Journal of Depression and Anxiety
Open Access
ISSN: 2167-1044
ISSN: 2167-1044
Research - (2020)Volume 9, Issue 4
The COVID-19 crisis has become the largest crisis in modern times and particularly impacted healthcare workers (HCW) leading to extreme stress due to risk of exposure and health concerns. A web-based survey was conducted using two instruments – the Perceived Stress Scale-4 (PSS-4) and the Patient Health Questionnaire for Depression and Anxiety-4 (PHQ-4). The survey was administered in the months of March to June during the COVID-19 pandemic to both doctors (MD) and nurses (RN). A total of 569 HCWs completed the questionnaire (50% RNs and 30% MDs). About 42% HCWs screened positive for a mood disorder depression/anxiety based on PHQ-4 of >4, and 49% respondents had an elevated stress level (PSS-4 of >8). A significant gender influence was seen; 69% of HCWs in the high-stress group were female, as compared to 29% males. Gender influence in both PSS-4 and PHQ-4 was found to be statistically significant (p<0.001). Significantly higher PHQ-4 and PSS-4 scores were found in RNs compared to MDs. There was a strong correlation between PSS and PHQ scores (r = 0.705). The COVID-19 pandemic has resulted in an extremely high level of stress and mental health morbidity, especially among nurses and females.
COVID-19; Stress; Anxiety; Depression; Healthcare workers
A novel strain of coronavirus was found in December 2019 in Wuhan, China [1,2]. The World Health Organization (WHO) declared COVID-19 a global pandemic on March 12, 2020 [3]. The COVID-19 pandemic has become one of the worst healthcare and economic crises of modern times. As of July 12, 2020, COVID-19 was responsible for 133,486 deaths of the 3.16 million confirmed cases in the US [4].
In the past, such viral outbreaks have been shown to result in significant levels of stress in healthcare workers (HCW). The COVID-19 pandemic has introduced multiple stressors for HCWs. The rapid surge in cases in many places rapidly depleted resources including ICU beds and ventilators and rapidly depleted personal protective equipment (PPE) [5] . This meant HCWs faced heavy workloads in extremely stressful conditions while at the same time lacking in resources to care patients and facing a high risk of exposure to the virus, thereby potentially putting in jeopardy both their own health and lives, as well as those of their families. Added to this was uncertainty with regards to their financial future, as well as the health of their families. Early data from China confirmed the presence of significant mental health morbidity in HCWs in the early stages of the COVID-19 pandemic [6,7] To our knowledge, little is known about this pandemic’s mental health impact on the of HCWs in the USA. Given the impact of the situation, it is vital to measure and analyze the psychological well-being of different HCWs during the pandemic to develop measures and interventions to address the situation. This cross-sectional study measured the impact of the COVID-19 pandemic on mental health (perceived stress, anxiety, and depression) of HCWs in the USA.
Study setting and design
A cross-sectional study was undertaken between March and June 2020 at the peak of the COVID-19 pandemic in the USA. To minimize the face-to-face interaction and to comply with physical distancing restrictions, we developed a self-administered online questionnaire in an electronic format that was widely distributed to health care workers via social media (including, Facebook, Twitter, and LinkedIn) and direct virtual contact. All records were kept anonymous and did not involve divulging any personally identifiable information such as name, age, or hospital/clinic. We collected information about the gender, profession, and state of domicile in the online form. Protocol was submitted to IRB and exempt status was obtained.
Study instrument
For this study, we administered the Perceived Stress Scale (PSS-4) and the Patient Health Questionnaire for Depression and Anxiety (PHQ-4). The Perceived Stress Scale is a self-report questionnaire developed by Cohen et al. to measure a person’s evaluation of stressful situations in the previous one month of his or her life [8]. It is a global measure of stress that is easy to use, has been well studied in multiple settings as well as in different languages, and has been found to have strong reliability and validity measures [8–10]. The full instrument contains 14 statements that measure the respondent's perception of stress on a 5-point Likert scale. It consists of both negative elements - intended to assess the lack of control and negative affective reactions, as well as positive elements – intended to measure the degree of ability to cope with existing stressors. The PSS-4 is a short form scale containing four items from the original scale (items 2, 6, 7, and 14) and has been shown to also have good reliability and validity [11,12]. PSS-4 score ranges from 0-16 (low to high), with higher scores equating to higher stress. In this study, we have categorized the severity of stress level as normal (0-7), mild (8-10), moderate (11-12), and severe (13-16) based on the PSS-4 scores.
