Journal of Infectious Diseases & Preventive Medicine
Open Access
ISSN: 2329-8731
ISSN: 2329-8731
Research Article - (2020)Volume 8, Issue 1
Background: Given their unpredictable nature, their direct impact on human health, as well as their broader environmental, economic, and societal impacts, emerging and reemerging infectious diseases (EIDs) require ongoing and sustained attention, funding, and response from the global community. The purpose of this paper is to understand the institutional capacities necessary to effectively respond to EIDs and highlight key strategies and potential points of intervention.
Methods: We undertook a systematic analysis of the existing literature to understand what an effective preparedness and response framework for EIDs would look like. Using the Lancet Infectious Disease Journal and PubMed, we selected all relevant results that described possible epidemic preparedness interventions or EID prevention and control strategies. We included any results published in English and within the last ten years. The different interventions and/or prevention and control strategies were grouped into larger categories to develop an effective preparedness and response framework for EIDs.
Results: An ideal emerging disease preparedness and response environment should center on collaboration between all impacted sectors and a fiscal and social commitment to strengthen the capacity on all levels of the country to respond to threats as they emerge. The potentially affected sectors are numerous, but many that have been traditionally excluded from disease preparedness activities.
Conclusion: When considering how best to participate in emerging disease response activities, it is important to identify these critical points and how interventions might work to strengthen the system in entirety. While these breakdown points are common across many settings, it is imperative that the preparedness and response activities be contextualized to specifics of the disease and setting.
Emerging infectious diseases (EID); Strategies; Points of intervention; Effective EID preparedness and response framework
CDC: Centers for Disease Control; EID: Emerging Infectious Disease; SARS: Severe Acute Respiratory Syndrome; US: United States
Emerging and reemerging Infectious Diseases (EID) have an important role in the modern world and leave long-lasting legacies. There is a long history of EIDs in humans, and they have varied greatly in type, transmission method, fatality rate, and cost. Most EIDs are zoonotic, meaning they originated in wildlife (typically in mammals), and have found their way into the human population. 70% of the 300 emerging infectious disease events between 1940 and 2004 were zoonotic in nature [1]. Furthermore, it is estimated that 25-44% of all zoonotic events have been due to viruses [1]. Viruses are particularly challenging due to their wide diversity and tendency to genetically mutate – making EID response strategies moving targets. The costs associated with EIDs are numerous and can be enumerated in many ways: in terms of lives lost (both among healthcare workers and the general population), the financial cost of response, social costs, and higher economic costs. The costs are direct in the short-term and indirect over the long-term. The global cost of the 2003 outbreak of severe acute respiratory syndrome (SARS) is estimated to be between US$13 billion and US$50 billion [2]. More recently, the centers for Diseases Control and Prevention reports that the 2014 Ebola virus outbreak response in West Africa cost roughly US$3.6 billion in total [3]. It is difficult to ascertain the true financial revenue lost as a result of an infectious disease outbreak, but history demonstrates that disease results in reductions in tourism, livestock value, exports, food production, and beyond [4]. EIDs also have devastating effects on health systems, resulting in reductions in preventive care due to reprioritization of resources toward outbreak response, declines in vaccination rates, loss of trained health care workforce members, and the additional burden of providing long-term care to survivors with chronic symptoms [4].
Due to the inherent uncertainty in predicting the next infectious disease to emerge, the global community has shifted its focus and prediction efforts away from the general question of why is this disease emerging? To the question, why is this disease emerging at this time in this location? Four domains have been identified as central to estimating EID threats: 1) genetic and biological factors of pathogens and hosts; 2) physical and environmental factors; 3) ecological factors; and 4) social, political, and economic factors [5]. First, the nature of the infectious agent and the source from where it emerges are important. This domain is difficult to ascertain due to the need for disease identification and more detailed biologic understandings. There are programs actively working on testing large populations of wildlife for the presence of pathogens. Second, the physical environment, in particular weather and climate patterns, is seasonal and subject to change as a result of global climate change. This has led to a recent expansion and movement in disease vector range. Third, the ecological factors in a setting, (i.e., land-use makeup, presence of large agricultural operations, and deforestation) are resulting in species movement and increased human-animal interactions. Finally, numerous social, political, and economic factors impact how humans interact with animals, the source of proteins, and sanitation availability. It is important to incorporate each of these factors when trying to predict the location of the next emerging disease. Some researchers believe that the reasons behind disease emergence should be disaggregated and described in more specific terms as “drivers” of disease [6,7]. Such drivers of disease include microbial adaptation and change, human susceptibility to infection, climate and weather, changing ecosystems, human demographics and behavior, economic development and land use, international travel and commerce, technology and industry, breakdown of public health measures, poverty and social inequality, war and famine, lack of political will, and intent to harm. Most of the disease outbreaks of international concern can be attributed to a single driver – lack of public health infrastructure. This has been amply evident from the Ebola outbreak in some of the Western African countries during this decade. EID prediction capabilities have improved drastically in recent years and are now monitoring additional “drivers” of disease emergence. However, there remains a challenge of establishing real-time data collection and processing at the ground level in most countries.
