Clinical & Experimental Cardiology
Open Access
ISSN: 2155-9880
ISSN: 2155-9880
Mini Review - (2025)Volume 16, Issue 6
One significant way to drain fluid from the pericardial cavity is via an emergency pericardiocentesis. It is typically administered to patients suffering from extreme pericardial effusion, which can cause instability in their body’s blood flow. Pericardiocentesis, guided by ultrasound, is currently considered the gold standard for pericardial fluid aspiration. Traditionally, it relied on echocardiography using a low-frequency transducer, but the lack of real-time needle trajectory visualization sometimes led to complications. To address this, we are introducing a new technical approach in this brief review. We’ll be discussing an ultrasound-guided pericardiocentesis method that utilizes a highfrequency transducer, using an in-plane technique with a lateral-to-medial approach from the right parasternal. The suggested technique involves using a high-frequency ultrasound probe on the right parasternal region. This allows for immediate visualization of the needle path and neighboring anatomical structures like the myocardium, pericardial effusion, sternum and right internal thoracic vessels. The needle is inserted from lateral to medial at a 45-degree angle, ensuring a safe path to the pericardial effusion between the pleural sliding endpoint and the right internal thoracic vessels. The described method enables real-time visualization of the needle and its surroundings, potentially enhancing precision and preventing complications. It might ease access for both emergency pericardiocentesis and loculated pericardial effusion treatment surrounding the right atrium. Nonetheless, further research with significant patient populations is necessary.
Pericardiocentesis; Ultrasound-guided pericardiocentesis; High-frequency probe; In-plane technique; Lateral-to-medial approach; Right parasternal access
PE: Pericardial Effusion; ITVs: Internal Thoracic Vessels; CT: Computed Tomography
Patients experiencing hemodynamic compromise due to substantial pericardial effusion can be saved by performing an emergency pericardiocentesis, which involves aspirating fluid from the pericardial cavity [1]. These days, most of these pericardiocentesis procedures use ultrasound-guided techniques. The correct entry site and diagnosis of pericardial effusion have traditionally been achieved using echocardiography and a lowfrequency transducer [2-4]. However, some new, unconventional methods for pericardiocentesis have been documented, such as the use of high-frequency transducer-guided pericardiocentesis with echocardiography [5-9].
In this paper, we present a mini review on a novel proposed technique for ultrasound-guided pericardiocentesis using right parasternal access and a high-frequency probe [9].
Echocardiography-guided pericardiocentesis, developed in the 1970's, is now considered the gold standard due to its lower risk of complications [4]. But, because to in experience with point-of-care ultrasound, numerous institutions continue to employ blind subxiphoid pericardiocentesis. An estimated 6% of patients may die as a result of this procedure, while the morbidity rate is around 20% [2]. In comparison, echo-guided pericardiocentesis has significantly fewer complications, the incidence of minor and major complications is 0.420% and 0.339%, respectively [4].
Generally, CT-guided pericardiocentesis is carried out on patients who have impaired acoustic apertures and complex, regularly loculated pericardial effusions [10].
Conventional methods often use low-frequency probes to ensure needle insertion towards areas with the most fluid accumulation and to prevent the needle’s path from intersecting with critical structures [2-4].
Several observational studies have shown that the parasternal method is more effective than the subxiphoid method for accessing the pericardial space. This is due to its more direct, safer, and superficial nature [1,4,8].
For traditional parasternal access, the needle is inserted right next to the sternum to avoid damaging the ITVs, located about 1 cm laterally [11]. However, this technique can lead to complications arising from the inability to track the needle’s path and its proximity to surrounding anatomical structures.
In ultrasound-guided pericardiocentesis, a number of recent studies have suggested using a high-frequency probe [5-9]. There has been no presentation of these applications as lateral-tomedial ways when approached from the right parasternal position, even though case reports have recorded parasternal, inplane and real-time procedures [7,8]. A small group of patients was studied by Osman, et al. [6] to show that a high-frequency probe in a left parasternal in-plane medial-to-lateral approach reduced procedure time, had no problems and resulted in a 100% success rate. We detailed a novel technical method for doing a successful, complication-free emergency pericardiocentesis utilizing a high-frequency probe and right parasternal access in a recent case report [9].