The PHQ-4 is a valid ultra-brief tool for detecting both anxiety and depressive disorders, and studies have confirmed its reliability and validity as a measure of depression and anxiety in the general population [13,14]. PHQ-4 is a 4-item inventory rated on a fourpoint Likert scale. A score of 3 or greater on the anxiety subscale (Questions 1 and 2) and depression subscale (Questions 3 and 4) has been identified as a cut-off to identify the potential presence of anxiety and depression, respectively. The severity is categorized as normal (0-2), mild (3-5). Moderate (6-8) and severe (9-12) based on the overall PHQ-4 scores.
Data collection and procedure
An online link was sent to all study participants. The online link consisted of an electronic consent form and a basic sociodemographic information sheet. After consenting to participate, participants were redirected to a secure page to complete the questionnaire. The survey took approximately one minute to complete.
Data analysis
All the collected data was organized in an Excel spreadsheet. All the data was quality-checked by a researcher to ensure accuracy and completeness. Analysis was performed in SPSS 22.0. Descriptive analysis was summarized as frequencies and percentages for categorical variables, and mean (M) and standard deviation (SD) were calculated for continuous variables. χ2 tests were used to compare group differences of categorical variables. The Mann Whitney and Kruskal Wallis tests were used to compare the respondents on abnormally distributed stress, anxiety, and depression scores. The Pearson correlation coefficient, r, was used to evaluate the association between PSS-4 and PHQ-4. A two-tailed p-value of < 0.05 was considered statistically significant.
A total of 569 health care workers completed the questionnaire. Demographic distribution and characteristics of the respondents are shown in Table 1. The majority (51.7%) of the respondents were in the age group of 41-60 years and 80.1% were women. The participants included registered nurses (50.03%), physicians (30.2%), medical & nursing assistants (5.4%), respiratory therapists (5.4%), and others (8.6%). Among the respondents, the majority were Caucasians (46.6%) and more than half of the respondents (53.8%) were from Texas.
| Variables | Frequency (n=569) | Percent |
|---|---|---|
| Gender | ||
| Female | 456 | 80.1 |
| Male | 103 | 18.1 |
| Not Available | 10 | 1.8 |
| Age Group | ||
| 20-40 Years | 237 | 41.7 |
| 41-60 Years | 294 | 51.7 |
| >60 Years | 36 | 6.3 |
| Not Available | 2 | 0.4 |
| Occupation | ||
| Medical and Nursing Assistants (CNA & MA) | 31 | 5.4 |
| Physicians (MD) | 172 | 30.2 |
| Registered Nurse (RN) | 286 | 50.3 |
| Respiratory Therapists | 31 | 5.4 |
| NP | 1 | 0.2 |
| Not Available | 48 | 8.4 |
| Race | ||
| Afro Americans | 10 | 1.8 |
| Caucasians | 265 | 46.6 |
| Asians | 72 | 12.7 |
| South Asians | 45 | 7.9 |
| Hispanic | 154 | 27.1 |
| Unknown | 23 | 4.0 |
| Location | ||
| California | 48 | 8.5 |
| Texas | 306 | 53.8 |
| Northeast US | 41 | 7.2 |
| Others/NA | 174 | 30.6 |
Table 1: Socio-demographic characteristics of the study participants.
Individual mean scores and the percentage of PSS-4 and PHQ-4 among the respondents segmented by gender and occupation are reported in Tables 2 and 3. The mean (SD) of PSS-4 scores among men and women was 5.62 (3.15) and 7.38 (2.98) respectively while the mean (SD) of PHQ-4 scores among men and women were 2.88 (2.61) and 5.06 (3.35). The difference in the mean values of PSS-4 and PHQ-4 among men and women was found to be statistically significant (p<0.001) (Table 2). The proportion of study participants with different ratings in the PSS-4 and PHQ-4 was reported in Figures 1 and 2.