While there are numerous disease prediction programs and methods in use globally, there have been regions with significant histories of disease emergence that are under increased scrutiny to ensure continued political commitments and capacity building on many levels. It is important to exhaust all potential avenues to understand, predict, and respond to emerging infections. Furthermore, strategic development efforts can target specific drivers of disease emergence (i.e., public health infrastructure) through surveillance and system strengthening activities to ensure efficient and effective use of monies. There is an opportunity to learn from past outbreaks and work to develop an inclusive preparedness network with the ability to tweak and respond to any potential threat that may arise. While each emerging diseases is unique , there are some control efforts, namely communication/collaboration and preparedness steps that are universal. The universality of some preparedness activities has already been acknowledged by international agencies that have worked to strengthen the International Health Regulations (2005) to respond to emerging disease threats [8]. Furthermore, some countries have made significant progress towards the achievement of the International Health Regulations and the establishment of strong disease surveillance and response plans. There is still an immense opportunity to assess capacities, develop policies, and plans to fill gaps and improve the operational quality of these systems around the world. Given their unpredictable nature, their direct impact on human health, as well as their wider environmental, economic, and societal impacts, EIDs require ongoing and sustained attention, funding, and response from the global community. The purpose of this paper is to understand the institutional capacities necessary to effectively respond to EIDs and highlight key strategies and potential points of intervention. We undertook a review of the literature to understand what an effective preparedness and response framework for EIDs would look like.
We undertook a systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [9].
Search eligibility and criteria
The search was conducted through the two databases, PubMed and The Lancet Infectious Disease Journal. The search was limited to all resources published in English and within the last ten years from August 1, 2009, to August 1, 2019. Article types accepted in the search included systematic reviews, review, observational studies, meta-analysis, journal article, editorial, comparative study, comment, case report, case study, and correspondences. We applied the Boolean research method. For consistency, we employed the same set of search terms on all databases. The search terms or phrases used were [emerging infectious disease” OR “EID response framework” AND “epidemic response” AND “interventions” OR “prevention and control strategies” OR “epidemic preparedness”]. Only studies discussing possible epidemic preparedness interventions and/or EID prevention and control strategies using a case or country context were included. The search protocol for this review is provided as supporting information (Additional File 1) [10-41].
Data collection and synthesis
A total of 264 records were identified using the two databases and the search criteria (Figure 1).
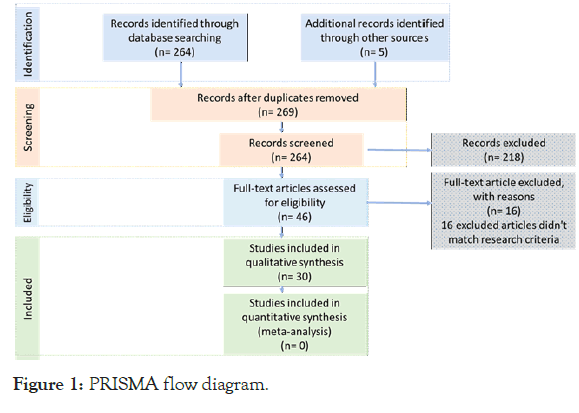
Figure 1. PRISMA flow diagram.
