Journal of Depression and Anxiety
Open Access
ISSN: 2167-1044
ISSN: 2167-1044
Research Article - (2020)
Background: The COVID-19 crisis has become the largest crisis in modern times and has particularly impacted students due to school closures, prolonged social isolation, and anxieties related to their future and health. All these factors may have caused significant stress and led to anxiety and depression in students. The purpose of this study was to study the prevalence and severity of COVID-19 associated mental health morbidity in students in the United States (US).
Methods: A online cross-sectional survey was conducted using two instruments – the Perceived Stress Scale-4 (PSS-4) and the Patient Health Questionnaire for Depression and Anxiety-4 (PHQ-4). The survey was administered in the months of March to June during the COVID-19 pandemic to both high school and undergraduate college students.
Results: In total, 369 students agreed to participate: 51.8% were male, 44.1% were college students. An elevated perceived stress level (PSS- 4 > 8) and a positive mood disorder (PHQ-4 > 4) was present in 49.6% and 56.6% of respondents, respectively. The mean (SD) PSS scores in males and females were 6.7 (2.7) and 8.2 (2.9) respectively among all the respondents, while the mean (SD) PHQ scores in males and females were 3.7 (3.2) and 5.3 (3.2) respectively. Prevalence of anxiety and depression in the respondents was 35.0% and 36.3% respectively. Females students reported higher PSS and PHQ scores compared to male students. There is a significant correlation between PSS and PHQ (r=0.66)
Conclusion: The COVID-19 pandemic has resulted in an extremely high level of stress and mental health morbidity in both high school and college students, and this is more pronounced in females. Specific screening measures and interventions to improve the mental health of students is urgently warranted with a focus on females.
COVID-19; Stress; Anxiety; Depression; Students; Survey
The COVID-19 pandemic has been one of the worst healthcare and economic crises of modern times. In the US alone, there have been more than 2 million cases and over 100,000 deaths as of June 1, 2020 [1]. Mitigation efforts to contain the spread of the virus and limit the scope of this pandemic have led to an unprecedented level of physical distancing measures with nationwide lockdown and shelter in place. Due to this, schools and colleges have been forced to shut down and transition to emergency online learning formats, bringing disruptions to daily routines, prolonging social isolation, and increasing academic stressors for students. In addition, many students have also faced the loss of summer internships and cancellation of key standardized tests. Previous studies have shown that college students get adversely affected due to school closures from epidemics and as a result, experience compounded negative emotions [2]. These stressors are further accentuated by a backdrop of family uncertainty due to loss of income or jobs, looming uncertainty regarding the family’s financial future as well as potential health risks to family members, all of which would impact the normal coping strategies for students [3].
Given the impact of the situation, it is vital to analyze the psychological well-being of the students during the pandemic to develop measures and interventions adjusting to the situation. To our knowledge, no detailed study on the mental health well-being of students facing the COVID-19 outbreak has been published in the USA. The purpose of this study was to measure the impact of the COVID-19 pandemic on mental health (perceived stress, anxiety, and depression) of students in the USA.
Study setting and design
A cross-sectional study was undertaken between the months of March and June 2020 at the peak of the COVID-19 pandemic in the US.
A self-administered online questionnaire developed in an electronic format was widely distributed to college and school students via social media and direct networks. All records were kept anonymous and did not involve divulging any personally identifiable information such as their name, age, or school. Study was exempt from IRB as it only involved collection from online of anonymous data.
Data collection and procedure
An online link was sent to all study participants. The online link consisted of an electronic consent form and a basic sociodemographic information sheet. After consenting to participate, participants were redirected to a secure page to complete the questionnaire. The survey took approximately one minute to complete.