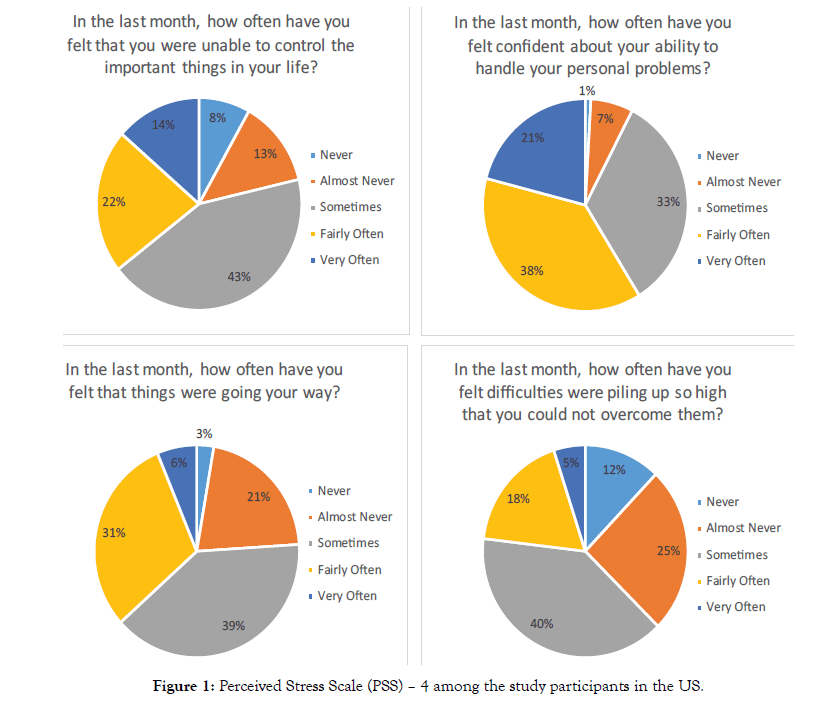
Figure 1: Perceived Stress Scale (PSS) – 4 among the study participants in the US.
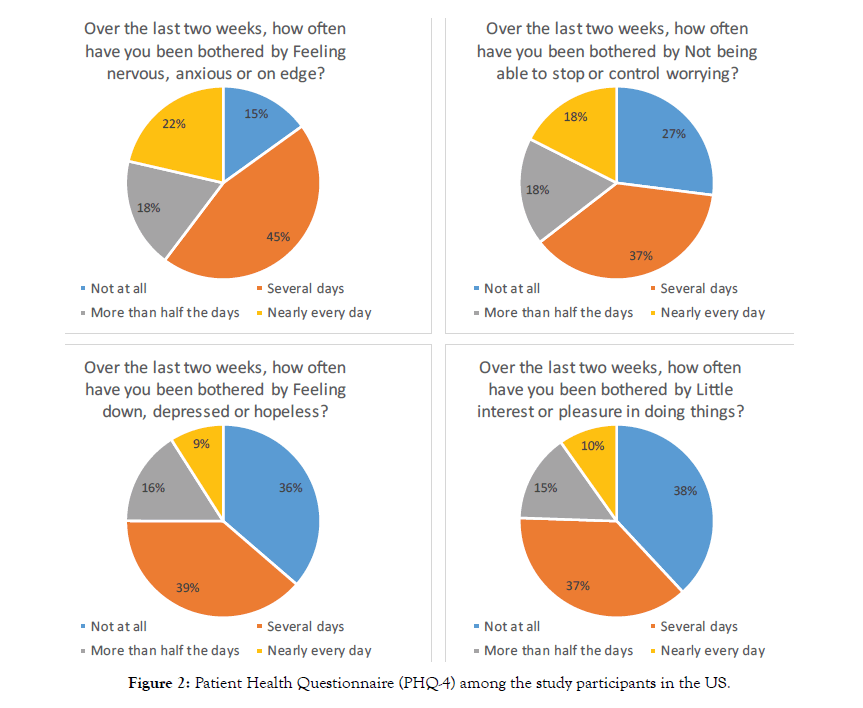
Figure 2: Patient Health Questionnaire (PHQ-4) among the study participants in the US.