Technique description
Pre-procedure: An initial evaluation was conducted utilizing a cardiac phased array probe to determine the size and location of the pericardial effusion. After that, in order to have an excellent view, a high-frequency probe was placed transversely in the right parasternal region. The ideal viewpoint which revealed the pericardium in close proximity to the chest wall, could be identified and adjusted according to this location. The probe revealed the right atrium, pleural sliding, sternum, pericardial effusion and Internal Thoracic Veins (ITVs on the right side. Measurements of the effusion's diameter and the distance between the pericardial sac and the skin were then taken (Figure 1). The technique may be safely performed if the diameter of the Pericardial Effusion (PE and the distance between the right Internal Thoracic Vasculature (ITVs and pleural sliding endpoints were greater than 1 cm in the right parasternal window [9].
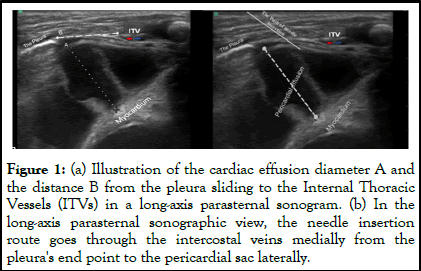
Figure 1: (a) Illustration of the cardiac effusion diameter A and the distance B from the pleura sliding to the Internal Thoracic Vessels (ITVs) in a long-axis parasternal sonogram. (b) In the long-axis parasternal sonographic view, the needle insertion route goes through the intercostal veins medially from the pleura's end point to the pericardial sac laterally.
Procedure: Each step must be executed under antiseptic conditions. The patient remained supine during the procedure as the ultrasound device was situated to her left. After adjusting the ultrasound settings appropriately, the operator stood on the right to get a clear view of the ultrasound screen.
A high-frequency ultrasound probe was transversely positioned in the right parasternal intercostal space, where the preprocedure scan had shown the clearest image.
The environment was later defined by its structures. The optimal drainage penetration path was then determined. Following this, the needle was skillfully moved at a 45-degree angle from the right hand towards the media while maintaining plane alignment. During this procedure, the needle, which navigates medially through the PE between the right ITVs and the lateral end point of plural sliding, is monitored in real-time. Confirmation of successful entry into the pericardial space is obtained by aspirating the pericardial cavity once the catheter is in place [9].
The novel in-plane technique, which involves a lateral-to-medial approach via right parasternal access for ultrasound-guided emergency pericardiocentesis, presents several potential benefits. This technique is carried out using a high-frequency probe.
Using the in-plane technique, particularly the lateral-to-medial approach, improves the live visualization of the needle path and surrounding anatomical features. This could shorten the procedure time and reduce the risk of complications [6].
The in-plane method, which utilizes right parasternal access, could be a practical alternative for emergency pericardiocentesis, this approach can also manage localized effusions or hematomas that develop around the right atrium and are difficult to reach through conventional methods [9]. These cases might otherwise require surgical intervention [10].
Conventional ultrasound-guided pericardiocentesis presents significant challenges. One of these is the difficulty in obtaining a clear, real-time view of the needle’s complete path using a lowfrequency transducer [2-4]. This can potentially risk damaging nearby vital organs. However, recent advancements in real-time visualization have introduced new techniques and approaches, such as the use of high-frequency probes [5-9].
High-frequency probe of ultrasound is extensively utilized in percutaneous thoracic interventions [12]. It enhances spatial resolution, reduces artifacts and helps clinicians avoid damage to crucial anatomical structures [13].