For this study, we administered the Perceived Stress Scale (PSS- 4) and the Patient Health Questionnaire for Depression and Anxiety (PHQ-4). The Perceived Stress Scale (PSS-4) is a self-report questionnaire developed by Cohen et al. to measure a person’s evaluation of stressful situations in the previous 1 month of his or her life [4]. It is a global measure of stress that is easy to use, has been well studied in multiple settings as well as in different languages, and found to have strong reliability and validity measures [4–6]. The full instrument contains 14 statements that measure the respondent's perception of stress on a 5-point Likert scale. It consists of both negative elements - intended to assess the lack of control and negative affective reactions, as well as positive elements - intended to measure the degree of ability to cope with existing stressors. The PSS-4 is a short form scale containing four items from the original scale (items 2, 6, 7, and 14) and has been shown to also have good reliability and validity [7,8]. PSS-4 score ranges from 0-16 (low to high), with higher scores equating to higher stress. In this study, we have categorized the severity of stress level as normal (0-7), mild (8-10), moderate (11-12), and severe (13- 16) based on the PSS-4 scores.
The PHQ-4 is a valid ultra-brief tool for detecting both anxiety and depressive disorders, and studies have confirmed its reliability and validity as a measure of depression and anxiety in the general population in the last two weeks [9,10]. PHQ-4 is a 4-item inventory rated on a four-point Likert scale. A score of 3 or greater on the anxiety subscale (Questions 1 and 2) and depression subscale (Questions 3 and 4) has been identified asis a cut-off to identify potential presence of anxiety and depression, respectively. The severity is categorized as normal (0-2), mild (3-5). Moderate (6-8) and severe (9-12) based on the overall PHQ-4 scores.
Data collection and procedure
An online link was sent to all study participants. The online link consisted of an electronic consent form and a basic sociodemographic information sheet. After consenting to participate, participants were redirected to a secure page to complete the questionnaire. The survey took approximately one minute to complete.
Data analysis
All the analysis was performed in SPSS 22.0. Descriptive analysis was completed, frequencies and percentages were computed for categorical variables, and mean (M) and standard deviation (SD) were calculated for continuous variables. Univariate analysis (Mann Whitney test and Kruskal Wallis test) was used to explore the significant associations between the respondents and the stress, anxiety, and depression level. Pearson correlation coefficient, r, was used to evaluate the association between PSS-4 and PHQ-4. A twotailed p-value of < 0.05 was considered statistically significant. All the analysis was performed in SPSS 22.0.
A total of 369 (191 Male; 177 Female) students completed the questionnaire, with their grade distribution and location shown in Table 1. Individual mean scores and the percentage of PSS-4 and PHQ-4 among the respondents segmented by gender and grades are reported in Figures 1 and 2 and Tables 2 and 3. Overall 49% of the respondents had an abnormal PSS score and 68% had an abnormal PHQ4 score. (Figure 3). Females had consistently higher elevated stress levels and mood disorder depression/anxiety than males (Figure 4). Severity levels of perceived stress and anxiety/ depression among the students is presented in Figure 4. About 34% of respondents had moderate to severe anxiety/depression in PHQ, and 13% reported moderate to severe stress in PSS (Figure 4). High school and college students had similar levels of stress as well as anxiety and depression (Figure 5 and Table 3). There is a significant gender influence in both PSS and PHQ scores (Tables 2 and 3). Univariate ordinal regression analysis of the severity of PHQ-4 and PSS-4 is reported in Tables 4 and 5. Gender and the location of the respondents are significantly associated with the severity of PHQ-4 and PSS-4. Female respondents and students from California had higher stress and anxiety/depression scores compared to males and other states of the US. This is found to be statistically significant (Tables 4 and 5). There was a strong correlation between PSS scores and PHQ scores both overall (r = 0.66) as well as in individual questions (Table 6).