| Anxiety and Depression scores using PSS and PHQ | Mean ± SD | P-Value | |
|---|---|---|---|
| Male | Female | ||
| PSS* (Total) | 5.62 ± 3.15 | 7.38 ± 2.98 | 0.000 |
| PSS-Q1* (Unable to control the important things in your life?) | 1.75 ± 1.19 | 2.28 ± 1.04 | |
| PSS-Q2* (Confident about your ability to handle your personal problems?) | 1.10 ± 0.90 | 1.33 ± 0.90 | |
| PSS-Q3* (Things were going your way?) | 1.48 ± 0.97 | 1.90 ± 0.89 | |
| PSS-Q4* (Difficulties were piling up so high that you could not overcome them?) | 1.30 ± 0.98 | 1.88 ± 1.02 | |
| PHQ 4** (Total) | 2.88 ± 2.61 | 5.06 ± 3.35 | 0.000 |
| PHQ-Q1** (Feeling nervous, anxious or on edge?) | 0.96 ± 0.89 | 1.56 ± 0.98 | |
| PHQ-Q2** (Not being able to stop or controlworrying?) | 0.70 ± 0.84 | 1.38 ± 1.04 | |
| PHQ-Q3** (Feeling down, depressed or hopeless?) | 0.54 ± 0.71 | 1.07 ± 0.96 | |
| PHQ-Q4** (Little interest or pleasure in doing things?) | 0.60 ± 0.84 | 1.03 ± 0.97 | |
| PHQ (Anxiety and Depression) | |||
| PHQ-Q1 and Q2 (Anxiety) | 1.66 ± 1.58 | 2.94 ± 1.91 | 0.000 |
| PHQ-Q3 and Q4 (Depression) | 1.16 ± 1.42 | 2.10 ± 1.79 | 0.000 |
PSS: Perceived Stress Scale; PHQ: patient health questionnaire; p-value (Student t-test)
*In the last month, how often have you felt that you were
**Over the last two weeks, how often have you been bothered by
Table 2: Descriptive statistics of anxiety, depression, and stress using PSS and PHQ in male and female participants (n=569).
| Anxiety and Depression scores using PSS and PHQ | Mean ± SD | P-Value | ||
|---|---|---|---|---|
| MD | SN | |||
| PSS* (Total) | 6.89 ± 2.78 | 7.21 ± 3.12 | 0.274 | |
| PSS-Q1* (Unable to control the important things in your life?) | 2.24 ± 1.02 | 2.19 ± 1.07 | - | |
| PSS-Q2* (Confident about your ability to handle your personal problems?) | 1.27 ± 0.85 | 1.33 ± 0.90 | - | |
| PSS-Q3* (Things were going your way?) | 1.77 ± 0.83 | 1.87 ± 0.91 | - | |
| PSS-Q4* (Difficulties were piling up so high that you could not overcome them?) | 1.55 ± 1.03 | 1.87 ± 1.01 | - | |
| PHQ-4** (Total) | 4.08 ± 2.97 | 5.04 ± 3.44 | 0.003 | |
| PHQ-Q1** (Feeling nervous, anxious or on edge?) | 1.34 ± 0.91 | 1.56 ± 1.04 | - | |
| PHQ-Q2** (Not being able to stop or controlworrying?) | 1.12 ± 0.97 | 1.35 ± 1.10 | - | |
| PHQ-Q3** (Feeling down, depressed or hopeless?) | 0.79 ± 0.87 | 1.08 ± 0.93 | - | |
| PHQ-Q4** (Little interest or pleasure in doing things?) | 0.76 ± 0.83 | 1.04 ± 0.97 | - | |
| PHQ (Anxiety and Depression) | ||||
| PHQ-Q1 and Q2 (Anxiety) | 2.46 ± 1.75 | 2.92 ± 2.02 | 0.015 | |
| PHQ-Q3 and Q4 (Depression) | 1.57 ± 1.60 | 2.12 ± 1.75 | 0.001 | |
PSS: Perceived Stress Scale; PHQ: Patient Health Questionnaire; MD: Physicians; SN: Registered Nurse
p-value (Student t-test)
*In the last month, how often have you felt that you were
**Over the last two weeks, how often have you been bothered by
Table 3: Descriptive statistics of anxiety, depression, and stress using PSS and PHQ by occupation (n=569).