Of these 264 results, only 46 of the results had titles/abstracts that matched the search criteria. After a full-text analysis of the 46 results, 16 were excluded for not fitting the search criteria. Finally, 30 studies were included in this systematic review. The studies were reviewed, and a list of EID preparedness interventions and prevention and control strategies were developed. Individually, the studies were assessed for risk of bias. Any studies considered biased will be excluded from the review.
The data shows that an ideal EID preparedness and response plan must incorporate interventions and strategies over a variety of categories (Table 1).
| No | Study (Author, Year) | EID surveillance and monitoring systems-tallored survellance strategies to prevent and mitigate damage | Multi-stakeholder response focusing on healthcare system strengthening. Including sharing of resources between global, national, and local levels to improve care, EID assessment, and response time | Integration of EID diagnostics into EID preventio and control plans including strengthening vaccination/vector control treatment strategies | Pharmaceutical and non-pharmaceutical preventative measures | Improving communication strategies between government Institutions and the public to improve feedback and regular monitoring especially risk based communication strategies including risk communication interventions | Strengthening existing public health institution capabilitoies to better handle surges including influenza drils, excercises and simulations for HWCs | Social, behavior, and culture change interventions including in social protection programs | Strengthening research and evaluation |
|---|---|---|---|---|---|---|---|---|---|
| 16 | Andrew et al.(2017) | * | * | ||||||
| 37 | Bell et al.(2016) | * | * | ||||||
| 35 | Cordova-Villalobos et al.(2017) | * | * | * | * | * | |||
| 17 | Dhama et al.(2015) | * | |||||||
| 31 | Gyawali et al.(2016) | * | |||||||
| 20 | Hamel et al.(2015) | * | |||||||
| 15 | Ho et al. (2017) | * | * | ||||||
| 36 | Hsu et al.(2017) | * | |||||||
| 18 | Kebede et al.(2010) | * | * | ||||||
| 2 | Kelly-Cirini et al.(2019) | * | |||||||
| 29 | Khalil et al.(2019) | * | |||||||
| 25 | Kim et al.(2015) | * | * | * | |||||
| 28 | King et al.(2017) | * | |||||||
| 40 | Matua et.al(2015) | * | |||||||
| 26 | Periman et al.(2019) | * | |||||||
| 23 | Purohit et al.(2017) | * | * | ||||||
| 38 | Rabkin et al.(2015) | * | * | ||||||
| 27 | Randremanana et al.(2017) | * | * | * | |||||
| 41 | Reeves et al.(2014) | * | |||||||
| 12 | Sambala et al.(2017) | * | * | * | * | ||||
| 34 | Schuchat et al.(2011) | * | * | ||||||
| 19 | Shirley et al.(2013) | * | * | * | * | ||||
| 21 | Sigmundsdottir et al.(2010) | * | |||||||
| 32 | Singapore Zika Study Group (2017) | * | * | ||||||
| 33 | SteelFidher et al.(2012) | * | |||||||
| 14 | Tambo et al. (2016) | * | * | * | * | * | |||
| 30 | Tay et al. (2010) | * | * | ||||||
| 13 | Thiam et al.(2015) | * | * | ||||||
| 11 | Veldhuis et al.(2019) | * | |||||||
| 39 | Yen et al.(2014) | * | * |
Table 1: EID study table (Domains of EID response strategies identified).
Considering that this literature review only included possible epidemic preparedness interventions and/or EID prevention and control strategies using a case or country context, the included studies were found to present no risk of bias. The data highlights that an ideal emerging disease preparedness and response environment should center on collaboration between all impacted sectors and a fiscal and social commitment to strengthen the capacity on all levels of the country to respond to threats as they emerge. A truly comprehensive EID response system requires system-wide coordination, ongoing surveillance systems throughout the world, strengthening healthcare resources (personnel, medications, facilities, etc.), social, behavior, and change interventions, and the integration of appropriate diagnostics into prevention and control plans [10-12]. Ten different results (33.3%) stressed the importance of tailored EID surveillance strategy that would prevent and mitigate EID outbreaks [13-23]. Strengthening the collaboration between multiple stakeholders to improve existing healthcare systems and encourage the sharing of resources to improve EID response and help mitigate the damage was outlined in 12 results. Social, behavior, and change interventions (including educational interventions for the public) and the integration of appropriate diagnostics into prevention and control plans were highlighted as significant factors to an ideal EID preparedness and response plan in 20 studies. The potentially impacted sectors are numerous, but many that have been traditionally excluded from disease preparedness activities (Figure 2).