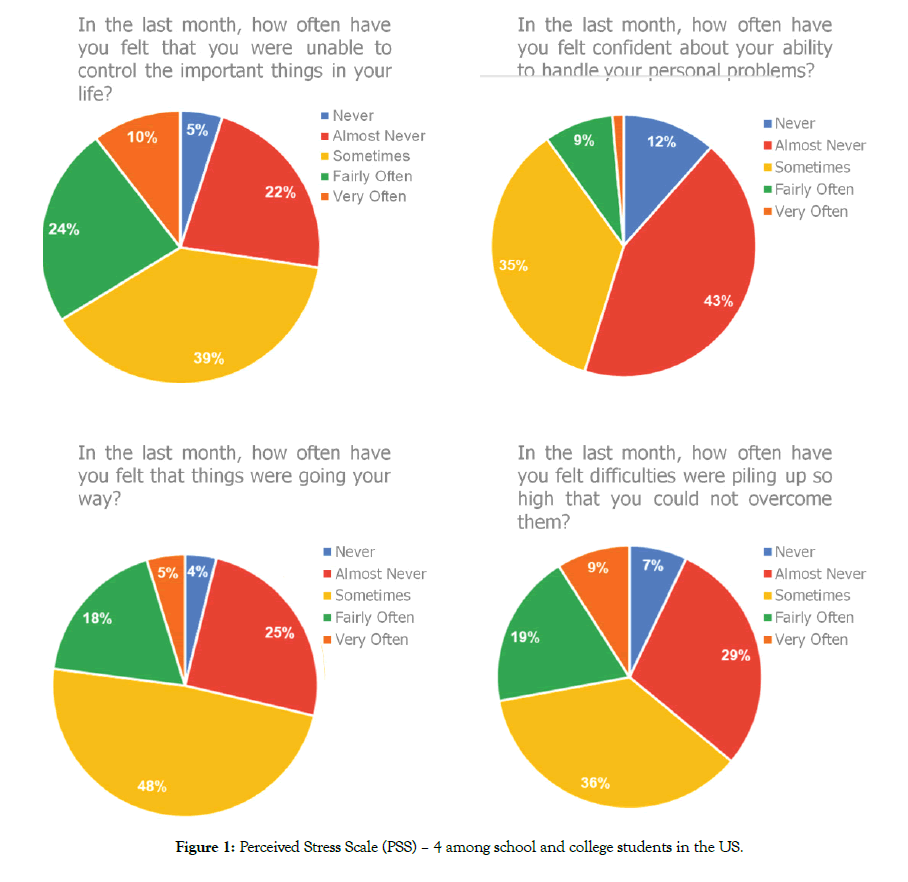
Figure 1: Perceived Stress Scale (PSS) – 4 among school and college students in the US.
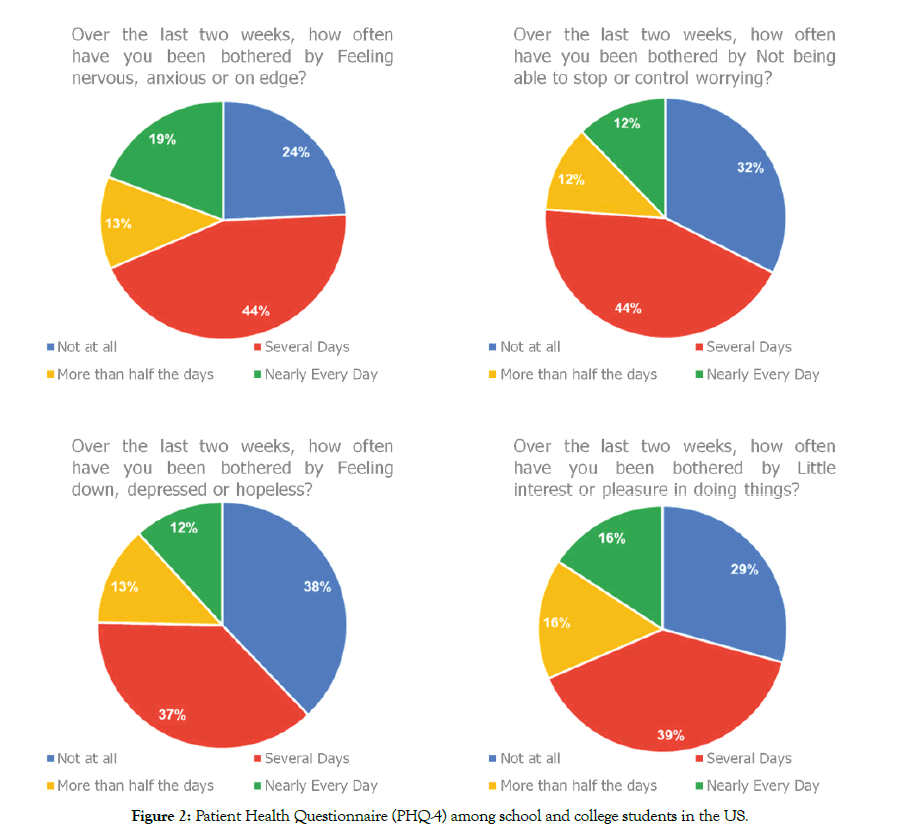
Figure 2: Patient Health Questionnaire (PHQ-4) among school and college students in the US.