Overall, 49% of the respondents had an abnormal PSS-4 score and 71% had an abnormal PHQ-4 score (Figure 3). Severity levels of perceived stress and anxiety/depression among the doctors and nurses are presented in Figure 4. Females had a consistently higher elevated stress level and mood disorder (depression/anxiety) than males. About 35% of respondents had moderate to severe anxiety/depression in PHQ-4, and 11% reported moderate to severe stress in PSS-4 (Figure 4). The prevalence of stress, as well as anxiety/depression, is higher in registered nurses compared to physicians (Figures 4 and 5). There is significant gender influence in both PSS-4 and the PHQ-4 scores. The mean differences in the scores were significant among the occupation for PHQ-4 (anxiety and depression) only and not in the PSS-4 levels (Tables 2 and 3). Univariate analysis of the severity of PHQ-4 and PSSreported that gender and the location of the respondents are significantly associated with the severity of PHQ-4 and PSS-4. Female respondents, HCWs from Texas, and nurses had higher stress and anxiety/depression scores compared to males, other states of the US, and physicians. This was found to be statistically significant (Tables 4 and 5). There was a strong correlation between both overall PSS-4 scores and PHQ-4 scores (r = 0.71) as well as in individual questions (Table 6).
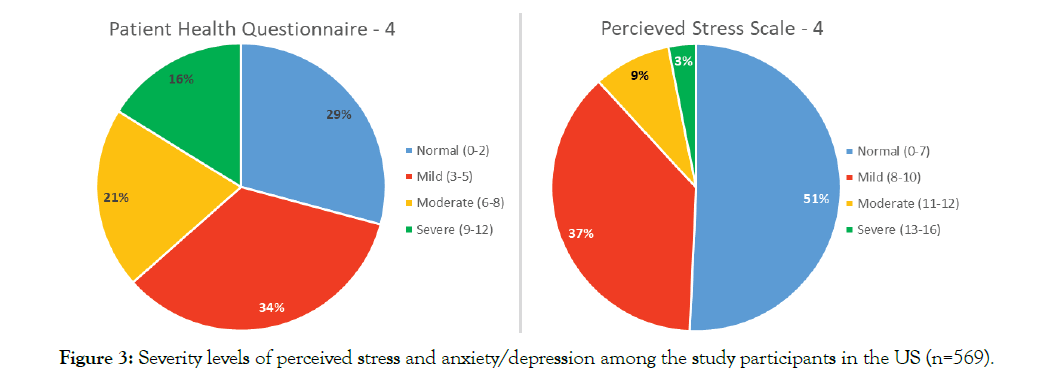
Figure 3: Severity levels of perceived stress and anxiety/depression among the study participants in the US (n=569).