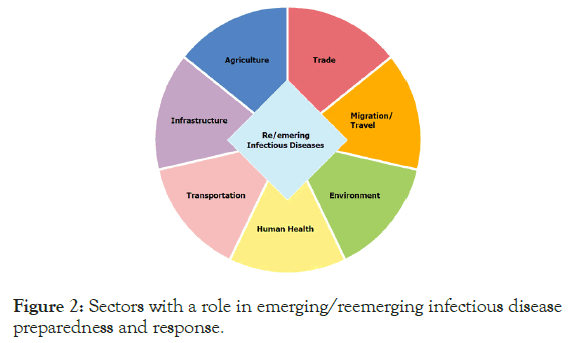
Figure 2. Sectors with a role in emerging/reemerging infectious disease preparedness and response.
The multi-sectoral approach is further expanded upon in the One Health framework and highlights the importance of the interconnectivity between numerous sectors integral to disease response [18,24-26]. The fact that we do not know with any certainty where, when, and how a disease will emerge is the critical challenge. Funding for prevention and mitigation efforts are limited due to the lack of obvious return on investment and the uncertainty associated with emerging diseases. Due to globalization and travel patterns around the world, EIDs are a legitimate threat for all people around the world, even for those not living in areas identified as hot-spots for diseases emergence. The proverty burden in many EID hotspot countries puts specific populations at an additional disadvantage as systems and infrastructure are not adequate to respond to a novel infectious Diseases .Both the Ebola and Zika virus outbreak instances demonstrate the significant long-term health impacts that can result from a little-understood pathogen. While there have been more outbreaks of Ebola in history than Zika, the natural host of the virus is yet to be fully ascertained. Similarly, studies amongst survivors of Ebola in West Africa are showing residual viral presence in bodily fluids for up to 12 months after recovery [27].These knowledge gaps make a comprehensive response difficult, and there are no curative medications or widelyapplied vaccinations available. The case of Zika is even less clear. Health agencies continue to update recommendations due to the changing understanding of the virus. The temporality of infectious diseases results in extreme highs in interest (during the large outbreak) and significant drops in interest (after the deaths stop) leaving the impacted community to address indirect and long-term sequelae independently.
Our proposed overall approach to EIDs centers on the emergency response cycle. The phases of the emergency response cycle mitigation, prevention, response and recovery. Each component of the cycle is a necessary part of the overall response; they are displayed in sequence but can occur concurrently or in quick succession depending on the scope and type of emergent risk. The goal of each component of the cycle is unique but complementary (Table 2).
| Cycle phase | Goal | Examples |
|---|---|---|
| Mitigation | Minimizing the effects of the disaster | Building codes and zoning, vulnerability analyses and public education |
| Preparation | Planning how to respond | Preparedness planning, emergency exercises/training, warning systems |
| Response | Efforts to minimize the hazards created by a disaster | Search and rescue and emergency relief |
| Recovery | Return the community to normalcy | Temporary housing, medical care and grants for recovery activities |
Table 2: The emergency response cycle.
The emergency response cycle works to guide a response, and there are critical points along the cycle where interventions can strengthen the entirety of the cycle. When considering how best to participate in emerging disease response activities, it is important to identify these critical points and how interventions might work to strengthen the system in its entirety. While these breakdown points are common across many settings, preparedness and response activities must be contextualized to specifics of the disease and setting Communication and capacity are constant across the cycle and require constant engagement and learning [10,28-31]. Communication strategies should also be tailored to fit local context and cultural settings [32]. If there are successful interventions at the beginning of the cycle, subsequent stages are more effective and efficient.
In order to expedite implementation and ensure the effectiveness of interventions, surveillance and response systems can be built on-top-of existing platforms or grown out of successful programs. The same can work in reverse - a functional surveillance system can be applied to a multitude of health issues to facilitate ongoing monitoring and community engagement. The harmonization of any new systems can help to ensure sustainability and uptake of novel approaches.