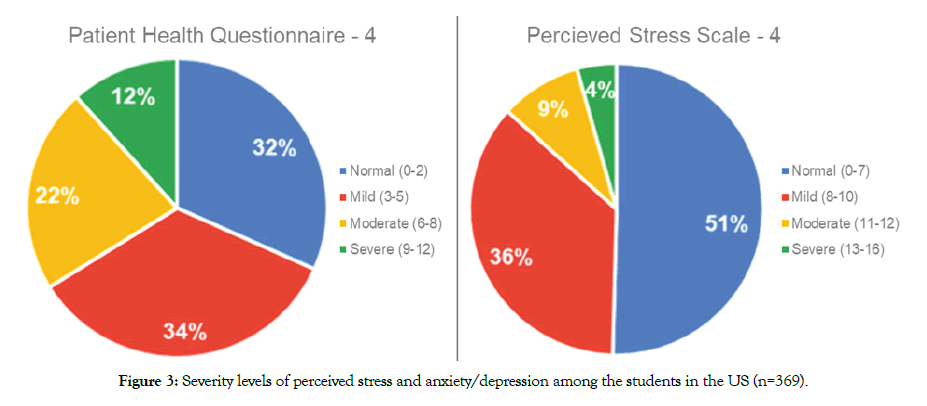
Figure 3: Severity levels of perceived stress and anxiety/depression among the students in the US (n=369).
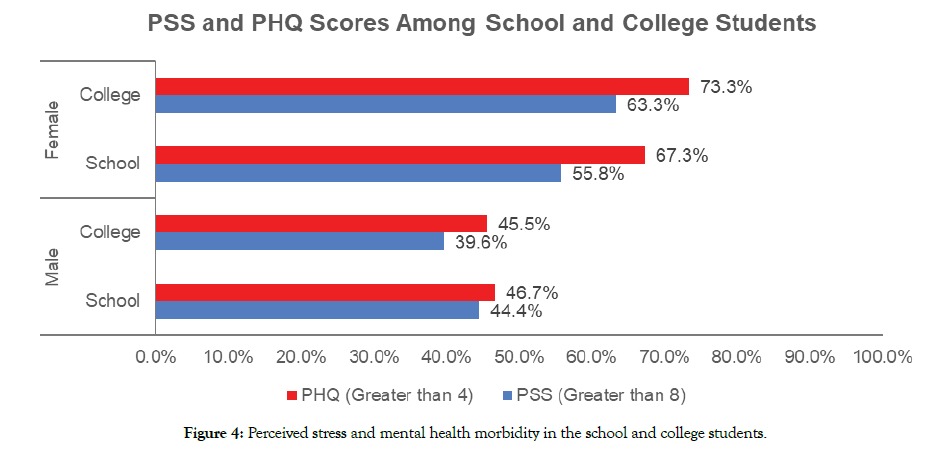
Figure 4: Perceived stress and mental health morbidity in the school and college students.
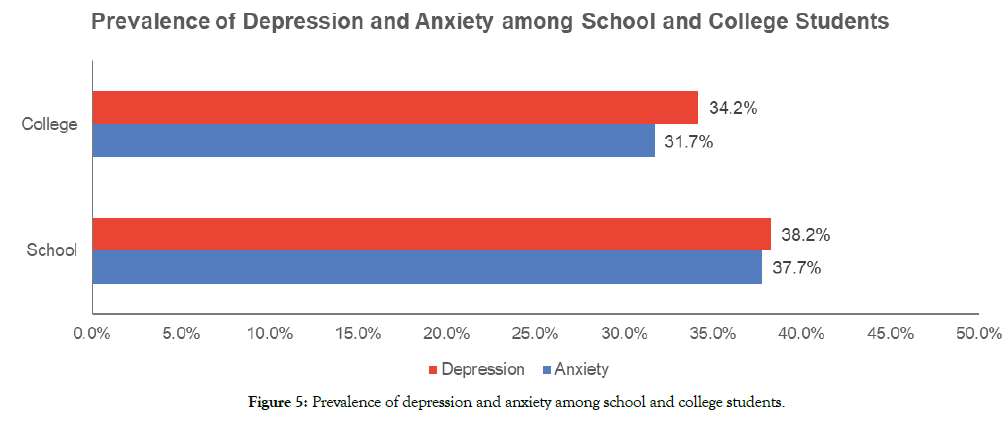
Figure 5: Prevalence of depression and anxiety among school and college students.