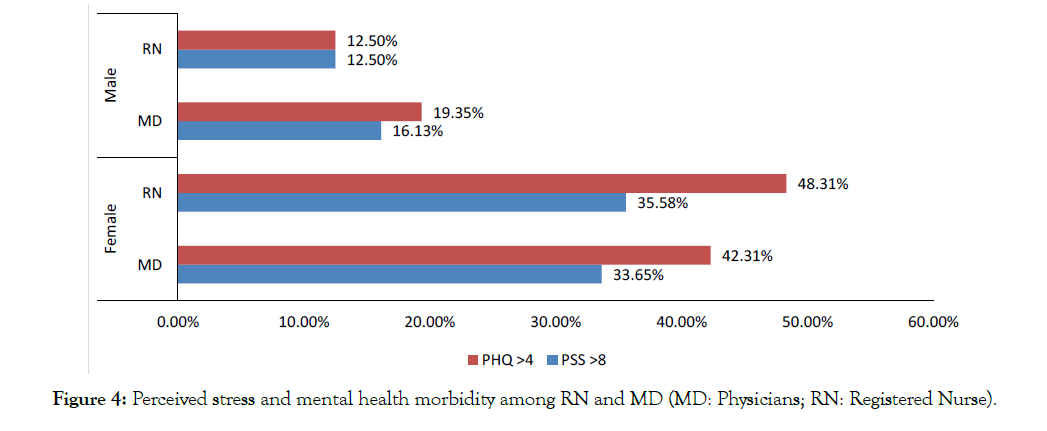
Figure 4: Perceived stress and mental health morbidity among RN and MD (MD: Physicians; RN: Registered Nurse).
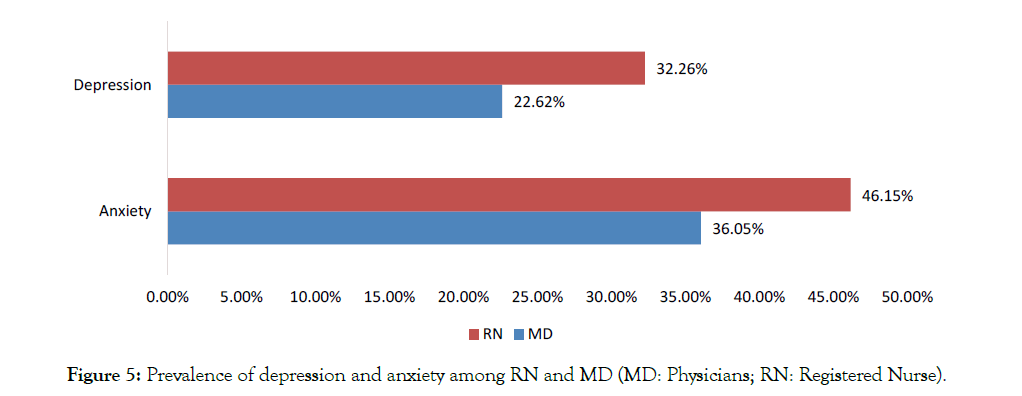
Figure 5: Prevalence of depression and anxiety among RN and MD (MD: Physicians; RN: Registered Nurse).
| Variables | PHQ - 4 (Severity) | |||||
|---|---|---|---|---|---|---|
| Normal (n=163) |
Mild (n=191) |
Moderate (n=114) |
Severe (n=19) |
Total (n=558) | p-value | |
| Gendera | 0.000 | |||||
| Female | 115 (25.2%) | 152 (33.3%) | 97 (21.3%) | 86 (18.9%) | 456 | - |
| Male | 48 (46.6%) | 35 (34.0%) | 12 (11.7%) | 3 (2.9%) | 103 | - |
| Occupationa | (n=135) | (n=149) | (n=93) | (n=73) | (n=458) | 0.066 |
| MD | 60 (34.9%) | 54 (31.4%) | 38 (22.1%) | 15 (8.7%) | 172 | - |
| RN | 75 (26.2%) | 95 (33.2%) | 55 (19.2%) | 58 (20.3%) | 286 | - |
| Locationb | (n=116) | (n=134) | (n=74) | (n=66) | (n=390) | 0.002 |
| California-A | 15 (31.3%) | 14 (29.2%) | 11 (22.9%) | 8 (16.7%) | 48 | - |
| Texas | 95 (31.6%) | 108 (35.9%) | 60 (19.9%) | 38 (12.6%) | 301 | - |
| Northeast US | 6 (14.6%) | 12 (29.3%) | 3 (7.3%) | 20 (48.8%) | 41 | - |
PHQ: Patient Health Questionnaire; MD: Physicians; SN: Registered Nurse; Percentage represents row percentage
a: Mann-Whitney U Test
b: Kruskal-Wallis Test
Table 4: Sociodemographic characteristics of study participants and the PHQ – 4 by severity.
