 60 healthcare professionals specializing in the management of the spectrum of placenta accreta. The multidisciplinary team was composed of anesthesiologists specializing in high complex cases, oncologists surgeons, vascular surgeons, urologists, obstetricians, neonatologists and obstetrician nurses (Figure 3).

Figure 3: Multidisciplinary team.
The objective of the meetings were to define the surgical approach and provide adequate planning with all the healthcare professionals that would be present on the day of surgery. Including, 10 units of blood, 4 units of plasma, 10 units of cryoprecipitate and 10 units of platelets were reserved. As well as beds in the ICU ward for the patient and a bed in the neonatal ward. The blood bank of the region and other banks of the city were prepared for the possibility of requiring the extra support during the procedure. The patient was admitted for a cesarean section and hysterectomy at 31 weeks. The procedure lasted 8 hours which was performed in the surgery block. The multidisciplinary team was present with the following order of procedures (Table 1).
|
Check list |
A. Team member present |
|
B. Revision of all the surgical and anesthetic material |
|
|
C. Blood products in the room and blood bank available |
|
|
D. Adult and neonatal ICU bed available |
|
|
Anesthesia |
Central and mean arterial pressure access. |
|
Spinal anesthesia. |
|
|
Administered 2.0 g of cefazolin and 1.0 gr of tranexamic acid infusion. |
|
|
Urologist |
Urologist inserted bilateral double J and verified invasion in bladder trigone through cystoscopy. |
|
Interventional radiologist |
Interventional radiologist inserted bilateral intra-aortic balloons in internal iliacs by bilateral femoral approach and selective fluoroscopic catheterization. |
|
Surgical team |
Indwelling bladder catheterization in a closed system. |
|
Cesarean section |
The surgical procedure was started with an abdominal opening through a median xyphopubic incision. Uterine approach through a fundal incision, away from the placenta. |
|
The newborn was born with APGAR 7 in the 5th minute, weighing 1638 g, referred to the Neonatal Intensive Care Unit, due to prematurity. |
|
|
Interventional radiologist |
Inflated arterial balloons shortly after umbilical cord clamping. |
|
Anesthesia |
General anesthesia with 3 aestheticians in the surgical room. |
|
Hysterectomy |
Joint participation of all the surgeons verifying with approach would be best for hysterectomy while leaving placenta in situ. |
|
It is necessary to inflate balloons to occlude the iliac arteries for about 30 minutes in four moments. |
|
|
Coagulation, adequacy of volume and hematological replacement were checked at various times through the use of thromboelastogram. |
|
|
Placenta was maintained in situ, and hysterectomy was initiated by the obstetric team, oncological, vascular and urologist surgeon. |
|
|
Extensive adherence of the placenta to the bladder wall and ureters was verified, with no plan for dissection, requiring a section of both for placental release. |
|
|
Significant invasion by the placenta was identified in the portion of the iliac vessels, mainly in the territory of the left iliac vein, requiring a joint approach with a vascular surgeon. |
|
|
Ligation of the anterior branch of the left iliac artery. |
Table 1: Order of the surgical and anesthetic procedure for the management of placenta accreta spectrum with iliac vessels invasion.
Despite all the measures, the patient presented with extreme blood loss, mainly due to the venous territory, until complete hemostasis was achieved. For this, hemostatic sutures, vascular ligatures, local compression, absorbable gelatin and biological glue were performed. Patient suffered blood loss of 22000 ml thus requiring massive transoperative transfusion of 14 units of red blood cells, 9 units of fresh plasma and 24 units of platelets. Ever since the patient's transfer to HCPA, she received, in total, 59 units of red blood cells, 13 units of fresh frozen plasma, 10 units of cryoprecipitates and 34 units platelets. The patient had 9.2 g/L of hemoglobin a day before surgery and then it lowered to 6.5 g/L during surgery. Afterwards, the patient was transferred to the Intensive Care Unit (ICU) where she immediately developed acute bilateral occlusion of the femoral artery. Urgently, bilateral femoral thrombectomy was performed without further occurrences. The patient remained in the ICU for 3 more days in which she presented good postoperative evolution. Diuresis of 1500 mL in the last 12 hours and received discharge from ICU with hemoglobin of 8.1 g/L. Patient was then transferred to the inpatient unit where she was observed for a while and discharged 9 days afterwards. During this postpartum stage, the patient’s surgical wound had a good aspect without a purulent discharge. Patient was walking and diuresis through the urinary catheter. Patient presented with a positive urine culture test in which she received treatment with sulfamethoxazole-trimipramine. The urinary catheter was removed at discharge from the inpatient unit and the patient was receiving 60 mg/day enoxaparin during her stay for thromboembolic prophylaxis.
The patient continued with frequent outpatient follow-up by an urologist, vascular surgeon and obstetrician. After 2 months, she presented discreet paresthesia in the left lower limb, without other sequelae. The newborn remained in the neonatal ICU, being discharged after 41 days without complications. The result of the histopathological examination of the placenta and uterus, showing placenta previa, percreta, adhered to the bladder and microscopic focal invasion of the detrusor muscle. Placental parenchyma showing infarcts and intervillous thrombi compromising about 10% of the specimen. Puerperal uterus showing adenomyosis. Chronic cervicitis with squamous metaplasia.
The approach for placenta accreta spectrum is divided into two different techniques, radical or conservative also known as expectants. The management is chosen depending on the level of experience from the excellence center and dependent on the complexity of the individual PAS case. Even though the conservative management allows patients to preserve their fertility, it is associated with long-term complications [9].