Table 1: Socio-demographic characteristics of the study participants.
| Variables | Frequency (n=369) | Percent |
|---|---|---|
| Gender | ||
| Female | 177 | 48.0 |
| Male | 191 | 51.8 |
| Education Grade | ||
| College Year 1-2 | 123 | 33.7 |
| College Year 3-4 | 38 | 10.4 |
| High School Grades 11-12 | 158 | 43.3 |
| High school Grades 9-10 | 46 | 12.6 |
| Location | ||
| Texas | 101 | 27.4 |
| California | 127 | 34.4 |
| Florida | 17 | 4.6 |
| Northeast US | 54 | 14.6 |
| Mid-West | 9 | 2.4 |
| Other US States | 16 | 4.3 |
| Not Available | 45 | 12.2 |
Table 2: Descriptive statistics of anxiety, depression, and stress using PSS and PHQ in male and female students (n=369).
| Anxiety and Depression scores using PSS and PHQ | Mean ± SD | P-value | |
|---|---|---|---|
| Male | Female | ||
| PSS* (Total) | 6.74±2.68 | 8.18±2.93 | 0.000 |
| PSS-Q1* (Unable to control the important things in your life?) | 1.91±0.97 | 2.34±1.04 | |
| PSS-Q2* (Confident about your ability to handle your personal problems?) | 1.35±0.84 | 1.56±0.86 | |
| PSS-Q3* (Things were going your way?) | 1.78±0.84 | 2.13±0.88 | |
| PSS-Q4* (Difficulties were piling up so high that you could not overcome them?) | 1.72±1.02 | 2.17±1.05 | |
| PHQ 4** (Total) | 3.68±3.18 | 5.29±3.17 | 0.000 |
| PHQ-Q1** (Feeling nervous, anxious or on edge?) | 1.05±0.98 | 1.49±1.04 | |
| PHQ-Q2** (Not being able to stop or control worrying?) | 0.80±0.87 | 1.29±1.00 | |
| PHQ-Q3** (Feeling down, depressed, or hopeless?) | 0.79±0.95 | 1.20±0.99 | |
| PHQ-Q4** (Little interest or pleasure in doing things?) | 1.05±1.04 | 1.32±0.99 | |
| PHQ (Anxiety and Depression) | |||
| PHQ-Q1 and Q2 (Anxiety) | 1.84±1.71 | 2.78±1.87 | 0.000 |
| PHQ-Q3 and Q4 (Depression) | 1.83±1.75 | 2.51±1.69 | 0.000 |
PSS: Perceived Stress Scale; PHQ: patient health questionnaire; p-value (Student t-test)
*In the last month, how often have you felt that you were
**Over the last two weeks, how often have you been bothered by
Table 3: Descriptive statistics of anxiety, depression, and stress using PSS and PHQ in school students vs. college students (n=369).