We are focusing on recently introduced method, including ultrasound-guided pericardiocentesis using a high-frequency probe through right parasternal access, conducted from the lateral to the medial direction [9]. That may potentially a beneficial to be one of safe and feasible choice for emergency pericardiocentesis when other approaches is infeasible especially for loculated effusions that formed around right atrium.
This technique was initially described and successfully applied in a clinical case study that was infant with cardiac tamponade. It was confirmed that this was the most practical, convenient and optimal site for use in the reported case [9].
The right parasternal approach has advantages; the pericardial space around the right atrium is widely known as the primary site for the most significant accumulation of PEs throughout the heart’s cycle. This can be primarily attributed to the low pressures in the right atrium and the influence of gravity [14-17]. As a result, it is easier for pericardial fluid to accumulate there. When lying down, the effusion has a tendency to collect surrounding the right atrium posteriorly, which is most noticeable in this position. As a result, the effusions that surround the atrium expands in diameter, becoming the main area where fluid accumulates the most. Having access to the fluid collection around the right atrium via the right parasternal approach may be a more easy and feasible option in comparison to other methods [9].
Postoperative complications often include hematomas and loculated PE effusions, as reported in studies [10,18]. Usually, hematomas causing specific symptoms are commonly located at the front and sides of the right atrial free wall. Due to direct access to the pericardial space surrounding the right atrium is possible through the right parasternal approach [9]. It is indicated that the suggested technical approach may offer a practical and effective way to access loculated effusions or hematomas that cannot be reached by traditional methods and necessitate intervention by surgery or CT-guided pericardiocentesis [9,10,18].
The in-plane technique can only be applied when the parasternal window effusion diameter surpasses 1 cm [9,19]. The recommended procedure involves moving the needle laterally from the end point of pleural sliding to the medial region of the right ITVs [9]. By doing so, the needle can be guided safely into the pericardial area without endangering any neighboring structures or causing any problems. For the procedure to be executed safely there must be a sufficient gap between them, preferably at least 1 centimeter. This rare procedure holds a certain similarity to more prevalent ones, such as ultrasoundguided peripheral and central vascular access, due to the proficiency of many emergency physicians in applying the inplane technique of the linear array probe for needle guidance [9]. The technique thus described holds promise for physicians who specialize in emergency and critical care.
Additional research and constraints
Ensuring patient safety and positive results requires the operator to be proficient and experienced in ultrasound-guided procedures. Although many emergency clinicians frequently employ these procedures, it is not a universal practice [9]. Thoracic emphysema can also impair image quality. In cases of cardiac arrest, the subxiphoid approach is significantly more effective than the parasternal approach [6,10,11]. Nevertheless, this technical approach has only been applied to a single clinical case, so it is essential to validate its effectiveness across a broader population.
Future studies should assess if the sonographic view from the right parasternal window is suitable for adults and older children. Additionally, if this suggested method proves superior to surgical or CT-guided pericardiocentesis procedures, it could be clinically applicable for local effusions or hematomas around the atrium.
This review has outlined a new technique used in emergency pericardiocentesis procedures when other methods may not be feasible. Real-time visualization can improve needle placement accuracy and reduce the risk of complications. This technique might be used for pericardiocentesis, loculated pericardial effusion, or a hematoma that formed around the right atrium. Still, more research and clinical experience are needed to confirm its effectiveness and potential benefits.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Mohammed NA, Al-Zubairi TA (2025) Innovative Approach: Ultrasound-Guided Pericardiocentesis Performed via the Right Parasternal Using a Novel Approach. J Clin Exp Cardiolog. 15:954.
Received: 07-Mar-2024, Manuscript No. JCEC-24-30048; Editor assigned: 08-Mar-2024, Pre QC No. JCEC-24-30048 (PQ); Reviewed: 22-Mar-2024, QC No. JCEC-24-30048; Revised: 01-Jun-2025, Manuscript No. JCEC-24-30048 (R); Published: 08-Jun-2025 , DOI: 10.35248/2155-9880.25.16.954
Copyright: © 2025 Mohammed NA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.