In a literature review of 119 cases of placenta percreta, 61% of those cases had partial or total placenta in situ postpartum, or partial resection of the accreta area, had at least one complication postoperative: Bleeding, infection and a higher risk of 50% for obtaining a hysterectomy in less than a year from the cesarean section [10]. With that being said, the radical approach (primary hysterectomy without trying to separate the placenta or delayed hysterectomy between the 3rd and the 12th week postpartum) continues to be the golden standard of management in PAS cases. With more than half of healthcare professionals choosing this radical management over the conservative [3].
The management of this case began with the correct diagnosis which was confirmed by experience professional in ultrasound imaging, as directed in the diagnosis and treatment of placenta accreta guidelines of the Royal College of Obstetricians and Gynecologists (RCOG), the International Federation of Gynecology and Obstetrics (FIGO) and Society of Obstetricians and Gynecologists of Canada (SOGC). As an alternative, MRI is not essential for the confirmation of PAS [3]. However, in such cases that the placenta is situated posteriorly in PAS cases, MRI is a helpful tool to visualize the extent of the invasion [11]. Our team decided that in order to have successful surgical planning, it was important to obtain magnetic resonance imaging to visualize the extent of invasion of the placenta accreta in areas that the ultrasound was difficult to evaluate. Studies show that early diagnoses of PAS are related to better maternal outcomes as compared to intraoperative diagnosis [12]. During the time that this case took place, literature review was conducted without finding the appropriate approach for placenta percreta with iliac vessel invasion. Thus, the decisions that took place were based on the knowledge of our healthcare specialists and on the extension of the placenta invasion.
The limitation that we are able to recognize in this particular case, involves intraoperative techniques of blood recovery. Even though we had access to a cell saver, we did not have healthcare specialists that were skillful to conduct this procedure, as if not performed correctly it can increase the risk of embolism in case that amniotic fluid is aspirated together with blood. A case study published in the United States, the referred hospital had access and an experienced professional to deal with this intraoperative technique, the cell saver. As well as with hemodilution, which probably contributed, in that case, to the minimal blood loss of about 400 ml [13]. In the case described, the use of the cell saver could have helped in the management of massive bleeding.
It is important to emphasize the various strengths involved in the reported case. It illustrates the need for a coordinated multidisciplinary team, including obstetrician, gynecologiconcologic surgeon, vascular surgeon, urologist, anesthetist, radiologist, intensivist, neonatologist and nurse, which is often found in tertiary care settings. Studies show that a multidisciplinary team used to dealing with these cases can lead to successful results [3]. In this case, the involvement of vascular surgeons in surgical planning and execution was essential for a good outcome. The patient evolved in the first postoperative hours with occlusion of the bilateral femoral artery. This is a relatively common complication in patients treated with endovascular occlusion strategies [14]. The planning of this hospital institution with a 24 hour shift by vascular surgeons allowed immediate re-intervention with bilateral thrombectomy, facilitating the postpartum woman's prompt recovery, which contributed as another strong point.
Our team at Hospital de Clinicas de Porto Alegre has experience in dealing with complex cases of placenta accreta spectrum disorders since 2015. To be considered a center of excellence in placenta accreta, it has most of the criteria suggested by Silver et al. [15]. Despite the large blood loss, surgical morbidity and bilateral thrombosis in the immediate postoperative period, the patient had an excellent recovery, being discharged in 9 days with less morbidity. We believe that the preoperative planning and the general experience of the team were fundamental for the success of this case.
In conclusion, this case report underscores the gravity of Placenta Accreta Spectrum (PAS) disorder, particularly emphasizing the challenges and successful management of a high-complexity case of placenta percreta adhering to multiple structures in a patient with three previous cesarean sections. The comprehensive management involved a multidisciplinary team and meticulous surgical planning, highlighting the significance of a center of excellence for PAS.
The case exemplifies the critical role of early diagnosis, enabled by experienced professionals and advanced imaging techniques such as MRI, in facilitating optimal surgical planning. Despite the rarity and complexity of placenta percreta with iliac vessel invasion, the decision-making process was guided by the expertise of the healthcare specialists and the extent of placental invasion.
While acknowledging limitations such as intraoperative blood recovery techniques, the report emphasizes strengths including the coordinated efforts of a multidisciplinary team and the prompt intervention by vascular surgeons, leading to a favorable outcome despite significant challenges.
The successful outcome of this case underscores the importance of specialized centers with expertise in managing PAS, as well as the necessity for ongoing research and refinement of management strategies. Overall, this report contributes to the growing body of knowledge aimed at improving outcomes for patients with PAS, reaffirming the critical role of multidisciplinary collaboration and meticulous surgical planning in ensuring maternal safety and wellbeing.
We would like to thank all healthcare professionals who were involved in the multidisciplinary team from the center of excellence for the management of Placenta Accreta (CEAPA/ HCPA) which was essential for the good maternal and fetal outcome that occurred.
None.
This case report did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
None declared.
Obtained.
Not commissioned; externally peer reviewed.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Azevedo R, Vettorazzib J, Salazar CC, Valeriob EG, Magnob V, Grudner MA, et al. (2024) Multidisciplinary Team Approach for Planceta Percreta with Iliac Vessel Invasion. Gynecol Obster. 14:632.
Received: 07-Oct-2023, Manuscript No. GOCR-23-27145; Editor assigned: 09-Oct-2023, Pre QC No. GOCR-23-27145 (PQ); Reviewed: 23-Oct-2023, QC No. GOCR-23-27145; Revised: 03-Dec-2024, Manuscript No. GOCR-23-27145 (R); Published: 10-Dec-2024 , DOI: 10.35248/2161-0932.24.14.632
Copyright: © 2024 Azevedo R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.