In light of the interest in EID response and preparedness, there have been novel approaches deployed for community use. Some of the previously identified applications of technology and system strengthening are provided in Table 3.
| Area of response | Example approaches |
|---|---|
| Surveillance/vector control | App to report potential sources of mosquito breeding for community use |
| Apps for community health workers to report potential illness | |
| Systems for laboratories and doctors to report results up the chain of command | |
| Systems for veterinarians to report large animal illnesses (and in their associated human population) | |
| Behavior change communications | App to provide educational information regarding disease identification and prevention for general public |
| Continued learning modules for trained healthcare workers to receive disease recommendation updates | |
| Health systems strengthening | Establishment of public-private coordination system to keep up-to-date info available for decision making |
| Capacity building for the implementation of new technologies (diagnostic tools, mosquito control efforts, vaccine deployments, personal protective equipment) | |
| Creation of real-time maps of available services and disease cases | |
| Establishment of ongoing monitoring system for Zika pregnancies and children with microcephaly |
Table 3: Novel approaches for addressing emerging and reemerging infectious diseases.
The range of technological applications is vast, but each was created for a particular context and outbreak. It is important to ensure that any innovations are realistic for the setting, and the technology works to fill the identified gap in capacity. Additionally, it will be important to understand how each of the relevant sectors can address issues on the system, community, provider, family, and individual levels. To identify some of these potential breakdown points and how-to response to identified needs, a more detailed description of EID response activities and required inputs is provided in Figure 3. This figure outlines the progression of an outbreak from initial consideration and planning stages to postemergency responses.
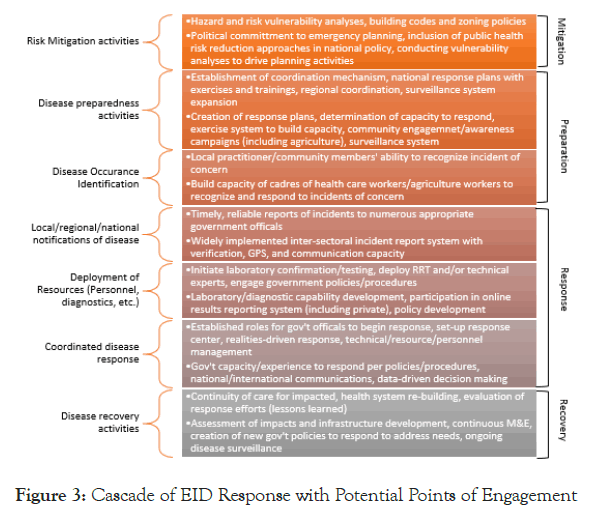
Figure 3. Cascade of EID Response with Potential Points of Engagement.
There were clear strengths and limitations to our review. Strength of the review was that the use of the specific eligibility criteria and search process made narrowing down relevant articles efficient and straightforward. A limitation of the review was that the search could have been more comprehensive with the inclusion of other databases. However, for the two databases used – scaling the search to the past ten years provided a significant amount of relevant search results.
Emerging infectious diseases represent an ongoing challenge to the global community and bring with them the ongoing threat of grave health, environmental, economic, and societal impacts. An ideal emerging disease preparedness and response environment should center on collaboration between all impacted sectors, as well as fiscal and social commitment to strengthen the capacity of countries and communities to respond to threats as they emerge. When considering how best to participate in emerging disease response activities, it is important to identify these critical points and how interventions might work to strengthen the system in entirety. While these breakdown points are common across many settings, it is imperative that the preparedness and response activities be contextualized to specifics of the disease and setting.
HJM and NK conceptualized and designed the project. HJM performed the analysis wrote the original draft of the manuscript. CL and NK were major contributors in reviewing and revising the manuscript. SJ conducted the literature review. All authors read and approved the final manuscript.
Citation: Al Mossawi HJ, Kak N, Longacre C, Joshi S (2020) Key Strategies to Address Emerging and Reemerging Infectious Diseases: A Systematic Analysis. J Infect Dis Preve Med. 8:194. DOI:10.35248/2329-8731.20.08.194.
Received: 14-Feb-2020 Accepted: 29-Feb-2020 Published: 07-Mar-2020 , DOI: 10.35248/2329-8731.20.08.194
Copyright: © 2020 Al Mossawi HJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.