| PSS – 4 | ||||||
|---|---|---|---|---|---|---|
| Variables | Normal (n=280) |
Mild (n=207) |
Moderate (n=48) |
Severe (n=17) |
Total (n=552) | p-value |
| Gendera | 0.000 | |||||
| Female | 214 (46.9%) | 178 (39.0%) | 39 (8.6%) | 17 (3.7%) | 456 | |
| Male | 65 (63.1%) | 23 (22.3%) | 6 (5.8%) | 0 | 103 | |
| Occupationa | (n=231) | (n=162) | (n=38) | (n=12) | (n=458) | 0.170 |
| MD | 94 (54.7%) | 57 (33.1%) | 12 (7.0%) | 4 (2.3%) | 172 | |
| RN | 137 (47.9%) | 105 (36.7%) | 26 (9.1%) | 8 (2.8%) | 286 | |
| Locationb | (n=200) | (n=149) | (n=26) | (n=11) | (n=386) | 0.003 |
| CaliforniaA | 24 (52.2%) | 16 (34.8%) | 3 (6.5%) | 3 (6.5%) | 46 | |
| Texas | 164 (54.7%) | 112 (37.3%) | 19 (6.3%) | 5 (1.7%) | 300 | |
| Northeast US | 12 (30.0%) | 21 (52.5%) | 4 (10.0%) | 3 (7.5%) | 40 | |
PSS: Perceived Stress Scale; MD: Physicians; SN: Registered Nurse; Percentage represents row percentage
a: Mann-Whitney U Test
b: Kruskal-Wallis Test
Table 5: Sociodemographic characteristics of study participants and the PSS – 4 by severity.
Our study points to a high prevalence of mental health morbidity in the form of stress as well as anxiety and depression levels, among physicians and nurses. We especially note that nurses seem to be more severely impacted and that nurses have higher levels of stress and anxiety compared to doctors.
HCWs are the first-line fighters treating patients with COVID-19. Even at baseline, healthcare workers have significant prevalence of stress burnout, anxiety and depression. In normal times, half of all physicians are experiencing significant mental stress in the form of burnout or emotional fatigue [15]. Nurses experience depressive symptoms at a rate twice as high as individuals in other professions [16]. Public health emergencies like these can affect the psychosocial wellbeing of the HCWs, and it reflects in the form of stress, anxiety, and depression. The COVID-19 pandemic has exacerbated the stress levels in healthcare workers to unprecedented levels, as evidenced by our data. The Lancet, in its recent position paper, called for high-quality data on the mental health effects of the COVID-19 pandemic across health care professionals [17]. In the US, this stress has been accentuated by lack of PPE and in many places, a surge of patients that overwhelmed the health care infrastructure. [5]. Since the start of the COVID-19 pandemic, there have been few studies that have already examined the impact of COVID-19 on mental health on HCWs. Lai et al. examined anxiety and depression by administering the 7-item Generalized Anxiety Disorder Scale (GAD-7), the 7-item Insomnia Severity Index, and the 22-item Impact of Event Scale-Revised, on 1,257 health care workers in 34 hospitals in China. They found a considerable proportion of participants reported symptoms of depression (634 [50.4%]), anxiety (560 [44.6%]), insomnia (427 [34.0%]), and distress (899 [71.5%]). Additionally, they found that nurses, women, frontline health care workers, and those working in Wuhan, China, reported more severe degrees of all measurements of mental health symptoms than other health care workers [6]. Similar findings were seen in another study from China by Que et al. who found the prevalence of symptoms of anxiety, depression, insomnia, and the overall psychological problems in healthcare workers during the COVID-19 pandemic in China to be 46.04%, 44.37%, 28.75%, and 56.59% respectively [7]. Our study’s findings are similar to these studies, including higher levels of mental health impact in women and nurses. The underlying basis for such a strong gender difference in resilience levels may be related to physiologic or psychosocial factors and may need to be better studied and understood.