| Anxiety and Depression scores using PSS and PHQ | School | College | P-value |
|---|---|---|---|
| Mean ± SD | |||
| PSS* (Total) | 7.61±2.99 | 7.19±2.77 | 0.137 |
| PSS-Q1* (Unable to control the important things in your life?) | 2.10±1.05 | 2.14±1.01 | |
| PSS-Q2* (Confident about your ability to handle your personal problems?) | 1.51±0.90 | 1.37±0.79 | |
| PSS-Q3* (Things were going your way?) | 2.01±0.91 | 1.88±0.83 | |
| PSS-Q4* (Difficulties were piling up so high that you could not overcome them?) | 2.01±1.07 | 1.83±1.04 | |
| PHQ-4** (Total) | 4.54±3.21 | 4.36±3.38 | 0.645 |
| PHQ-Q1** (Feeling nervous, anxious or on edge?) | 1.26±1.06 | 1.26±1.01 | |
| PHQ-Q2** (Not being able to stop or control worrying?) | 1.03±0.94 | 1.04±1.01 | |
| PHQ-Q3** (Feeling down, depressed, or hopeless?) | 1.00±0.99 | 0.96±0.99 | |
| PHQ-Q4** (Little interest or pleasure in doing things?) | 1.24±1.02 | 1.12±1.04 | |
| PHQ (Anxiety and Depression) | |||
| PHQ-Q1 and Q2 (Anxiety) | 2.30±1.83 | 2.29±1.88 | 0.980 |
| PHQ-Q3 and Q4 (Depression) | 2.24±1.72 | 2.07±1.80 | 0.406 |
PSS: Perceived Stress Scale; PHQ: Patient Health Questionnaire; p-value (Student t-test)
*In the last month, how often have you felt that you were
**Over the last two weeks, how often have you been bothered by
Table 4: Socio-demographic characteristics of study participants and the PHQ – 4 severities.
| Variables | PHQ - 4 (Severity) | P-value | ||||
|---|---|---|---|---|---|---|
| Normal (n=117) |
Mild (n=127) |
Moderate (n=82) |
Severe (n=117) |
Total (n=369) | ||
| Gender | 0.000a | |||||
| Female | 37 (31.6%) | 58 (43.2%) | 56 (68.8%) | 26 (58.5%) | 177 (48.0%) | |
| Male | 79 (67.5%) | 69 (54.3%) | 26 (31.7%) | 17 (39.5%) | 191 (51.8%) | |
| Education | 0.471a | |||||
| High School | 62 (53.0%) | 67 (52.8%) | 51 (62.2%) | 24 (55.8%) | 204 (55.3%) | |
| College | 53 (45.3%) | 59 (46.5%) | 30 (36.6%) | 19 (44.2%) | 161 (43.6%) | |
| Normal (n=91) |
Mild (n=87) |
Moderate (n=62) |
Severe (n=30) |
Total (n=282) | ||
| Location | 0.003b | |||||
| Texas | 29 (31.5%) | 36 (38.3%) | 23 (35.9%) | 13 (40.6%) | 101 (35.8%) | |
| California | 54 (58.7%) | 40 (42.6%) | 20 (31.3%) | 13 (40.6%) | 127 (45.0%) | |
| Northeast US | 9 (9.8%) | 18 (19.1%) | 21 (32.8%) | 6 (18.8%) | 54 (19.1%) | |
PHQ: Patient Health Questionnaire
a: Mann-Whitney U Test
b: Kruskal-Wallis Test
Table 5: Socio-demographic characteristics of study participants and the PSS – 4 severities.
| Variables | PSS - 4 | P-value | ||||
|---|---|---|---|---|---|---|
| Normal (n=186) |
Mild (n=134) |
Moderate (n=33) |
Severe (n=16) |
Total (n=369) | ||
| Gender | 0.000a | |||||
| Female | 74 (39.8%) | 66 (49.3%) | 24 (72.7%) | 13 (81.3%) | 177 (48.0%) | - |
| Male | 111 (59.7%) | 68 (50.7%) | 9 (27.3%) | 3 (18.8%) | 191 (51.8%) | - |
| Education | 0.197a | |||||
| High School | 101 (54.3%) | 71 (53.0%) | 18 (54.5%) | 14 (87.5%) | 204 (55.3%) | - |
| College | 83 (44.6%) | 62 (46.3%) | 14 (42.4%) | 2 (12.5%) | 161 (43.6%) | - |
| Normal (n=153) |
Mild (n=92) |
Moderate (n=27) |
Severe (n=10) |
Total (n=282) | ||
| Location | 0.044b | |||||
| Texas | 53 (34.6%) | 33 (35.9%) | 13 (48.1%) | 2 (20.0%) | 101 (35.8%) | - |
| California | 78 (51.0%) | 35 (38.0%) | 9 (33.3%) | 5 (50.0%) | 127 (45.0%) | - |
| Northeast US | 22 (14.4%) | 24 (26.1%) | 5 (18.5%) | 3 (30.0%) | 54 (19.1%) | -- |
PSS: Perceived Stress Scale
a: Mann-Whitney U Test
b: Kruskal-Wallis Test
Table 6: Correlation analysis between the total scores of PSS and PHQ in the study population.
| Perceived Stress Scale (PSS) | PHQ-4 (Total) | |
|---|---|---|
| r-valye | P-value | |
| PSS-Q1 | 0.527 | 0.000 |
| PSS-Q2 | 0.425 | 0.000 |
| PSS-Q3 | 0.358 | 0.000 |
| PSS-Q4 | 0.632 | 0.000 |
| Total PSS | 0.656 | 0.000 |
PSS: Perceived Stress Scale; PHQ: Patient Health Questionnaire; r – Pearson Correlation Coefficient
Our study points to a high prevalence of stresses as well as anxiety and depression among students. We especially note that female students seem to be more severely impacted and that high school students have higher levels of stress and anxiety compared to college students.
Public health emergencies can affect the psychosocial wellbeing of the students, and it reflects in the form of stress, anxiety, and depression. Since the start of the COVID-19 pandemic, there have been few studies that have already examined the impact of COVID-19 on mental health in different student populations. Cao et al. administered a 7-item Generalized Anxiety Disorder Scale (GAD-7) on 7,143 college students in China. They found 24.9% of the respondents had anxiety of which only 2.7% was considered moderate and 0.9% was severe [11]. In our study, the prevalence of anxiety/depression (PHQ) was higher at 68% and what was strikingly different was our study group showed a prevalence of severe anxiety (PHQ- Questions 1 & 2 anxiety ≥ 3) of 34% compared to only 0.9% in their group. Also, interestingly their study did not show any gender differences, while in our study we found marked gender differences with females having higher levels of anxiety than males. We speculate that these differences may be related to cultural differences since their study was based in China and ours was in the USA. Their study found college students' anxiety regarding the epidemic was associated with their place of residence, source of parental income, whether living with parents, and whether a relative or an acquaintance was infected with COVID-19. It will be interesting to explore these factors in future studies in US students to see if they are different. The authors suggested that the mental health of college students should be monitored during epidemics. Another report from Greece [12] used an online survey on 1,000 university students and reported a ‘horizontal’ increase in scores by 42.5% for anxiety, 74.3% for depression, and 63.3% increase in total suicidal thoughts when compared to the general population. Since this was a brief report, more details of their methodology and findings are missing. A Spanish study assessed the psychological impact of COVID-19 in a university community using a Depression Anxiety Stress Scale (DASS-21) to assess symptoms of depression, anxiety and stress and found moderate to extremely severe scores of anxiety, depression, and stress in 21.34%, 34.19% and 28.14% of the respondents, respectively [13]. In our study, the prevalence of anxiety (PHQ-Anxiety ≥3), depression (PHQ-Depression ≥3) and stress (PSS>8) was 31.7%, 34.2% and 48.4% among the college students, Anxiety and stress levels were slightly higher in our study than the Spanish study, while the depression levels are similar. This high prevalence among college students could be due to the Spanish study being conducted in one University whereas our participants are in various universities across the US. Another study from China administered the Kessler 6-item Psychological Distress Scale (K6) and the Impact of Event Scale-Revised (IES-R) to 1,442 health professional students [14]. They found that 26.63% of participants demonstrated clinically significant psychological distress, while 11.10% met the criterion for a probable Acute Stress Reaction. This study did not include any questionnaires related to anxiety or depression. In another study from China in 2,485 participants from 6 universities, using the PTSD Checklist Civilian Version and PHQ-9, the prevalence of PTSD and depression was found to be 2.7% and 9.0% respectively. The most significant risk factor for psychological distress was subjectively feeling extreme fear. These numbers are a lot lower for both stress and depression than the findings from our group and may reflect regional and ethnic differences as well as possible differences in severity of the social disruption.