In another study from China by Kang et al. who administered the PHQ-9, in the immediate wake of the viral epidemic, among 94 medical and nursing staffs working in Wuhan, 36.9% had subthreshold mental health disturbances, and the prevalence of mild-moderate and severe disturbances was 34.4%, 22.4% and 6.2% respectively [18]. This indicates a relatively lower level of stress/mental health disturbance than seen in our study. In a small single-center study from Germany, 75 nurses and 35 physicians were administered the Patient Health Questionnaire (PHQ) and the Maslach Burnout Inventory (MBI). They found that nurses working in COVID-19 wards reported higher exhaustion, depressive symptoms, and lower job fulfillment together with an overall higher stress perception at work compared to their colleagues in regular wards. Physicians working in COVID-19 wards did not report increased psychological burden [19]. A multinational study was carried out by Chew et al. in 5 major hospitals, involved in the care for COVID-19 patients, in Singapore and India using the Depression Anxiety Stress Scales (DASS-21) and the Impact of Events Scale-Revised (IES-R) instruments. They found that only 5.3% screened positive for moderate to very-severe depression, 8.7% for moderate to extremely severe anxiety, and 2.2% for moderate to extremely-severe stress [20]. These numbers are significantly lower than our study. We speculate that these may be related to differences in ethnicity, timeline of administration of the questionnaire in relationship to the COVID-19 surge, as well as population variance in stress levels and resilience in reaction to the COVID-19 pandemic. Another study from Asia in Oman surveyed 509 physicians and nurses using the PSS, GAD Scale, and World Health Organization Well-Being Index and found 26% of respondents suffered from moderate to severe anxiety [21]. HCWs who are in direct contact with COVID-19 patients are exposed to higher risk of infection [22]. Nurses are particularly vulnerable by virtue of prolonged contact time and more direct and close contact with COVID-19 patients
Another thing to note is that Lai’s paper was focused on HCWs in Wuhan, China while our paper was focused on HCWs in the USA. [6]. This would explain why the levels of stress and anxiety were higher in his study than in ours as the virus originated in China. The findings from this study can be perceived as the level of mental preparedness among the HCWs during the pandemic period. The results of the current survey are concerning and raise the need for early intervention to mitigate the immediate and longer-term consequences of the psychological wellbeing amongst the HCWs in the USA.
There are a few limitations to our study. Firstly, this is a crosssectional study carried out under an unprecedented and rapidly developing situation. Secondly, the sample representation was skewed with over 50% of the respondents from on state (Texas) and it is possible that representation that included other states or cities might have yielded a more accurate snapshot. Thirdly, this was an internet-based survey using social media, and given the anonymous nature of the survey we were unable to verify the identity or veracity of the respondents and this might have contributed to some bias in the study findings. We also did not have data on the prevalence of COVID-19 in the hospitals in which these respondents worked.
Despite this, our study provides a pivotal early glimpse of the glaring degree of mental health morbidity in health care workers due to the COVID-19 pandemic and the resultant national lockdown and points to an urgent need for more attention and intervention in this vulnerable and critical demographic.
In summary, our study is an important addition to the growing body of literature that sheds light on the growing mental health crisis amongst doctors and nurses in the US. This study suggests that the psychological wellbeing and mental health should be carefully monitored during the pandemic, and hospitals and workplaces should provide psychological support for adapting to these circumstances through targeted intervention. These efforts may need to be especially focused on females and nurses, as it was found that these populations reported higher stress, anxiety, and depression scores. A comprehensive and proactive strategy of providing mental health services at point of care on the entire healthcare workforce should be a key focus of all health care institutions, and adequate resources should be invested in this direction.
Nil
No funding was obtained to conduct the study.
Citation: Aiyer A, Surani S, Ratnani I, Surani S (2020) Mental Health Impact of COVID-19 on Healthcare Workers in the USA: A Cross-Sectional Web- Based Survey. J Depress Anxiety. 9:373. doi: 10.35248/2167-1044.20.9.373
Received: 22-Aug-2020 Accepted: 15-Sep-2020 Published: 22-Sep-2020 , DOI: 10.35248/2167-1044.20.9.373
Copyright: © 2020 Aiyer A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.