Our study is the first report in the USA and to our knowledge the first study that incorporates both stresses as well as anxiety/ depression among both high school as well as college students. Experts have already warned about the particular vulnerability of adolescents for mental health problems brought on by COVID-19 [15-17]. One review opined that COVID-19-associated mental health risks will disproportionately affect children and adolescents who are already disadvantaged and marginalized. Research is needed to assess the implications of policies enacted to contain the pandemic on the mental health of children and adolescents, and to estimate the risk/benefit ratio of measures, such as homeschooling, to be better prepared for future developments [17].
The higher incidence of anxiety and stress in college students in our survey may be a consequence of the high prevalence of mental health problems in college students as they transition to young adulthood [18,19]. College students have been known to harbor a high burden of mental health problems even at baseline – one study showed high rates of self-reported psychiatric symptoms and diagnoses especially among ethnic minority groups [20]. Liu et al. found in their study a high rate of multiple stress exposures among the U.S. college population and advocated for an urgent need for service utilization strategies, given the high impacts of stress on mental health and suicidality.
Gender differences have previously been seen in stress-related to COVID-19 in a study by Liu et al. in China [21]. They found that the prevalence of post-traumatic stress syndrome a month after the COVID-19 outbreak was 7% in the hardest-hit areas and that women were more significantly impacted in the domains of reexperiencing negative alterations in cognition or mood, and hyperarousal.
Numerous factors may be contributing to mental health problems in students during the COVID-19 epidemic. These may include social isolation and loneliness [22], fear and helplessness related to the disease as well as lack of sleep [23,24], as this pandemic prompted all the countries to opt for confinement or physical distancing. Also, the overwhelming and sensational news headlines, travel restrictions, inability to meet loved ones, fear of career progression, or academics may have added to anxiety, depression, and high stress among the students Similar results have also been seen in earlier pandemics such as the severe acute respiratory syndrome (SARS) epidemic. In one study of 381 students in China during SARS, significant mental health burdens in students were found and additionally, that the number of stressors and use of avoidant coping strategies positively predicted psychological symptoms [25].
We found regional variation in levels of stress in our survey with California students being particularly more affected. We speculate this may be due to California being one of the first states to get affected and may be a consequence of potentially more stringent lockdown measures. It could also be reflective of regional differences in baseline levels of stress and anxiety across the US.
There are a few limitations to our study. Firstly, this is a crosssectional study carried out under an unprecedented and rapidly developing situation. Secondly, our study samples were small relative to other studies, but we believe that this was a representative sample from different regions of the US. Thirdly, this was an internet-based survey using social media and given the anonymous nature of the survey we were unable to verify the identity or veracity of the respondents and this might have contributed to some bias in the study findings.
Despite this, our study provides a pivotal early glimpse of the glaring degree of mental health morbidity in US students in both high school and college due to the COVID-19 pandemic and the resultant national lockdown and points to an urgent need for more attention and intervention in this vulnerable and critical demographic.
In summary, our study is an important addition to the growing body of literature that sheds light on the growing mental health crisis amongst high school and college students in the US. This study suggests that psychological wellbeing and mental health should be carefully monitored during the pandemic, and educational institutions should provide psychological support for adapting to these circumstances. Also, it is important to explore why younger school students are suffering a greater psychological impact in future studies.
Nil.
AA and SS analyzed and interpreted the participant's data. AA, YG, ZS and RI administered the study tool, and AA ZS and SS were a major contributor in writing the manuscript. All authors read and approved the final manuscript.
This protocol was submitted to Solutions IRB for a survey on healthcare workers and declared to be IRB exempt - Protocol #2020/05/7 verified as Exempt according to 45 CFR-46.104(d)(2): (2) Tests, Surveys, Interviews and this protocol has been followed in this study.
Informed consent was obtained from all students voluntarily completed the survey and the collection was anonymous with no identifying information.
All authors have given their consent for publication.
The authors declare that they have no competing interests.
Citation: Aiyer A, Surani S, Gill Y, Iyer R, Surani Z (2020) Mental Health Impact of Covid-19 on Students in the USA: A Cross-Sectional Web-Based Survey. J Depress Anxiety. 9:375. doi: 10.35248/2167-1044.20.9.375.
Received: 14-Oct-2020 Accepted: 03-Nov-2020 Published: 10-Nov-2020
Copyright: © 2020 Aiyer A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.